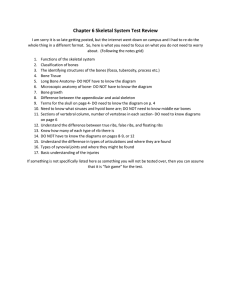
SKELETAL CARTILAGES
advertisement

BONES AND SKELETAL TISSUES SKELETAL CARTILAGES • Skeletal cartilages: – Made of some variety of cartilage – Consists primarily of water • High water content accounts for its resilience – Ability to spring back to its original shape after being compressed – Contains no nerves or blood vessels – Surrounded by a layer of dense irregular connective tissue called the perichondrium • Acts like a girdle to resist outward expansion when the cartilage is compressed • Contains the blood vessels from which nutrients diffuse through the matrix to reach the cartilage cells – This mode of nutrient delivery limits cartilage thickness SKELETAL CARTILAGES • Three types: – Hyaline – Elastic – Fibrocartilage • All three types have the same basic components: – Cells called chondrocytes • Encased in small cavities (lacunae) within an extracellular matrix containing a jellylike ground substance and fibers HYALINE CARTILAGE • Looks like a frosted glass when freshly exposed • Provides support with flexibility and resilience • Most abundant skeletal cartilage – Chondrocytes appear spherical – Only fiber type in the matrix is fine collagen fibers HYALINE CARTILAGE HYALINE CARTILAGE • Includes: – Articular cartilages: • Cover the ends of most bones at movable joints – Costal cartilages: • Connect the ribs to the sternum (breastbone) – Respiratory cartilages: • Form the skeleton of the larynx (voicebox) – Reinforces other respiratory passageways – Nasal cartilages: • Support the external nose BONE CARTILAGE ELASTIC CARTILAGE • Looks very much like hyaline cartilages, but they contain more stretchy elastic fibers and so are better able to stand up to repeated bending ELASTIC CARTILAGE ELASTIC CARTILAGE • More flexible than hyaline • Located only in the: – External ear – Epiglottis of the larynx: • Flap that bends to cover the opening of the larynx each time we swallow BONE CARTILAGE FIBROCARTILAGE • Highly compressible and have great tensile strength • Perfect intermediate between hyaline and elastic cartilages • Consist of roughly parallel rows of chondrocytes alternating with thick collagen fibers FIBROCARTILAGE FIBROCARTILAGE • Occur in sites that are subjected to both heavy pressure and stretch: – Padlike cartilages (menisci) of the knee – Discs between vertebrae BONE CARTILAGE Growth of Cartilage • Growth occurs in two ways: – Appositional growth (growth from the outside) results in outward expansion due to the production of cartilage matrix on the outside of the tissue • Cartilage-forming cells in the surrounding perichondrium secrete new matrix against the external face of the existing cartilage tissue – Interstitial growth (growth from inside) results in expansion from within the cartilage matrix due to division of lacunae-bound chondrocytes and secretion of matrix • Lacunae-bound chondrocytes divide and secrete new matrix, expanding the cartilage from within Growth of Cartilage • Typically, cartilage growth ends during adolescence when the skeleton stops growing • Under certain conditions—during normal bone growth in youth and during old age— calcium salts may be deposited in the matrix and cause it to harden, a process called calcification – NOTE: calcified cartilage is NOT bone CLASSIFICATION OF BONES • 206 named bones of the human skeleton are divided into two groups: – Axial skeleton: • Forms the long axis of the body • Protect, support, or carry other body parts • Includes: – Skull – Vertebral column – Rib cage – Appendicular skeleton: • Bones of the upper and lower limbs, and the girdles (pectoral/shoulder and pelvic/hip) that attach them to the axial skeleton • Help us to get from place to place (location) BONE CARTILAGE CLASSIFICATION OF BONES • Classified by shape: – Long – Short – Flat – Irregular BONE SHAPE Long Bones • Longer than they are wide: – Have a definite shaft and two ends – Consist of all limb bones except patellas, the carpels (wrist), and tarsals (ankles) • Named for their elongated shape, NOT their overall size – Example: the three bones in your fingers (digits) are long bones, even though they are very small BONE SHAPE Short Bones • Somewhat cube-shaped • Include: – Carpals: wrist – Tarsals: ankle – Sesamoid bone: • Shaped like a sesame seed • Special type of bone that forms in a tendon – Example: patella • Vary in size • Some clearly act to alter direction of pull of a tendon • Functions of others is not known BONE SHAPE Flat Bone • Thin, flattened and often curved • Include: – Most skull bones – Sternum (breastbone) – Scapulae (shoulder blades) – Ribs BONE SHAPE Irregular Bones • Complicated shapes that do not fit in any of the previous classes – Example: • Vertebrae • Coxae (hip bone) BONE SHAPE FUNCTIONS OF BONES • Besides contributing to body shape and form, our bones perform several important functions: – 1. Support – 2. Protection – 3. Movement – 4. Mineral storage – 5. Blood cell formation Support • Bones provide a framework that supports the body and cradles its soft organs • Examples: – Bones of the lower limbs act as pillars to support the body trunk – Rib cage supports the thoracic wall Protection • Fused bones at the skull protect the brain • Vertebrae surround the spinal cord • Rib cage helps protect the vital organs of the thorax Movement • Skeletal muscles, which attach to bones by tendons, use bones as levers to move the body and its parts – As a result, we can walk, grasp objects, and breathe Mineral Storage • Bone is a reservoir for minerals – Most important are calcium and phosphates – Stored minerals are released into the bloodstream as needed for distribution to all parts of the body: • Deposits and withdrawals of minerals to and from the bones go on almost continuously Blood Cell Formation • Most blood cell formation (hematopoiesis) occurs in the marrow cavities of certain bones Bone Structure • Because bones contain various types of tissue, bones are organs: – Bone (osseous) tissue – Nervous tissue in their nerves – Cartilage tissue in their articular cartilages – Fibrous connective tissue lining their cavities – Muscle and epithelial tissues in their blood vessels Gross Anatomy • Bone markings are projections, depressions, and openings found on the surface of bones that function as sites of muscle, ligament, and tendon attachment, as joint surfaces, and as openings for the passage of blood vessels and nerves Names of Bone Markings • Projections (bulges): grow outward from the bone surface – Projections that sites of muscle and ligament attachment: • Tuberosity: elevated round swelling – Large and rounded – May be roughened • Crest: elongated prominence – Narrow ridge – Usually prominent • Trochanter: to run – – – – Very large Blunt Irregularly shaped ONLY in the femur • Line: – Narrow ridge – Less prominent than crest • Tubercle: little swelling – Small and rounded • Epicondyle: above a knuckle (condyle) – Raised area on or above a condyle • Spine: – Sharp, slender, often pointed projection • Process: – Any bone prominence Names of Bone Markings • Projections That Help to Form Joints: articulation – Head: • Bony expansion carried on a narrow neck – Facet: small face • Smooth, nearly flat articular surface – Condyle: knuckle • Rounded articular projection – Ramus: branch • Armlike bar of bone Names of Bone Markings • Depressions and openings: – Allow blood vessels and nerves to pass • Meatus: passage/opening – Canal-like passageway • Sinus: curve, hollow – Cavity within a bone, filled with air and lined with mucous membrane • Fossa: furrow or shallow depression – Shallow, basinlike depression in a bone – Often serves as an articular surface • Groove: ditch – Furrow • Fissure: slender deep furrow – Narrow, slitlike opening • Foramen: passage/opening – Round or oval opening through a bone Bone Textures • Compact: – All bones have a dense outer layer consisting of compact bone that appears smooth and solid • Spongy Bone: – Internal to compact bone is spongy bone, which consists of honeycomb, needle-like, or flat pieces, called trabeculae (little beam) • In living bones the open spaces between trabeculae are filled with red or yellow bone marrow Compact/Spongy Bone Typical Long Bone Structure • All long bones have the same general structure: – Diaphysis: dia (through) / physis (growth) • • • Tubular shaft Forms the long axis of the bone Constructed of a relatively thick collar of compact bone that surrounds a central medullary cavity or marrow cavity – – In adults, the medullary cavity contains fat (yellow marrow) and is called the yellow bone marrow Epiphyses: epi (upon) / epiphyses (singular) • • • The ends of the bone Consist of internal spongy bone covered by an outer layer of compact bone Joint surfaces of each epiphysis is covered with a thin layer of articular (hyaline) cartilage, which cushions the opposing bone ends during joint movement and absorbs stress LONGBONE Typical Long Bone Structure • Epiphyseal line: sometimes called the metaphysis – Located between the epiphyses and diaphysis in an adult • Is the remnant of the epiphyseal plate, a disc of hyaline