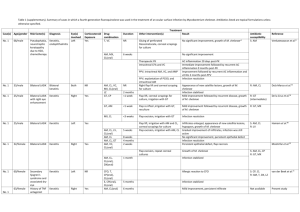
M. chelonae
advertisement

內科專科醫師 職業醫學專科醫師 胸腔暨重症醫學專科醫師 結核病專科醫師 簡歷 索任 現任 2005/5 2006/120021994- 社團法人中華民國防癆協會第一胸腔病防治所所長 行政院衛生署傳染病防治諮詢委員會結核病防治組召集人 中華民國職業病醫學會理事 台灣結核病醫學會理事 曾任 2002/7 – 2005/3 2002/2 – 2002/7 2001/8 – 2002/1 1999/7 – 2001/8 1997/1 – 1999/6 1989/3 – 1997/1 1984/4 – 1989/3 1983/7 – 1984/4 1979/7 – 1983/7 行政院衛生署桃園醫院內科師一級主治醫師 行政院衛生署胸腔病院代理院長 行政院衛生署慢性病防治局代理局長 行政院衛生署慢性病防治局副局長 台北縣慢性病防治所醫師 台灣省慢性病防治局技正兼主任 台灣省防癆局技正兼主任 台灣省防癆局主治醫師 台灣省防癆局住院醫師及總住院醫師 1979 台灣大學 醫學院 醫學系 Tuberculosis and diseases caused by nontuberculosis mycobacteria in Taiwan: Clinical aspect 社團法人 中華民國防癆協會 第一胸腔病防治所 索 任 醫 師 solo@tstb.org http://www.tb.org.tw 台北市民權西路104號2樓 The Genus Mycobacterium Gram-positive, acid-fast, non-spore-forming, straight or slightly curved rods (0.2~0.6 1.0~10m) coccobacillary, filamentous, branched Pigment in dark or after exposure to light Aerobic or microaerophilic Subdivision: rapid growers, slow growers Large amounts of lipid in cell walls: mycolic acids Typical species: Mycobacterium tuberculosis Classification of mycobacterial species commonly cause human disease Mycobacterium tuberculosis complex M. leprae Slowly growing mycobacteria Photochromogens (Runyon group I) Scotochromogens (Runyon group II) Nonchromogens (Runyon group III) Rapidly growing mycobacteria (Runyon group IV) Mycobacterium tuberculosis complex M. tuberculosis M. bovis M. africanum M. microti M. canetti M. tb M. kansasii 結核病 – 被遺忘了的瘟疫 Tuberculosis 1992 傳染源 Latent infection vs. disease 感染 發病 感染:會呼吸的人都是結核病的易感宿主 發病:新近感染及免疫力減弱為主要危險因子 如何檢查結核菌感染 結核菌素測驗 (不夠精準的檢查) 結核菌素 tuberculin (Koch,1890) Mantoux test (1907) 干擾 – 宿主的抵抗力, 卡介苗或其他非結核分枝桿菌(NTM)感染, 測驗技術和判讀經驗 怎樣檢查肺結核病? 胸部X光檢查 驗痰 TB TB 何時了 潛伏感染 發病 大女兒 69-4-3 F 大兒子 67-11-11 M 82-3-13 “5” M+C+ 父 39-10-15 M 75-4-7 “5” M+C+ HS 抗藥 76-10 完治 95-2-23 “5” M+ ST N/A 小女兒 71-3-19 F 82-12 完治 88-6-28 “3” M+C+ HS 抗藥 89-4 完治 結核病 Class I Exposure Class II Class III Disease Infectious 83-4-11 Latent TB Infection Non Infectious 81-3-27 Death TB TB 何時了 – 診斷延遲 93/10/12 94/11/30 TB TB 何時了 – 診斷延遲 94/02/23 95/01/12 TB TB 何時了 – 不規則治療 910529 940909 傳染 transmission 化學治療 Chemotherapy 結核病防治 結核病的傳染期 = 病人延遲 + 醫師延遲 +病人治療管理不當 Prophylactic treatment 預防性 治療 Preventive 醫師延誤 病人延誤 Doctor’s delay Patient’s delay therapy 傳染性 結核病 接觸 Exposure 結核潛伏 感染 Subclinical infection Infectious TB 死亡 非傳染性 結核病 Non-Infectious TB BCG vaccination 卡介苗 Source: Interventions for Tuberculosis Control and Elimination, IUATLD 2002 Death 結核病防治 三個基本動作 盡早找出結核病人 盡速治癒每個找出來的病人 不讓結核菌產生抗藥性 結核菌持續挑釁 衛生體系重組 (Health reform) 抗藥性結核菌 HIV/AIDS 貧窮 Mycobacteria other than M. tuberculosis and M. leprae Nontuberculous mycobacteria (NTM) Mycobacteria other than tuberculosis (MOTT) Environmental mycobacteria Opportunistic mycobacteria Atypical mycobacteria Anonymous mycobacteria Unclassified mycobacteria NTM of Clinical Significance Runyon classification and major species I. Photochromogens M. kansasii, M. marinum, M. simiae, M. asiaticum II. Scotochromogens M. gordonae, M. scrofulaceum, M. szulgai, M. flavescens III. Nonchromogens MAC (M. avium, M. intracellulare), M. terrae complex, M. ulcerans, M. xenopi, M. malmoense, M. haemophilum, M. genavense, M. gastri, M. celatum IV. Rapid growers M. fortuitum, M. chelonae, M. abscessus, M. phlei, M. vaccae I. Photochromogen M. marimun M. kansasii II. Scotochromogen M. gordonae M. szulgai M. scrofulaceum III. Nonchromogen M. intracellulare M. avium M. xenopi IV. Rapid grower M. chelonae M. abscessus M. fortuitum Historical Perspective and Epidemiology of the NTM (I) Organism First human Source (s) case