Slide 1 - Vanderbilt University Medical Center

MODERN OBSTETRICS
COMES TO VANDERBILT:
A PERSONAL HISTORICAL
PERSPECTIVE
Frank H. Boehm, M.D.
Birth of Modern Obstetrics
The process leading to significant improvement in the care and outcome of pregnant women and their babies had its birth in the late 1960s and became fully developed in the 1970s.
Maternal Mortality in 1930
670 deaths per 100,000 live births
Maternal Mortality in 1982
7.5 deaths per 100,000 live births
Perinatal Mortality
1940
1965
2004
60/1,000
41/1,000
7/1,000
Infant Mortality
1940
1997
47/1,000
8/1,000
Electronic Fetal Monitoring
1972 – Purchase of 5 EF monitors and a blood gas analyzer at cost of $50K
L & D renamed Fetal Intensive Care Unit
All patients in labor underwent EFM with scalp pH sampling PRN
Monitor conference, Mondays at 4 pm began
Southern Med J
1974; 67:1145.
Contemp Ob/Gyn
1977;9: 57
VANDERBILT OB
1972
60 deliveries per month
Most low-risk patients
AMA - 1971
Adopted a position supporting the regionalization of perinatal care. In
1972, ACOG/AAP developed guidelines on how to evolve regionalization.
Ideally, it was recommended that whenever possible, pregnant mothers should be transferred before delivery, so as to provide the unborn child with the best incubator (the mother's uterus) during transfer.
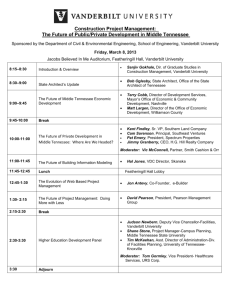
Perinatal Regionalization involved the transfer of high-risk newborns from smaller hospitals to larger, better-equipped and staffed neonatal intensive care units for their care following delivery. It also involved the transfer of high-risk pregnant women to tertiary hospitals, like Vanderbilt, prior to delivery, so they could receive the most sophisticated and advanced treatments available.
It was determined that delivery in a hospital appropriately staffed and equipped for all problems that might arise would result in better outcomes.
Regionalization of perinatal health care required the organization of a region,
(in our case, middle Tennessee), in which there were defined levels of perinatal care consisting of at least one tertiary care (Level 3) hospital, whose primary concerns were education, consultation, transportation and a high level of care.
Level 1 care hospitals (small rural hospitals throughout the 39 counties of middle Tennessee), described care given to normal obstetric patients and normal newborns
Level 2 care described care given for somewhat more complicated pregnancies and newborn illnesses
(Murfreesboro, Clarksville, Columbia,
Cookeville Hospitals).
Being a tertiary care facility, Vanderbilt
University Hospital was able to provide the Level 3 care required for the most complicated and sick pregnant patients and their newborns.
Important aspects of the regionalization process was the prevention of expensive duplication of health care services and staff as well as to provide the most sophisticated and technologically advanced care by highly trained health care providers.
The task for Vanderbilt was to convince doctors and administrators in small rural hospitals throughout surrounding counties of Nashville, to send to
Vanderbilt Hospital their sick newborns, as well as their complicated pregnancies, so that improved outcomes could materialize
Initial telephone calls to practicing
Obstetricians in some of the hospitals around Nashville to explain the benefits of Perinatal Regionalization were not productive.
I soon realized that convincing physicians to transfer care of their patients (and income) to Vanderbilt
Hospital would take a face-to-face encounter in their office, as well as a visit to the administrator of the hospital who would also be affected by a loss of patient care dollars.
With that in mind, I paid a visit to Dr.
Eugene Fowinkle, the then Tennessee
State Commissioner of Health, to ask for his support. I explained the importance of Perinatal Regionalization and how this process would not only save lives, but would also save considerable duplication of equipment and personnel in hospitals throughout the state.
Dr. Fowinkle did not hesitate. He instructed me to write a proposal outlining the costs and said he would do what he could.
Three months later, the State of
Tennessee awarded Vanderbilt's
Ob/Gyn Department $20,000 a year for two years thus allowing me to travel to each hospital in middle Tennessee in hopes of convincing doctors to send their high risk pregnant patients to
Vanderbilt rather than trying to care for them in their local community hospitals.
Convincing doctors to accept Perinatal
Regionalization once I arrived in their picturesque cities, however, was not as pretty.
Local doctors resented Vanderbilt
Hospital for the way some of its staff had treated them whenever they attempted to call for a consult or when they sent a critically ill patient to
Vanderbilt for special care. Many referring doctors explained how physicians at Vanderbilt were often condescending or arrogant when asked their advice.