cartilage that grows during childhood to lengthen the bone LONGBONE Typical Long Bone Structure • Membranes: Periosteum – The external surface of the entire bone except the joint surfaces is covered by a glistening white, doublelayered membrane called the periosteum (peri=around / osteo=bone) • Outer fibrous layer is dense irregular connective tissue • Inner osteogenic layer abutting the bone surface consists primarily of: – Bone-forming cells: osteoblasts – Bone-destroying cells: osteoclasts LONGBONE Typical Long Bone Structure • Membranes: Periosteum – Richly supplied with nerve fibers, lymphatic vessels, and blood vessels, which enter the diaphysis via a nutrient foramen – Secured to the underlying bone by perforating (Sharpey’s) fibers • Tufts of collagen fibers that extend from its fibrous layer into the bone matrix – Provides anchoring points for tendons and ligaments • At these points the perforating fibers are exceptionally dense LONGBONE Typical Long Bone Structure • Membranes: Endosteum (within bone) – The internal surface of the bone is lined by a connective tissue membrane called the endosteum • Covers the trabeculae of spongy bone and lines the canals that pass through the compact bone • Like the periosteum, the endosteum contains both osteoblasts and osteoclasts LONGBONE Structure of Short, Flat, and Irregular Bones • Short, flat, and irregular bones consist of thin plates of periosteum-covered compact bone on the outside, and endosteumcovered spongy bone inside, which houses bone marrow between the trabeculae (no marrow cavity is present) • Not cylindrical • No shaft or epiphyses • Called the diploe (folded) – Arrangement resembles a sandwich FLATBONE Location of Hematopoietic Tissue in Bones • Hematopoietic tissue of bones, red bone marrow, is located within: • The trabecular cavities of the spongy bone in flat bones • The trabecular cavities of the spongy bone of the epiphyses in the long bones – Red bone marrow is found in: • All flat bones • Epiphyses, and medullary cavities of infants • In adults, distribution is restricted to flat bones and the proximal epiphyses of the humerus and femur – Hence, blood cell production in adult long bones routinely occurs only in the head of the femur and humerus – Red marrow found in the diploe of flat bones (such as the sternum) and in some irregular bones (such as the hip bones) is much more active in hematopoiesis » These are the sites used for obtaining red marrow samples – Yellow marrow in the medullary cavity can revert to red marrow if a person becomes very anemic and needs enhanced red blood cell production Microscope Anatomy of Bone • Although compact bone looks dense and solid, a microscope reveals that it is riddled with passageways that serve as conduits for nerves, blood vessels, and lymphatic vessels COMPACT BONE Microscope Anatomy of Bone Compact Bone • The structural unit of compact bone is the osteon, or Haversian system – Each osteon is an elongated cylinder oriented parallel to the long axis of the bone • • Tiny weight –bearing pillars Group of hollow tubes of bone matrix, one placed outside the next like the growth rings of a tree trunk – • – In diagram: osteon are drawn as if pulled out like a telescope to illustrate the individual lamellae Each matrix tube is a lamella (little plate), and for this reason compact bone is often called lamellar bone Although all of the collagen fibers in a particular lamella run in a single direction, the collagen fibers in adjacent lamella always run in opposite directions • This alternating pattern is beautifully designed to withstand torsion (twisting) stresses—the adjacent lamella reinforce one another to resist twisting OSTEON Microscope Anatomy of Bone Compact Bone • Collagen fibers are not the only part of bone lamellae that are beautifully ordered – • Running through the core of each osteon is: – • • Tiny crystals of bone salts align with the collagen fibers and thus also alternate their direction in adjacent lamellae The Central (Haversian) Canal that containing small blood vessels and nerve fibers that serve the needs of the osteon’s cells Perforating (Volkmann’s) Canals lie at right angles to the long axis of the bone, and connect the blood and nerve supply of the periosteum to that of the central canals and medullary cavity BOTH Haversian and Volkmann Canal are lined with endosteum COMPACT BONE Microscope Anatomy of Bone Compact Bone • (b):Osteocytes (spider-shaped mature bone cells) occupy lacunae (small space, cavity, or depression occupied by cells) at the junctions