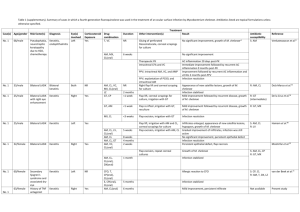
443 Rapid Development of Resistance to Clarithromycin Following Monotherapy for Disseminated Mycobacterium chelonae Infection in a Heart Transplant Patient Pablo Tebas, Faisal Sultan, Richard J. Wallace, Jr.,* and Victoria Fraser From the Infectious Diseases Division, Department of Medicine, Washington University School of Medicine, St. Louis, Missouri Mycobacterium chelonae (formerly known as M. chelonae subspecies chelonae) is a rapidly growing mycobacterium that can cause disseminated infections, especially in immunocompromised hosts. The bacterium is typically resistant to antimicrobial agents; less than 20% of M. chelonae isolates are susceptible to trimethoprim-sulfamethoxazole, doxycycline, erythromycin, or ciprofloxacin. Findings in a recent study suggested that clarithromycin may be the drug of choice for the treatment of cutaneous (disseminated) disease due to M. chelonae. We describe a 60-year-old heart transplant patient with disseminated M. chelonae infection for whom monotherapy with clarithromycin failed because of the rapid development of resistance to the drug. Case Report A 60-year-old male underwent orthotopic heart transplantation on 1 December 1992 because of severe ischemic cardiomyopathy. After transplantation, he received treatment with prednisone, cyclosporin A, and azathioprine as immunosuppressive agents and trimethoprim-sulfamethoxazole (TMP-SMZ) as prophylaxis against Pneumocystis carinii. On Received 3 March 1994; revised 23 May 1994. * Current affiliation: Department of Microbiology, University of Texas Health Center, Tyler, Texas. Reprints or correspondence: Dr. Pablo Tebas, Infectious Diseases Division, Washington University, Box 8051, 660 South Euclid, St. Louis, Missouri 63110. Clinical Infectious Diseases 1995;20:443-4 © 1995 by The University of Chicago. All rights reserved. 1058-4838/95/2002-0032$02.00 28 December 1992 he had an episode of acute rejection that was treated with three boluses of 5 methyl-prednisolone (500 mg each). On 30 March 1993 he presented with multiple, red, nontender subcutaneous nodules. A nodule had appeared on his right hand 6 weeks before presentation, and similar lesions subsequently developed on both arms. He denied having fever or any systemic symptoms except fatigue. A physical examination revealed multiple subcutaneous nodules (1 cm in diameter), primarily on the arms and legs; two of the lesions were pustular. The white blood cell count was 5,700/mm 3 , and the creatinine level was 2.3 mg/dL. Examination of an aspirate of the nodules showed an acidfast, gram-positive, branching filamentous organism. The patient began treatment with high-dose TMP-SMZ for suspected nocardiosis. The organism was subsequently identified as M. chelonae, and treatment with clarithromycin (500 mg twice a day) was initiated. The dosage of TMP-SMZ was reduced to one double-strength pill every day. The nodules disappeared while the patient was receiving clarithromycin therapy (the drug susceptibilities of the organism are shown in table 1). In June 1993 the patient developed new nodular lesions on the forearms and general malaise. Examination of a skin biopsy specimen again showed acid-fast, branching filamentous organisms. M. chelonae was identified, but the isolate was now highly resistant to clarithromycin. Immunosuppressive drugs were reduced to the minimum dosage possible, and intravenous therapy with imipenem and tobramycin was started; the patient's clinical condition improved. Tobramycin therapy was discontinued 4 weeks later because of nephrotoxicity. In October 1993, after 14 weeks of imipenem monotherapy, the patient had another relapse. Culture of a skin lesion yielded M. chelonae; the isolate's susceptibility pattern was similar to those of the two previous isolates except for a onedilution rise in the MIC of imipenem (MIC = 16 tig/mL), an increase in the MIC of the aminoglycosides, and development of clinically significant resistance to clarithromycin. With the agreement of the patient, all antibiotic therapy was discontinued because of his lack of response, the increase in Downloaded from http://cid.oxfordjournals.org/ at University of Arizona on May 31, 2015 Mycobacterium chelonae (formerly known as M. chelonae subspecies chelonae) is a rapidly growing mycobacterium that causes skin and soft tissue infections; these infections may disseminate, especially in immunocompromised hosts. The disseminated form of the disease usually presents as multiple subcutaneous nodules that involve the extensor surfaces of the arms and legs [1, 2]. The bacterium is typically resistant to antimicrobial agents, and <20% of M. chelonae isolates are susceptible to trimethoprim-sulfamethoxazole, doxycycline, erythromycin, or ciprofloxacin [3-6]. Findings in a recent study suggest that clarithromycin may be the drug of choice for treatment of cutaneous (disseminated) disease due to M. chelonae [7]. In an open noncomparative trial in which 14 patients who had M. chelonae disease received monotherapy with clarithromycin, 11 patients had an excellent response, 2 patients died of unrelated conditions, and 1 patient who did not comply with the regimen initially responded (this last patient then relapsed; the M. chelonae isolated was resistant to clarithromycin) [7]. We describe a second patient with disseminated M. chelonae infection for whom clarithromycin monotherapy failed because of the rapid development of resistance to the drug; the findings in this case question the value of single-drug therapy for M. chelonae infection. 