The Economic Impact of the WFI by Dr. Kerry Kuehl
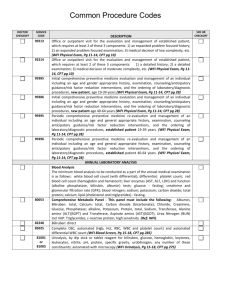
advertisement

Economic Impact of the Wellness Fitness Initiative Kerry Kuehl MD DrPH Department of Medicine Oregon Health & Science University Cost of Injury and Illness In the U.S., total direct and indirect costs associated with work-related injuries and illnesses are > $150 billion or nearly 3 percent of the gross domestic product (Leigh et al., 2000). Injuries are responsible for the majority of those events, with illness accounting for only 15%. These costs are three times that of Alzheimer’s disease and nearly equivalent to the costs for cancer. High Risk Combination Fire fighters have health risks similar to the average American and their work is more physically demanding This combination places FF at high risk for heart disease Leading cause of death fighting fires is heart disease Risks are similar to other Americans 65% > 3 cardiac risk factors 40% > 4 cardiac risk factors 30% 25% 20% Sedentary lifestyle High fat diet Obesity Dyslipidemia Diabetes High blood pressure 15% 10% 5% 0% 0 1 2 3 4 5 6 7 Number of Risk Factors (Combined Data) Background The overall economic impact of workrelated injuries and illness is high. Firefighters are an especially high-risk group for musculoskeletal injuries and other work-related health problems. New means to reduce work-related illness and injury are needed. 8.6X more injuries among FF than private industry Most Hazardous Occupation The fire service is one of the most hazardous occupations. The incidence of work-related injury is eight times that of private industries. NFPA estimated > 80,000 firefighter injuries occurred in the line of duty in 2005. This was an increase of 5.6%, and the highest rate since 2002 (Karter & Molis, 2006). Incidence of FF Injuries Each year, approximately one-third of the more than one million U.S. firefighters sustain a work related injury. National Institute of Standards and Technology (NIST) released a study that estimated the 2002 costs of injuries and efforts to prevent them was from $2.8 billion to $7.8 billion per year (TriData Corporation, 2005). Balance Sheet: $$ OUT WFI:Screening Costs of Testing treadmill stress test physical exam laboratory tests body weight/% fat mental health strength flexibility pulmonary functions dietary history Costs of Follow up (evaluation abnormal results, injuries during testing) Many benefits are long-term and won’t show up on a short term economic analysis. Costs for a Program Balance Sheet: $$ SAVED Comprehensive Medical Lipids Bloodwork BP Aerobic Fitness Lung Function Strength Flexibility Body Comp Questionnaire Testing Only $600 $500$1000 Dollar Costs per Firefighter for Testing Only $500 $400 $300 $200 $100 treadmill stress test physical exam laboratory tests strength $250 flexibility pulmonary functions body weight/% fat dietary history $100 $0 Full Meal Deal Minus Stress Test Labs & Surveys What Level of Testing Is Cost Effective? Cost to diagnose 1 case of hepatitis: $10,000. Cost to diagnose 1 FF with CHD = $100,000. Hepatitis: Quality-Adjusted Life Year (QALY) = $10,000 per QALY for Blood Test. CHD: $100,000 per QALY for Stress Testing. Standard Index for a Cost-Effective Procedure is < $50,000 per QALY. Not Cost-Effective to Stress Test all FF. Follow-up Costs For Abnormal Blood Test – Liver Enzymes Test Number Cost Total Cost Chem-20: 600 30 $11 $75 $6600 $2250 5 $250 $1250 Follow-up Lab Hepatitis Panel To identify 1 case of asymptomatic hepatitis: Total = $ 10,000 Follow-up Costs For Abnormal Stress Tests TEST NUMBER COST TOTAL $$ Stress Test 600 $250 $150,000 Thallium/Echo 70 $1000 $70,000 Cardiologist 10 $250 $2500 Cardiac Cath 10 $2500 (3 Severe CAD) $25,000 Bypass Surgery 2 $25,000 $50,000 Coronary A Stent 1 $7,500 $7500 To identify 3 FF who have severe CAD: Total = $305,000 Considerations of Test Selection Additional follow-up costs must be considered when selecting test In addition to picking the package, consider the risk profile of those being tested Risk Stratification to identify those at high risk is cost effective (i.e., not cost effective to stress test all FF annually) Balance Sheet: IN Short Term and Long Term Benefits Of A Wellness Program WHAT IS THE BOTTOM LINE? Preventing Injury Reducing Costs Decreasing Morbidity and Mortality Business Case For Worksite Wellness Majority of studies show positive ROI ~ $3 Negative studies not published Threats to validity (self selection, low participation, high dropout, effects difficult to measure) Savings about $250/employee at 4 years What about the fire service? Economics of Fire Fighter Wellness Clearly, in other industries, research supports the cost-effectiveness of worksite wellness Wellness programs among fire fighters less obvious One of major roadblocks in preventing fire departments from implementing WFI is concerns about return on investment (ROI) COST OF MAINTENANCE & REPAIR (Percent of Budget) Fire Apparatus Firefighter Maintenance 70% 3% Repair 30% 97% TOTAL 100% 100% Is FF Wellness Cost-Effective? Phoenix: 6 years after implementing wellness program, severity of injuries decreased by 46%. Wichita: 50% reduction in sick leave after implementing fitness