Animal reservoir (s) Rapid growers MAC 1930s 1943 Soil, water Soil, water M. ulcerans M. marinum M. scrofulaceum M. kansasii M. xenopi M. simiae 1948 1951 1950s 1953 1965 1965 Unknown Salt, fresh water Lake, river water Water Hot water tank, taps Water (rare) Cats, cattle, dogs… Birds, cats, swine dogs, horses Cats Fish Cattle, swine Cattle, deer, swine Cats, cattle, swine Monkeys Emerging Infections I, 1998 Geographic Distribution Organism Distribution M. malmoense, M. xenopi Coal-mining regions, northern Europe Japan, Australia Southwestern US, Israel, Cuba Africa, Australia, southeast Asia Southern, central US New York City M. shimoidei M. simiae M. ulcerans M. kansasii M. haemophilum Epidemiology of NTM Environmental Sources Most NTM have been recovered from water and soil Mycobacteria Sources of infection MAC, M. kansasii Tap water; airborne M. marinum Salt, fresh water, fish tanks, swimming pool M. xenopi Hot water; hospital heating tank (43-45oC) M. simiae Tap water M. genavense Dogs, pet bird (psittacine birds) Rapid growers Tap or distilled water, dialysate; nosocomial Environmental sources of infection are likely: M. ulcerans, M. haemophilum, M. szulgai, M. celatum, M. genavense, M. conspicumm The most important nontuberculous mycobacteria Harrisons principles of internal medicine, 15th ed. -1 The most important nontuberculous mycobacteria Harrisons principles of internal medicine, 15th ed. -2 Principal Types of Mycobacterial Disease in Man and the Causative Agents (1) Disease Usual Uncommon Tuberculosis M. tuberculosis M. bovis M. africanum Leprosy M. leprae Lymphadenopathy M. avium complex M. scrofulaceum Many other species Post-traumatic abscesses M. Chelonae M. fortuitum M. terrae M. flavescense Swimming pool granuloma M. marinum Buruli ulcer M. ulcerans Other skin lesions M. haemophilum M. kansasii M. shinshuenses Principal Types of Mycobacterial Disease in Man and the Causative Agents (2) Disease Usual Uncommon Opportunistic pulmonary disease M. avium complex M. kansasii M. xenopi M. malmoenses M. scrofulaceum M. asiaticum M. celatum M. gordonae M. simiae M. Szulgai M. chelonae M. fortuitum HIV-associated M. avium complex M. genavense Non-HIV-associated M. avium complex M. chelonae Disseminated Disease Diseases Caused by Nontuberculous Mycobacteria Most disease: in immunosuppressed patients Source of infection: environment Person-to-person transmission: not proved Culture contamination: environmental saprophytes Colonization without producing overt disease Assessing clinical significance of isolates Clinical syndromes NTM infection of the lung in HIV- patients often occur in the context of preexisting lung disease, especially: chronic obstructive pulmonary disease (COPD), bronchiectasis, pneumoconiosis, cystic fibrosis, and previous tuberculosis AJRCCM 1997; 156:S1-S19. Diagnosis of NTM pulmonary disease Clinical criteria Compatible signs/symptoms (cough, fatigue most common; fever, weight loss, hemoptysis, dyspnea) with documented deterioration in clinical status of underlying disease, and Reasonable exclusion of other diseases (eg. TB, cancer, histoplasmosis) or adequate treatment of other conditions with deterioration in clinical signs/symptoms AJRCCM 1997; 156:S1-S19. Diagnosis of NTM pulmonary disease Radiographic Criteria Chest X-ray Evidence of progression if baseline film > 1 year old Infiltrates with or without nodules (persistent 2 months or progressive) Cavitation Multiple nodules as a solitary finding HRCT Multiple small nodules Multifocal bronchiectasis with or without small