444 Tebas et al. Table 1. Summary of susceptibilities of Mycobacterium chelonae isolated from a heart transplant recipient with disseminated infection. MIC of M. chelonae (AgImL) First isolate (4/15/93) Second isolate (6/4/93) Third isolate (11/8/93) Amikacin Tobramycin Clarithromycin Doxycycline Cefoxitin Imipenem Sulfamethoxazole Ciprofloxacin Azithromycin 32 <2 0.125 >16 >256 8 >32 8 1 32 2 >128 16 >256 8 >32 8 >32 >64 8 >128 >16 >256 16 >32 8 >128 NOTE. All tests were performed at the Mycobacterial/Nocardia Research Laboratory at the University of Texas Health Center in Tyler, Texas. antibiotic resistance, and the necessity of maintaining prolonged intravenous access. The patient received no treatment for 8 months and remained stable; the few relapses that occurred were self-limited. He died of cardiac disease in September 1994. An autopsy revealed evidence of ongoing M. chelonae infection, but this infection did not directly contribute to his death. Discussion The spectrum of infections produced by M. chelonae has recently been described [8]. More than 50% of patients who are infected with M. chelonae have disseminated cutaneous infections. Disseminated infections are usually seen in immunocompromised hosts, and the chronic use of steroids seems to be the most important factor predisposing to disseminated infection [8]. One-third of patients who are infected with M. chelonae have localized infections in the skin or bone, which usually occur in immunocompetent hosts following minor trauma. Approximately 10% of these patients have catheter-related infections. Clinical data on antibiotic susceptibility and resistance for M. chelonae have not been well defined, and the National Committee for Clinical Laboratory Standards has not determined breakpoints for this bacterium. To determine MICs for M. chelonae, most laboratories use the breakpoints for aerobic bacteria with slight modifications. According to recent studies, clarithromycin is the drug most active against M. chelonae; the MICs of clarithromycin for most isolates were <0.25 Ag/mL [4]. The findings in this case demonstrate the difficulties in managing patients with disseminated infections due to M. chelonae. Although clarithromycin is a promising drug for the treatment of infections due to this organism, rapid emergence of resistance can be a problem even for patients who comply with the treatment regimen. Rapid development of resistance has also been reported for other drugs (e.g., ciprofloxacin) that have been used as monotherapy in the treatment of other rapidly growing mycobacteria (e.g., Mycobacterium fortuitum) [6]. Because of the rarity of disseminated infection due to M. chelonae, prospective comparative studies of other potential therapies will be difficult. On the basis of the findings in this report and experience with other mycobacterial infections, the use of at least two drugs (one of which should be clarithromycin) should be considered for treatment of M. chelonae infections, especially in immunosuppressed patients. Potential agents to use in combination (which were efficacious at least temporarily in this case) include imipenem and tobramycin. These drugs could be given initially as part of induction therapy. Therapy for disseminated M. chelonae infections in immunocompromised hosts should be continued for at least 6 months [7, 9]. Resistance to clarithromycin and other drugs may still develop in patients with disseminated M. chelonae infection who have received treatment. If resistance develops, treatment with a realistic potential for cure would not be available; thus, the patient's only option may be symptomatic therapy including drainage of obvious fluid collections. References 1. Cooper JF, Lichtenstein MJ, Graham BS, Schaffner W. Mycobacterium chelonae.. a cause of nodular skin lesions with a proclivity for renal transplant recipients. Am J Med 1989; 86:173 - 7. 2. Wallace RJ Jr. The clinical presentation, diagnosis, and therapy of cutaneous and pulmonary infections due to the rapidly growing mycobacteria, M. fortuitum and M. chelonae. Clin Chest Med 1989;10:419 - 29. 3. Swenson JM, Wallace RJ, Silcox VA, Thornsberry C. Antimicrobial susceptibility of five subgroups of Mycobacterium fortuitum and Mycobacterium chelonae. Antimicrob Agents Chemother 1985;28: 807-11. 4. Brown BA, Wallace RJ Jr, Onyi GO, De Rosas V, Wallace RJ III. Activities of four macrolides, including clarithromycin, against Mycobacterium fortuitum, Mycobacterium chelonae, and M. chelonae-like organisms. Antimicrob Agents Chemother 1992; 36:180-4. 5. Wallace RJ Jr, Brown BA, Onyi GO. Susceptibilities of Mycobacterium fortuitum biovar. fortuitum and the two subgroups of Mycobacterium chelonae to imipenem, cefmetazole, cefoxitin, and amoxicillin-clavulanic acid. Antimicrob Agents Chemother 1991;35:773 - 5. 6. Wallace RJ Jr, Bedsole G, Sumter G, et al. Activities of ciprofloxacin and ofloxacin against rapidly growing mycobacteria with demonstration of acquired resistance following single-drug therapy. Antimicrob Agents Chemother 1990; 34:65-70. 7. Wallace RJ, Tanner D, Brennan PJ, Brown BA. Clinical trial of clarithromycin for cutaneous (disseminated) infection due to Mycobacterium chelonae. Ann Intern Med 1993; 119:482-6. 8. Wallace RJ Jr, Brown BA, Onyi GO. Skin, soft tissue, and bone infections due to Mycobacterium chelonae chelonae: importance of prior corticosteroid therapy, frequency of disseminated infections, and resistance to oral antimicrobials other than clarithromycin. J Infect Dis 1992; 166:405-12. 9. Wallace RJ, O'Brien R, Glassroth J, Raleigh J, Dutt A. Diagnosis and treatment of disease caused by nontuberculous mycobacteria. Am Rev Respir Dis 1990; 142:940-53. Downloaded from http://cid.oxfordjournals.org/ at University of Arizona on May 31, 2015 Drug CID 1995;20 (February)