Chapter 4: The Biomechanics of Human Bone Growth and
advertisement

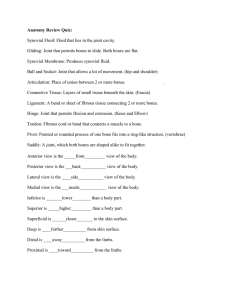
The Rigid Framework of the Body THE SKELETAL SYSTEM CHAPTER 10: Skeletal Anatomy Skeletal System • Mechanically, the skeletal system my be thought of as an arrangement of rigid links connected to each other at joints to allow specific movements. Knowledge of the skeletal system is important for ALL movement analysts Composition and Structure of Bone Tissue • Mechanical functions of bone • provides a rigid skeletal framework to support and protect other tissues. • forms a system of rigid levers (links) that can be moved by forces from the attached muscles (rotated by torques from the attached muscles). Divisions of the Skeletal System (239): • Central or axial skeleton • skull, vertebrae, sternum, and ribs • Peripheral or appendicular skeleton • bones of the arms and legs Bone Shape • The mechanical stresses imposed a bone and its function determine its shape. Three point bending test of an intact rat femur. The resulting force-deflection curve from a three point bend test provides the biomechanical properties of bone Types of Bones • Short bones • Limited gliding motions and shock absorption. • Small, cubical structures (e.g., carpals, tarsals) Types of bones • Short bones • Flat bones • Protection, provide attachment sites • Flat in shape (e.g., scapula) Types of bones • Short bones • Flat bones • Irregular bones • Multi-functional • odd shapes (e.g., vertebrae) Types of bones • • • • Short bones Flat bones Irregular bones Long bones • long shaft and bulbous heads (condyles, tubercles, or tuberosities) • serve as levers for movement (e.g., tibia, femur, humerus, radius, ulna, clavicle, fibula, metatarsals, and the phalanges) Material Constituents: • Calcium carbonate 60 to 70% of mass • calcium phosphate • collagen • water 25 to 30% of bone mass Material Constituents: •stiffness • Calcium carbonate •compressive • calcium phosphate strength • collagen • flexibility (tensile strength) • water • tensile & compressive strength Varies from person to person Structural Organization Cortical bone (compact) Low porosity 5-30% of bone volume nonmineralized tissue. Trabecular (spongy\cancellous) High porosity 30 to > 90% volume non-mineralized tissue. Load and Response •Stress • force per unit area • Strain • deformation • amount of deformation divided by original length Life is an ongoing cycle of repeated applied external stresses, interrupted by applications of isolated stresses of varying magnitudes. Generic Stress-Strain Relationship Elastic Limit Strain (deformation) Bone Stress-Strain Relationship Fracture Threshold Strain (deformation) Tension Compression Stress to Fracture Relative Bone Strength Load Type Fractures: with excessive loads, bone tends to fracture on the side loaded in tension. Bone Growth and Development • Living bone is dynamic • continually changes throughout lifespan. • Longitudinal growth • length increases occur at the epiphyses • epiphyseal plates. • produce new bone tissue until closing during adolescence or early adulthood. • Circumferential growth • Bones alter diameter throughout lifespan • most rapid change before adulthood. • Osteoblasts • Osteoclasts • form new bone • resorb existing bone Critical factor in bone modelling/remodelling: balance of their action Bone Response to Stress • Wolff's law (1892) • tissue adapts to level of imposed stress • increased stress • • decreased stress • • hypertrophy (increase strength) atrophy (decrease strength) SHAPE REFLECTS FUNCTION • Genetics, Body weight, physical activity, diet, lifestyle (see note clippings) (review the stress continuum) Protecting our Bones in Sport The pattern of trabecular bone in the greater trochanter neck of the femur head of the femur reflects femur’s roles: muscle attachment flexibility weight transfer support Atrophy in Bone • Weight & strength decrease • Calcium content diminishes • reduced BMD • trabecular integrity is lost Bone stimulating factors Rate of loading Magnitude Frequency BMD and walking Quartiles based on miles walked/week Krall et al, 1994, Walking is related to bone density and rates of bone loss. AJSM, 96:20-26 Is physical decline inevitable with aging? No. Genetics dominates. But lifestyle modulates. Changing concept of old age. How much activity do we need? The synovial joint You should be able to draw and label this diagram. Joint Architecture & Classification • Synarthoses (immovable) • Amphiarthroses (slightly movable) • Diarthroses or synovial (freely movable) • Get our attention William Hunter (1743) [The bone ends] are covered with a smooth elastic crust, to prevent mutual abrasion; connected with string ligaments, to prevent dislocation; and enclosed in a bag that contains a proper fluid deposited there for lubricating the two contiguous surfaces. Synovial Joint Features • Articular (hyaline) cartilage • • • • covers articulating surfaces no blood vessels no nerves Serves 3 purposes: • reduces friction • increases articulating area to reduce stress • shock absorption Synovial Joint Features • Articular (hyaline) cartilage • Articular (fibrous/joint) capsule • double layer membrane surrounds synovial joint • outer connects bones • inner secretes synovial fluid • may have definite ligaments Synovial Joint Features • Articular (hyaline) cartilage • Articular capsule • Synovial fluid • clear, slightly yellow liquid • lubricates joint • nourishes cartilage Synovial Joint Features • • • • Articular (hyaline) cartilage Articular capsule Synovial fluid Fibrocartilage: • disc or partial disc between articulating bones. • • • • • Intervertebral discs; menisci increase surface area: reduce stress improve fit of articulating surfaces limits translation or slip of bones shock absorption Synovial Joint Features • • • • • Articular (hyaline) cartilage Articular capsule Synovial fluid Fibrocartilage Tendon sheaths • surround tendons located close to bones • reduce stress on tendon • maintain low friction Synovial Joint Features • • • • • • Articular (hyaline) cartilage Articular capsule Synovial fluid Fibrocartilage Tendon sheaths Bursae • small synovial fluid filled capsules • separate tendon from bone to reduce friction Mobility is a very precious gift. More complex than the space shuttle. Role of Meniscii Meniscii effect on mechanical stress Back pain 'starts in school By Roger Highfield Around half of all children are at risk of suffering a lifetime of back problems because of awkward postures during lessons and using computers, furniture and other equipment designed for adults. Forty per cent of schoolchildren suffer health problems considered in adults to be "work related” that could affect them for the rest of their lives, said Prof Peter Buckle, of the University of Surrey's Robens Centre for Health Ergonomics in Guildford. He said a Danish study showed that 51 per cent of children aged 13 to 16 reported low back pain in the previous year, and 24 per cent of 11- to14-year-olds in the north-west of England reported having back pain in the month prior to completing a questionnaire. "Under European laws the health of workers is protected," he said. "But when we start to look at young adults and children the picture is far less clear. "Worryingly, evidence is starting to show that, for some health problems, we may be leaving it too late before we start helping." A study found that those reporting low back pain in school were more likely to report low back pain as adults. (Filed: 10/09/2002) © Copyright of Telegraph Group Limited 2002. Joint Stability • Joint stability - resist abnormal displacement of the articulating bones. • Dislocation - bones displace out of their normal positions. • Subluxation - a partial dislocation of a joint. Joint Stability • Dislocation - bones displace out of their normal positions. Impingement Subluxation Dislocation Joint Stability • Contributing factors • shape of articulating surfaces • close-packed position: position of max contact • knee, wrist, interphalangeal: full extension • ankle: full dorsiflexion • loose-packed position: position other than c-p • most prone to dislocation, cartilage damage Joint Stability • Fatigue or improper use of the joints are major contributing factors. • Muscles add to joint stability. Joint Stability • Contributing factors • arrangement of ligaments & muscles • concept of rotary & stabilizing components of muscle/ligament tension • rotary: component that causes/tends to cause rotation • stabilizing: acts parallel to the bone Joint Stability • Rotary component - perpendicular component of a muscle force. • Stabilizing component - parallel component of a muscle force acting toward the joint center. • Dislocating component - parallel component of a muscle force acting away from the joint center. Joint Stability • Fascia - fibrous connective tissue that surrounds muscles and the bundles of muscle fibers within muscles, providing protection and support. • Iliotibial band. Flexibility: ROM at a joint Flexibility and Injury • Risk of injury is heightened when joint flexibility is extremely low, extremely high, or significantly imbalanced between dominant and non-dominant sides of the body. • Although people usually become less flexible with age, a large part is due to inactivity. Joint Flexibility • Factors influencing joint flexibility: • Shape of articulating bones • other soft tissue: stiffness & mass • muscle: current ‘tone” • ligaments: arranged in direction of expected pull • fatty tissue • • • • temperature: warmer = more pliant past injury: collagen alignment integrity clothing AGE??? vs inactivity Why is flexibility important? • Basic component of a fitness profile. Why is flexibility important? • Basic component of a fitness profile. • allows for greater choice of movement patterns • slides of gymnasts • elderly shoulder ROM & independence • Osteoarthroses • contractures (ie cerrebral palsy) • sprain ankle & inflammation Why is flexibility important? • Basic component of a fitness profile. • allows for greater choice of movement patterns • reduce risk of injury • absorb energy over a greater distance (time) • CAVEAT: Risk of injury increased with ROM high, or low • slide & next overhead From Cowan et al, 1988, ref #304 Why is flexibility important? • Basic component of a fitness profile. • allows for greater choice of movement patterns • reduce risk of injury • Increase forceful performance • apply force over a greater distance (time) • violation of principle of summation of joint force • violation of principle of IMPULSE Techniques for increasing joint flexibility Best Advice: Use It Don’t Lose It How best to stretch? Types of stretching: • Active - stretching muscles, tendons, & ligaments by active development of tension in the antagonist muscles • Passive - stretching muscles, tendons, & ligaments by a force other than tension in the antagonist muscles (gravity, another segment, another person) Types of stretching • Ballistic - a series of quick, bouncing movements. • Static - a slow controlled stretch held over time (10-30s, 3 to 4 reps) • Proprioceptive Neuromuscular Facilitation alternating contraction and relaxation of the muscles being stretched. • Contract-relax& pull-contract Techniques for increasing joint flexibility • Review neural innervation • Golgi tendon organs • located in junctions between muscles and tendons • responsive to tension in tendon • inhibits tension development in active muscle Techniques for increasing joint flexibility • Review neural innervation • Golgi tendon organs • Muscle spindles • located parallel to the muscle fibers in the belly of the muscle • responsive to lengthening of fibers (rate & length) Stretch Reflex • activate stretched muscle, inhibit antagonist (reciprocal inhibition) Techniques for increasing joint flexibility • Review neural innervation • Golgi tendon organs • Muscle spindles • Flexibility training goal • do not invoke stretch reflex (do not activate the muscle group to be stretched) HOW??? • activate golgi tendon organs (further inhibit the muscle group to be stretched (reduce tonus)) HOW???