of the lamellae – Hair-like canals called canaliculi connect the lacunae to each other and to the central canal • Tie all the osteocytes in an osteon together, permitting nutrients and wastes to be relayed from one osteocyte to the next throughout the osteon • Although bone matrix is hard and impermeable to nutrients, its canaliculi and cell-to-cell relays (via gap junctions) allow bone cells to be well nourished – Function is to maintain the bone matrix: • If they die, the surrounding matrix is resorbed (remove-assimilated) COMPACT BONE Microscope Anatomy of Bone Compact Bone • Not all the lamellae in compact bone are part of osteons – (c): Lying between intact osteons are incomplete lamella called interstitial lamella • These either fill the gaps between forming osteons or are remnants of osteons that have been cut through by bone remodeling • (a): Circumferential lamellae are located just beneath the periosteum, extending around the entire circumference of the bone – Effectively resist twisting of the long bone COMPACT BONE Spongy Bone • • Lacks osteons Trabeculae (honeycomb network) align along lines of stress and help the bone resist stress as much as possible – These tiny bone struts are as carefully positioned as the flying buttresses of a Gothic cathedral • • Irregularly arranged lamella and osteocytes interconnected by canaliculi Nutrients reach the osteocytes by diffusing through the canaliculi from capillaries in the endosteum surrounding the trabeculae LONGBONE FLATBONE COMPACT BONE Chemical Composition of Bone • Organic components: – Cells (osteoblasts, osteocytes, and osteoclasts) – Osteoid: nonliving • Composed of secretions from the osteoblasts which contribute to the flexibility and tensile strength of bone that allows the bone to resist stretch and twisting – Ground substance: proteoglycans and glycoproteins – Collagen fibers: » Bonds in or between collagen molecules break easily on impact dissipating energy to prevent the force from rising to a fracture value » In the absence of continued or additional trauma, most of the bonds reform Chemical Composition of Bone • Inorganic components: – Make up 65% of bone by mass • Consist of hydroxyapatite (mineral salts) that is largely calcium phosphate, which accounts for the hardness and compression resistance of bone – Present in the form of tightly packed tiny crystals surrounding the collagen fibers in the extracellular matrix • Because of the salts they contain, bones last long after death and provide an enduring “monument” • Healthy bone is half as strong as steel in resisting compression and fully as strong as steel in resisting tension (stretching) BONE DEVELOPMENT • Ossification and osteogenesis are synonyms meaning the process of bone formation (os=bone / genesis=beginning) – In embryos: leads to the formation of the skeleton – Early adulthood: bones increase in length – Throughout life: bones are capable of growing in thickness – Adults: ossification serves mainly for bone remodeling and repair Formation of the Bony Skeleton • Before week 8, the skeleton of a human embryo is constructed entirely from fibrous membranes and hyaline cartilage – Bone tissue begins to develop at about this time and eventually replaces most of the existing fibrous or cartilage structures – When a bone develops from a fibrous membrane, the process is intramembranous ossification, and the bone is called a membrane bone – Bone development by replacing hyaline cartilage is called endochondral ossification (endo=within / chondo=cartilage), and the resulting bone is called a cartilage (endochondral) bone Intramembranous Ossification • Results in the formation of cranial bones of the skull (frontal, parietal, occipital, and temporal bones) and the clavicles • All bones formed by this process are flat bones • Four Major Steps: 1, 2, 3, 4 Intramembranous Ossification Intramembranous Ossification Endochondral Ossification • Replaces hyaline cartilage, forming all bones below the skull except for the clavicles • Begins in the second month of development • Five Steps: 1,2,3,4,5 Endochondral Ossification • 1. Initially, osteoblasts secrete osteoid, creating a bone collar around the diaphysis of the hyaline cartilage model Endochondral Ossification Endochondral Ossification • 2. Cartilage in the center of the diaphysis calcifies: – Because calcified cartilage matrix is impermeable to diffusing nutrients, the chondrocytes die and deteriorate forming cavities Endochondral Ossification Endochondral Ossification • 3. The periosteal bud (nutrient artery