Case 5

SHOCK
Case presentations and CVS
Monitoring
Case 4
A 29-year-old lady (72 kg) arrives in the resuscitation room drowsy with the following vital signs:
• BP 80/50 mmHg,
• pulse 130 per minute,
• RR 28 per minute,
• Sa02 95% on 10 L/min O2 via a reservoir bag mask,
• temperature 38.5
° C.
She has a petechial rash on her trunk.
ABG: pH 7.31
Pa02 35.5 kPa
PaC02 3.5 kPa bicarb 12.7mmol/L
BE-10.
She responds to voice and there is no neck stiffness.
Her bedside glucose measurement is 6.2 mmol/L
Q1: What is your diagnosis?
Q2: What is your management?
Case 4
“A” - ensure a patent and protected airway, give a high concentration of oxygen (for example, 15 L/minute via a reservoir bag mask),
“B” - assess and treat any breathing problems,
“C” - assess and treat any circulation problems,
“D” - assess conscious level and check for Temp & UO.
The petechial rash is a clue to the possible cause of sepsis – think meningococcal and/or staphylococcal infections.
A full examination and appropriate investigations
(including CT/MRI, CSF and other cultures) should follow.
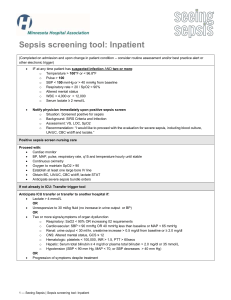
Modified Early Warning Score (MEWS) – useful tool in recognition of patients with presumed infection
Score 3 2 1 0 1 2 3
BP SYS < 80 80-89 90-109 110-160 161-180 181-200 >200
PULSE < 40
RESP.
TEMP.
40-50 51-100 101-110 111-129 >130
< 8 -
-
8-20 21-25 26-30 >30
<35 35.1-37.9 38.0-38.4 >38.5 -
AVPU New New
C onfusion
Alert Voice Pain Unrespon
W eakness sive
-----------------------------------------------------------------------------
If Score 3 in one category or total Score 4 - Think infection!
2 Signs and symptoms of infection (SSI) plus presumed infection = Sepsis
•
•
•
•
•
Two or more of the following :
Tachycardia > 90 bpm
Core temperature > 38.3
° C < 36 ° C
Tachypnoea > 20 bpm
WCC >12,000 or <4,000 or >10% immature neutrophils
Hyperglycaemia in the absence of Diabetis Mellitus
Q: Is there at least one organ failure already?
Septic shock - Acute circulatory failure unexplained by other causes.
Infection SSI Sepsis
Severe sepsis
Death
Septic shock
– is defined as
Severe sepsis with hypotension refractory to adequate volume resuscitation ,
Hypotension is defined as a systolic blood pressure of <90mmHg or a reduction of >40mmHg from baseline )
Sepsis with signs of at least one acute organ dysfunction (organ failure)
Cardiovascular
Unexplained metabolic acidosis
Central nervous system
Respiratory
Renal
Hepatic
Haematologica
SSI - Signs and symptoms of infection
Case 4
Patient has Severe Sepsis according to the SSC.
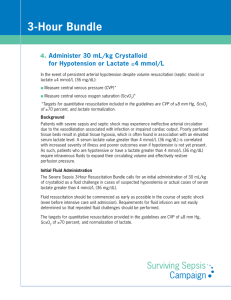
Fluid resuscitation using crystalloids or colloids 20-40 ml/kg/hr
Blood cultures and Lactate taken ASAP
Antibiotics administered within 1 hour
If BP is not responsive to fluids or if serum lactate is still elevated consider CVP, Invasive Arterial line for ABG and CVS monitoring
Repeated boluses of crystalloid/colloid 250-500 ml every 30 min until
CVP 8-12 mmHg
Vasopressors via central line if MAP < 65 mm Hg during and after adequate fluid resuscitation - Noradrenaline (4 mg in 50 ml of 5%
Dextrose - start at 0.05 mcg/kg/min) or Metaraminol infusion.
If Scv O2 < 70 % after adequate fluid replacement and Noradrenaline running, start Isotopes (Dobutamine at 2.5 mcg/kg/min or Adrenaline infusion via central line) and/or give RBC’s (to keep Ht above 30)
Case 5
A 53 year old motorcyclist is brought by Air
Ambulance having been involved in a high speed RTA with a truck.
Blood pressure is unrecordable, pulse is not palpable, except in carotid and femoral regions
A 14G cannula has been inserted by ‘ cutdown ’ in the left great saphenous vein, NaCl 0.9% running
He is intubated and ventilated
Q1: What are the possible causes of his low BP?
Q2: What should the management comprise?
Case 5
Management plan
:
• ABC approach
• Volume resuscitation
• Achieve stability
• Transfer to CT scan for ‘ Trauma series ’
• Act upon findings
A and B are checked and cleared
• No pneumothorax detected clinically
• CXR confirms no extrapulmonary air
Case 5
Circulation:
• Despite on-going IV fluid infusion, BP is difficult to record via NIBP monitor
• Additional venous access obtained (14G) - bloods are taken and Hartmann’s 1000 ml given stat.
• Radial Arterial line inserted, showing invasive pressure of 76/42 mmHg
Q1: What might be happening?
Q2: What could be done to investigate?
Case 5
FAST scan
• Suggests some free fluid in abdomen
• Small amount of fluid in pericardium
• Otherwise normal but empty heart appearance
• BP is very low - patient is not stable for CT scanner or theatre.
Q1: How does this help you?
Q2: What could be done, in view of the continuing instability?
Case 5
In view of possible intra abdominal bleeding
2 units of O (I) Neg blood and 1L Colloids given,
In order to support BP:
• Metaraminol IV boluses given every 3-5 mins,
• Subclavian CVC line is obtained and Noradrenaline infusion started by ITU Registrar
• But HR is now 150, BP is 46-51 mmHg systolic.
• Patient is in PEA arrest, +/- drug induced SVT ??
CPR started with Adrenaline given every 3 min.
Q: What else could be done to save life?
Case 5
CPR:
• 3 minute cycles with 1 mg Adrenaline given each time
• BP is unresponsive to drugs, only to CPR
• Massive Transfusion Protocol (MTP) is activated and another 6 u-ts of O (I) Neg blood given
Thoracotomy for open compressions in A&E
• Descending Aorta clamped
• Blood pressure improves somewhat (110/60)
• Heart is pumping well, massage stopped
• Patient is more stable now, can go to CT scanner
Case 5
CT results
• Small splenic and liver injuries (both Grade 2)
• Undisplaced T6 spinal fracture, no brain injury
• Femoral fractures
Went to Theatre for Laparotomy + Orthopaedics
• Spleenectomy, but only mild blood loss in abdomen
• Aortic clamp removed, chest drain placed
• Ex-fix placed on femur to prevent bleeding
• CVP reading is low CVP (~2 mmHg)
• Requiring moderate dose of noradrenaline to maintain adequate blood pressure
Q: Why is the blood pressure still poor?
Case 5
In Critical Care
• Intubated, ventilate, positive fluid balance is almost
10.5 litres;
• Patient noted to be moving arms but not legs;
• When woken up from sedation completely, still could not move legs
• MRI shows cord damage at T6 level
• Discharged from ITU in 2 weeks with some neurological improvement
Presumably spine was displaced enough to damage cord then returned to normal anatomical position
Questions