program. South Pasadena: Injury rates reduced over 50% after wellness program introduced. PHLAME program in Oregon (retrospective) 35 Injury Rates 30 25 Figure 4: Slope of change (with SEM) for injury rates between PHLAME and Non-PHLAME Fire Bureaus in Oregon as reported in Table 2. Statistical significance is at the p<.0001 level. * rates among PHLAME and Non-PHLAMEPHLAME fire bureaus 20Injury * * 15 * Non-PHLAME * P < .0001 10 5 0 1999 2000 2001 2002 PHLAME Study Year 2003 FD Savings From Reduced Injuries As Compared to 1999 Cost Savings/FF Total (687 FF) 2001 2002 $1353 $1600 $929,511 $1,100,200 IAFF Awards OHSU Grant To Review Economic Impact of Wellness Fitness Initiative In 2006-2007, the original 10 cities WFI task force fire departments contacted Site visits with HR and RM to review data availability diversity, and complexity 8 departments collected long term data with accessible computer data base Retrospective study and data analysis Fire Department Personnel WFI Participation WFI Participation Rate in 1997 Rate in 2004 Austin 1032 CONTROL CONTROL Calgary 983 CONTROL CONTROL Fairfax Co 1280 65% 85% Indianapolis 780 70% 95% LA County 10% 55% Miami-Dade 1900 CONTROL CONTROL Phoenix 1588 70% 90% Seattle 1015 CONTROL CONTROL 3013 Outcome Data Data represents aggregate or average of 4 WFI and 4 Non-WFI fire departments with no ability to identify individual FD claims Occupational Injury/Illness Claims Total Incurred Costs Number of Lost Work Days (LWD) Average Cost Per Claim RESULTS The mean total claims, lost work days, and total incurred costs represent service or occupational benefits paid per fiscal year for a department. Data from these fire departments do not include any non-occupational claims and costs due to difficulty with tracking this information through private insurance and individual medical providers. Occupational Claims Between WFI and Non-WFI Departments Claim Date WFI Claims Non-WFI Claims 1991-1997 Totals 3,033 2,459 1998-2004 Totals 3,210 3,023 Percent Change 5% Increase 22% Increase* *Statistically significant at p<.05 Total Incurred Cost* Between WFI and Non-WFI Departments Claim Date WFI Costs Non-WFI Costs 1991-1997 Totals $21,695,644 $17,055,723 1998-2004 Totals $22,276,143 $26,991,766 Percent Change 3% Increase 58% Increase *Health care costs increased 7% annually past decade Lost Work Days* Between WFI and Non-WFI Departments Claim Date WFI Lost Work Days Non-WFI Lost Work Days 1991-1997 Totals 40,611 26,747 1998-2004 Totals 31,671 41,388 Percent Change 28%Decrease 55% Increase *Some departments had lost hours or did not have lost time calculated Average Cost Per Claim Between WFI and Non-WFI Departments* Claim Date WFI Average Cost / Claim Non-WFI Average Cost / Claim 1991-1997 Totals $56,845 $47,912 1998-2004 Totals $46,225 $64,608 Percent Change -23% Decrease 35% Increase *Calculated from Total Incurred Cost divided by Number of Claims 60% 58% 55% 50% 35% 40% 30% 22% 20% 3% 10% 5% 0% -10% -28% -23% -20% -30% Claims LWD Total Avg Cost Cost per W.F.I Non W.F.I DISCUSSION - COSTS Total incurred costs increased $82,900 per year per WFI department and increased $1,419,435 per Non-WFI fire department per year (adjusted to 2001 dollar amounts). A difference of $1,336,535 per year was saved per WFI fire department as compared to Non-WFI department. CONCLUSION The information presented suggests there is an immediate reduction of occupational injury/illness claims and costs among fire departments that implemented the IAFF/IAFC Wellness Fitness Initiative as compared to fire departments that did not implement the WFI. CONCLUSION The results also demonstrate that the WFI fire departments have a lower rate of increasing claims and costs while decreasing lost work days and average cost per claim. The fact that lost work days and average cost per claim are reduced suggests that injury/illness severity is reduced, especially in the face of rising healthcare costs greater than the rate of inflation. CONCLUSION Adoption of the WFI confers a savings in the short term. Long-term economic benefit will be greater by addition of a health promotion program through prevention and early treatment of fire fighter musculoskeletal injuries, cancer, and cardiovascular disease LIMITATIONS Limitations of this study: Retrospective Data in various sizes, shapes, missing data Dosage effect and participation rate varied Further research with prospective study needed to answer this question of economic benefit of fire fighter wellness. FUTURE DIRECTIONS We have submitted a grant to CDC and NIH in cooperation with the IAFF of a health promotion/injury-reduction program for firefighters utilizing PFT’s with WFI. The proposal builds on prior NIH-funded behavior change research with firefighters including a cost-effective analysis PROSPECTIVE STUDY In addition to workman’s compensation and absenteeism claims, we also will track intervention costs, which might be referred to as opportunity costs, or the costs that would be avoided by forging the intervention. Those include direct cost of the program, salary of labor inputs (interventionists, scheduling personnel), program materials, and management inputs. Addition of PHLAME Behavioral component THANK YOU!