and vein, lymphatics, nerve fibers, red marrow elements, osteoblast, and osteoclasts) invades the internal cavities and spongy bone forms around the remaining fragments of hyaline cartilage Endochondral Ossification Endochondral Ossification • 4. The diaphysis elongates as the cartilage in the epiphyses continue to lengthen and a medullary cavity forms through the action of osteoclasts within the center of the diaphysis Endochondral Ossification Endochondral Ossification • 5. The epiphyses ossify shortly after birth through the development of secondary ossification centers – When complete, hyaline cartilage remains only at two places: • On the epiphyseal surfaces (articular cartilages) • Junction of the diaphysis and epiphysis, where it forms the epiphyseal plates Endochondral Ossification Postnatal Bone Growth • During infancy and youth: – Long bones lengthen entirely by interstitial growth of the epiphyseal plates – All bones grow in thickness by appositional growth Growth in Length of Long Bones • Side of the epiphyseal plate cartilage facing the epiphysis, the cartilage is relatively quiescent and inactive • Side of the epiphyseal plate cartilage abutting the diaphysis organizes into a pattern that allows fast, efficient growth (osteogenic zone) – As the cells divide the epiphysis is pushed away from the diaphysis • Long bone lengthens LENGTH GROWTH Bone Growth Growth in Length of Long Bones • During growth, the epiphyseal plate maintains a constant thickness because the rate of cartilage growth on its epiphyseal-facing side is balanced by its replacement with bony tissue on its diaphysisfacing side Bone Growth Growth in Length of Long Bones • As adolescence draws to an end, the chondroblasts of the epiphyseal plates divide less often and the plates become thinner and thinner until they are entirely replaced by bone tissue • Longitudinal bone growth ends when the bone of the epiphysis and diaphysis fuses – This process, called epiphyseal plate closure, happens at about 18 years of age in females and 21 years of age in males – However, an adult bone can still increase in diameter or thickness by appositional growth if stressed by excessive activity or body weight Growth in Width (Thickness) • Growing bones widen as they lengthen • Increases in thickness by appositional growth APPOSITIONAL GROWTH Growth in Width (Thickness) • Osteoblast beneath the periosteum secrete bone matrix on the external bone surface – Osteoclasts on the endosteal surface of the diaphysis remove bone • There is normally slightly less breaking down than building up – This unequal process produces a thicker, stronger bone but prevents it from becoming too heavy Appositional Growth Hormonal Regulation of Bone Growth • During infancy and childhood, the most important stimulus of epiphyseal plate activity is growth hormone from the anterior pituitary, whose effects are modulated by thyroid hormone, ensuring that the skeleton has proper proportions as it grows • At puberty, male and female sex hormones (testosterone and estrogen) are released in increasing amounts – Initially these sex hormones promote the growth spurt typical of adolescence, as well as the masculinization or feminization of specific parts of the skeleton – Ultimately these hormones induct the closure of the epiphyseal plate ending longitudinal bone growth BONE HOMEOSTASIS • Every week we recycle 5 to 7% of our bone mass, and as much as half a gram of calcium may enter or leave the adult skeleton each day • Spongy bone is replaced every 3-4 years • Compact bone, is replaced approximately every 10 years – This is fortunate because when bone remains in place for long periods the calcium crystallizes and becomes very brittle—ripe conditions for fracture • When we break bones (most common disorder of bones), they undergo a remarkable process of self-repair Bone Remodeling • In the adult skeleton, bone deposit and bone resorption (removal) occur BOTH at the surface of the periosteum and the surface of the endosteum – These two processes constitute bone remodeling: • They are coupled and coordinated by remodeling units (osteoblasts and osteoclasts) – Osteoblast: bone forming cells – Osteoclast: large cells that resorb or break down bone matrix – In adult skeletons, bone remodeling is balanced bone deposit and removal, bone deposit occurs at a greater rate when bone is injured, and bone resorption allows minerals of degraded bone matrix to move into the blood Bone Remodeling • Bone deposit: involves osteoblasts – Occurs wherever bone is injured or added bone