lung nodules AJRCCM 1997; 156:S1-S19. Diagnosis of NTM pulmonary disease Bacteriologic Criteria At least 3 sputum/bronchial wash speciemens within previous year Three positive cultures with negative AFB smears, or Two positive cultures and one positive AFB smear, OR Single available bronchial wash and inability to obtain sputum sample Positive culture with 2+, 3+, or 4+ growth, or Positive culture with 2+, 3+, or 4+ AFB smear OR Tissue biopsy, any of following Any growth from bronchopulmonary tissue biopsy Granuloma and/or AFB on lung biopsy with at least one positive cultures from sputum or bronchial wash Any growth from usually sterile extrapulmonary AJRCCM 1997; 156:S1-S19. Diagnosis of NTM pulmonary disease To conclusively diagnose NTM pulmonary disease, all three criteria – clinical, radiographic, and bacteriologic – must be satisfied Culture positive with 1+ growth is sufficient if HIV-positive with CD4<200 (excluding MAC) and in patients with general severe immune suppression, leukemia, lymphoma, organ transplantation, or other immunosuppressive therapy AJRCCM 1997; 156:S1-S19. Diagnosis of NTM pulmonary disease Comment The criteria fit best with M. avium complex M. abscessus M. kansasii At least three respiratory samples should be evaluated Other reasonable causes should be excluded Expert consultation AJRCCM 1997; 156:S1-S19. M. kansasii pneumonia a b c Chest radiographs of a patient with severe emphysema and bilateral upper lobe disease caused by Mycobacterium kansasii. (a) Before treatment. (b) After 9 months of antimycobacterial treatment. (c) 2 months after the end of treatment. M. avium complex pneumonia 54 year-old woman Fever, cough, weight loss, neck LAP VATS-AFB (+) Blood, pleural fluid (+) for M. avium complex MAC pneumonia (MACxIII, sputum) MAC pneumonia 46/M, AML, M2, post C/T; Pulmonary M. avium Infection Plus PCP; (CIP+EMB+RIF+Baktar) 8/03/2002 18/03/2002 (4017766) AIDS, MAC 28/F, cystic bronchiectasis M. abscessus M. Chelonae 64 year-old woman Destructive lung M. chelonae Clarithromycin + ciprofloxacin Persistent infection Disseminated MAC infection MAC tenosynovitis 75/M, CRI, herb Fever, right hand lesion for 2 weeks WBC, 6300; CRP, 1.33 Tenosynovitis EMB+CIP+CLA MAC lymphadenitis 45 year-old female Productive cough for 3 weeks Neck LAP P. marneffei pneumonia MAC lymphadenitis M. marinum infection (Fish-tank granuloma) A red-violet, verrucous plaque on the dorsum of the thumb of a fish-tank hobbyist arose at the site of an abrasion. Harrisons principles of internal medicine, 15th ed. M. Marinum infection M. ulcerans infection (Buruli ulcer) A huge ulcer with a clean base and undermined margins extends into the adipose tissue of a Ugandian child. Harrisons principles of internal medicine, 15th ed. M. flavescens NTM skin infection M. marinum M. kansasii skin infection 38 year-old female, SLE Recurrent M. chelonae infection Edema, erythematous nodules, scars on the lower legs of an 83year-old female, who was taking oral glucocoricoids chronically for asthma. Harrisons principles of internal medicine, 15th ed. M. chelonae NTM skin infection M. absxessus M. kansasii Clinically Significant NTM Disease NTUH, 1992-1996 Infection Pulmonary No. 10 Etiologies MAC (3), M. fortuitum (2), M. abscessus (1) M. chelonae (1), M. gordonae (1) Soft tissue & osteomyelitis 16 M. abscessus (4), M. fortuitum (2), M. marinum (2) M. chelonae (1), M. gordonae (1), M. haemophilum (1), M. kansasii (1) Disseminated 5 MAC (3), M. chelonae (1), M. scrofulaceum (1) Keratitis & conjunctivitis 7 M. abscessus (2), M. fortuitum (2), M. chelonae (2), M. xenopi (1) Peritonitis 1 MAC (1) Shih JY et al J Formos Med Assoc 1997 Thanks for attention M. kansasii pneumonia 30 F NTM infection of the lung in HIV- patients Cavitary disease in the upper lung zones, similar to pulmonary tuberculosis, is seen in approximately 90 percent of patients with M. kansasii infection and perhaps 50 percent of those with Mycobacterium avium complex (MAC) infection. The cavities caused by these organisms tend to have thinner walls and less surrounding parenchymal opacity than those caused by M. tuberculosis Approximately 50 percent of patients with MAC lung disease have radiographic abnormalities characterized by nodules associated with bronchiectasis or nodular/bronchiectatic disease. The nodules and bronchiectasis are usually present within the same lobe and occur most frequently in the right middle lobe and lingula NTM Disease Treatment Regimen Recommendations Mycobacteria Established Suggested M. scrofulaceum M. malmoense, M. simiae (lung) RIF, ETH, INH, STM (AMIK) CLAR (AZI), CIP, CLOF MAC (disseminated) CLAR (AZI), ETH CLOF, RIFB, RIF, CIP, AMK M. kansasii, M. szulgai RIF, INH, ETH STM, CIP, CLAR M. xenopi RIF, INH, ETH STM M. marinum ETH, RIF, DOX, TMP-SMX STM, CIP M. haemophilum – RIF, CFOX, DOX, TMP-SMX M. fortuitum AMIK, CIP, SULF CLOF, CLAR, CFOX, DOX, IPM M. abscessus AMIK CLOF, CLAR, CLOX M. chelonae TOB (AMIK) CLOF, CLAR, DOX Manual of Clinical Microbiology 1999 MAC Pulmonary Diseases Treatment Clarithromycin (500 mg bid) or azithromycin (250 mg gd) Rifampin (600 mg qd) or rifabutin (300 mg qd) Ethambutol (25 mg/kg for 2 m, then 15 mg/kg) Streptomycin (2-3 times/week for first 8 weeks) Duration: culture (-) on therapy for one year Disseminated M. avium Complex Disease Treatment 1. Clarithromycin (500 mg bid) or azithromycin (250500 mg gd) 2. Ethambutol (25 mg/kg for 2 m, then 15 mg/kg) 3. Rifabutin (300 mg qd) or rifampin (600 mg qd) (Clofazimine, ciprofloxacin, amikacin, streptomycin) Duration: 1+2+3 life long M. kansasii Pulmonary Disease Treatment Isoniazid (300 mg qd) Rifampin (600 mg qd) Ethambutol (25 mg/kg for 2 m, then 15 mg/kg) Clarithromycin or rifabutin (substituted for rifampin) in AIDS patients with protease inhibitors Duration: 18 months with > 12 month culture (-) Antibiotic Treatment Rapidly Growing Mycobacteria Bacteria M. abscessus Parenteral Amikacin, Imipenem Clarithromycin, Oral Quinolones, Sulfonamides M. chelonae Amikacin (tobramycin), Clarithromycin Imipenem M. fortuitum Amikacin, Cefoxitin Clarithromycin M. smegmatis Amikacin, Imipenem Doxycycline, Quinolones, Sulfonamides Guay DRP Ann Pharmacother 1996 Antibiotic Treatment Rapidly Growing Mycobacteria (III) Pulmonary disease Organism Treatment M. fortuitum Cefoxitin + amikacin (4-8 weeks) sulfamethoxazole + doxycycline + ciprofloxacin (ofloxacin) M. abscessus Cefoxitin + amikacin + macrolides (4-6 weeks) surgical excision macrolides (6-12 months) Clinical Syndromes of NTM Disease Chronic pulmonary disease Lymphadenitis Localized skin, soft tissue, and skeletal infection Infection of bursae, joints, tendon sheaths, and bones Disseminated disease in patients without AIDS Disseminated disease in patients with AIDS Other infections Harrisons principles of internal medicine, 15th ed. NTM Pulmonary Disease Immune Suppression Local Alcoholism Bronchiectasis Cyanotic heart disease Cystic fibrosis Prior mycobacterial disease Pulmonary fibrosis Smoking/COPD None General Leukemia Lymphoma Organ transplantation Immunosuppressive therapy HIV (+), CD4 count <200