strength is required – Optimal bone deposit requires: • • • • • Healthy diet rich in proteins Vitamin C Vitamin D Vitamin A Minerals: calcium, phosphorus, magnesium, and manganese Bone Remodeling • Bone Resorption: accomplished by osteoclasts – Move along a bone surface, digging grooves called resorption bays as they break down the bone matrix – Secretes: • Lysosomal enzymes that digest the organic matrix • Hydrochloric acid that converts the calcium salts into soluble forms that pass easily into solution – May also phagocytize the demineralized matrix and dead osteocytes Control of Remolding • Regulated by two control loops: – A negative feedback hormonal mechanism that maintains Ca2+ homeostasis in the blood • Calcium is important in many physiological processes: – – – – – Nerve impulses Muscle contraction Blood coagulation Secretion by glands, nerve cells Cell division – Responses to mechanical and gravitational forces acting on the skeleton • Daily calcium requirement is: – 400-800 mg from birth until the age of 10 – 1200-1500 mg from ages 11 to 24 Hormonal Mechanism • Mostly used to maintain blood calcium homeostasis, and balances activity of parathyroid hormone (PTH) and calcitonin (thyroid) Hormonal Mechanism • Increased parathyroid hormone (PTH) level stimulates osteoclasts to resorb bone, releasing calcium to the blood – Osteoclasts are no respectors of matrix age • They break down both old and new matrix • ONLY osteoid (unmineralized matrix), which lacks calcium salts, escapes digestion • As blood concentrations of calcium rise, the stimulus for PTH release ends HORMONE CONTROL Hormonal Mechanism • Calcitonin (Thyroid): – Secreted when blood calcium levels rise – Inhibits bone resorption – Encourages calcium salt deposit in bone matrix, effectively reducing blood calcium levels – As blood calcium levels fall, calcitonin release wanes HORMONE CONTROL REMODELING Hormonal Mechanism • These hormonal controls act not to preserve the skeleton’s strength or well-being but rather to maintain blood calcium homeostasis – In fact, if blood calcium levels are low for an extended time, the bones become so demineralized that they develop large, punched-out-looking holes • Thus, the bones serve as a storehouse from which ionic calcium is drawn as needed Response to Mechanical Stress and Gravity • • Wolff’s Law: Response to mechanical stress (muscle pull) and gravity serves the needs of the skeleton by keeping the bones strong where stressors are acting A bone’s anatomy reflects the common stresses it encounters: – Example: a bone is loaded (stressed) whenever weight bears down on it or muscles pull on it • Tends to bend the bone • Compresses the bone on one side and subjects it to tension (stretching) on the other side – Both forces are minimal toward the center of the bone (cancel each other out) BONE STRESS Wolff’s Law • 1. Long bones are thickest midway along the diaphysis, exactly where bending stresses are greatest (bend a stick and it will split near the middle • 2. Curved bones are thickest where they are most likely to buckle • 3. Trabeculae of spongy bone form trusses, or struts, along lines of compression • 4. Large, bony projections occur where heavy, active muscles attach – Bones of weight lifters have enormous thickenings at the attachment sites of the most used muscles • Also explains the featureless bones of the fetus and the atrophied bones of bedridden people—situations in which bones are not stressed Control of Remolding • Skeleton is continuously subjected to both hormonal influences and mechanical forces • The hormonal loop determines whether and when remodeling occurs in response to changing blood calcium levels • Mechanical stress determines where it occurs • Example: – When bone must be broken down to increase blood calcium levels, PTH is released and targets the osteoclasts – Mechanical forces determine which osteoclasts are most sensitive to PTH stimulation, so that bone in the least stressed areas (temporarily dispensable) is broken down Bone Repair • Fractures are breaks in bones: – Due to trauma to bones or thin, weaken bones Classification of Fracture • Position of the bone ends after fracture: – Nondisplaced: bone ends retain their normal position – Displaced: bone ends are out of normal alignment • Completeness of break: – Complete: bone is broken through – Incomplete: bone is not broken through • Greenstick: bone breaks incompletely (like green twig breaks) – Only one side of the shaft breaks; the other side bends • Orientation of the break relative to the long axis of the bone: – Linear: parallel fracture – Transverse: break is perpendicular to the bone’s long axis Classification of Fracture • Whether the bone ends penetrate the skin: – Open (compound): penetrates the skin – Closed (simple): does not penetrate the skin • Location: – Arm, leg, etc. – Epiphyseal: epiphysis separates from the diaphysis along the epiphyseal plate • Depressed: skull bones pushed in • External appearance • Nature of break: – Comminuted: bone fractures into 3 or more pieces – Spiral: angular Bone Repair • Repair of fractures involves four major stages: – 1. Hematoma formation: mass of clotted blood • Because blood vessels are damaged • Bone cells deprived of nutrients die at the site • Tissue at the site become swollen, painful, and inflamed BONE HEALING Bone Repair • 2. Fibrocartilaginous callus formation: – – – – Formation of soft granulation tissue (soft callus) Capillaries grow into the hematoma Phagocytes invade the area Fibroblasts: • Produce collagen fibers that span the break and connect the bone ends – Osteoblasts: • Begin forming spongy bone BONE HEALING Bone Repair • 3. Bony callus formation: – New bone trabeculae begins to form and is gradually converted to bony (hard) callus BONE HEALING Bone Repair • 4. Remodeling of the bony callus: – Excess material on the diaphysis exterior and within the medullary cavityis removed – Compact bone is laid down to reconstruct the shaft walls BONE HEALING Bone Repair New Methods • • • • 1. Electrical stimulation of fracture 2. Ultrasound treatments 3. Free Vascular fibular graft 4. VEGF: vascular endothelial growth factor • 5. Nanobiotechnology • 6. Bone Substitutes HOMEOSTATIC IMBALANCE • Imbalances between bone deposit and bone resorption underline nearly every disease that affects the adult skeleton Osteomalacia • Soft bones • Includes a number of disorders in adults in which the bone is inadequately mineralized • Osteoid is produced, but calcium salts are not deposited, so bones are soft and weak • Main symptom is pain when weight is put on the affected bones • Cause: insufficient calcium or by a vitamin D deficiency (helps to absorb calcium) • Treatment: drink vitamin D-fortified milk and exposing the skin to sunlight which stimulates production of vitamin D Rickets • Inadequate mineralization of bones in children caused by insufficient calcium or vitamin D deficiency • Treatment: drink vitamin D-fortified milk and exposing the skin to sunlight which stimulates production of vitamin D • Because young bones are still growing rapidly, rickets is much more severe than adult Osteomalacia – Bowed legs, deformities of the pelvis, skull, and rib cage are common Osteoporosis • Refers to a group of disorders in which the rate of bone resorption exceeds the rate of formation • Bones become so fragile that something as simple as a hearty sneeze or stepping off a curb can cause them to break • Bones have normal bone matrix (intercellular material of a tissue), but bone mass is reduced and the bones become more porous and lighter increasing the likelihood of fractures – Spongy bone of the spine is most vulnerable, and compression fractures of the vertebrae are common – Femur, particular the neck, is also very susceptible to fracture (broken hip) Osteoporosis • Older women are especially vulnerable to osteoporosis, due to the decline in estrogen after menopause • Other factors that contribute to osteoporosis include: – – – – – A petite body form Insufficient exercise or immobility to stress the bones A diet poor in calcium and vitamin D Abnormal vitamin D receptors Smoking: • Reduces estrogen levels – Hormone-related conditions: • Hyperthyroidism • Diabetes mellitus OSTEOPOROSIS (a): Normal Bone (b): Osteoporotic Bones Paget’s disease • Is characterized by excessive bone deposition and resorption, with the resulting bone abnormally high in spongy bone – High ratio of spongy bone to compact bones – It is a localized condition that results in deformation of the affected bone • Weaken of a region of a bone • Cause: unknown DEVELOPMENTAL ASPECTS OF BONES: TIMING OF EVENTS • The skeleton derives from embryonic mesenchymal cells, with ossification occurring at precise times – Most long bones have obvious primary ossification centers by 12 weeks • At birth, most bones are well ossified, except for the epiphyses, which form secondary ossification centers • Throughout childhood, bone growth exceeds bone resorption; in young adults, these processes are in balance; in old age, resorption exceeds formation FETAL OSSIFICATION BONE REPAIR