I was told that when these local doctors did refer patients to Vanderbilt, their patient were lost to follow up. No one at
Vanderbilt, it seemed, made an attempt to inform referring physicians as to what had happened to their patients.
To add insult to injury, I was told of patients having returned home following treatment at Vanderbilt, telling their local doctors of disparaging comments made by
Vanderbilt staff about the care they had received prior to transfer.
It was with this in mind that we began to stress to the many doctors and nurses in the department of Ob/Gyn at
Vanderbilt, the importance of our relationships with referring doctors throughout middle Tennessee.
Insisting on direct Vanderbilt attending physician to referring physician consultation, we were able to gain control of our communication with physicians in middle Tennessee and slowly began to change opinions of our referral base of doctors.
Putting into place a system that emphasized rapid verbal and written communication to keep referring doctors updated on their patients after transport to Vanderbilt, as well as making certain that none of our staff made negative comments concerning care patients had received prior to transfer, was helpful in beginning a process whereby doctors began feeling comfortable referring their complicated pregnant patients to Vanderbilt
Hospital for specialized care.
Unfortunately, not everyone was pleased with our attempts to regionalize the care of pregnant patients.
Slowly and steadily, however, the number of high-risk obstetric patient referral for in-patient care began coming to Vanderbilt Medical Center with numbers reaching as high as 700 each year.
As early as 1981, Vanderbilt was able to report that survival of very small infants born at Vanderbilt Medical
Center had doubled during the years
1975 and 1980
Perinatal mortality (babies dying around the time of birth) in Tennessee, which was 31.2 babies per 1000 births in 1970, steadily declined to 15.8 by
1983.
Maternal mortality (mothers dying because of pregnancy complications) also declined during this time, from 2.9 pregnant patients per 10,000 pregnancies to 1.3.
Am J Obstet Gynecol
1979; 134: 484
J Tenn Med Assoc
1979;72:829
Most doctors and nurses needed an ongoing educational process that would involve on-site education on a regular basis. We needed a team of educators who would travel to hospitals around
Nashville to provide education on the use and interpretation of fetal monitoring.
Our department turned to the March of
Dimes and requested money to hire a nurse specialist who would be able to spend her days traveling throughout middle Tennessee in order to teach nurses the art and science of fetal monitoring.
JOGN Nursing
1981; 141:451
J Gynecol Obstet Nursing
1978;7 :29
J Tenn Med Assoc
1977;70:326
We also requested enough money to purchase Xerox telecopiers for each hospital as well as one for our labor and delivery suite and my home, thereby allowing physicians to transmit strips of their patient's fetal heart rate tracings for rapid consultation
Obstet Gynecol
1973; 42:475
Obstet Gynecol
1979; 53:520
We also began receiving an even larger number of outpatient referrals to the
Vanderbilt Clinics. Patients were being sent to our clinics for consultations on how to manage their complicated pregnancies. Patients requesting genetic counseling and testing increased rapidly as was our need for ultrasound examinations of pregnant women.
Establishment of the
Diabetes Mellitus
Antepartum Clinic
1976
South Med J
1978;71:37
J Perinatology
1985; Vol. V; 1
During this time there did not seem to be anyone in our Vanderbilt Radiology
Department who was interested in the new and very exciting technology of ultrasonography.
We needed someone at Vanderbilt to step forward and help bring this technology to the bedside.
That someone did appear. It was, however, not a faculty member, but rather a very junior resident, Dr. Arthur
Fleischer who came to my office one day to tell me that he understood the capabilities and possibilities of ultrasound.
Radiol
1981; 141: 163
Am J Obstet Gynecol
1981; 141:153
J Tenn Med Assoc
1976;67:33
Obstet Gynecol
1986; 67: 566
Am J Obstet Gynecol
1989;160:586
Obstet Gynecol
1989; 74:338
This desire to deliver a baby in a home like atmosphere was becoming quite popular in many cities around the country. To keep up with this growing demand our obstetric staff requested the hospital administration to open birthing rooms (also called labor, delivery and recovery rooms (LDR)) on our newly constructed labor and delivery floor in the new 11 floor Hospital, which was scheduled to open in the fall of 1980.
Despite what seemed a reasonable request, opposition surfaced. Members of the anesthesia department were expressing concern that LDR rooms might impose an increased risk for laboring patients.
Anesthesiologists, providing pain relief for our laboring patients stated that any patient placed in one of the newly built LDR rooms should not have epidural anesthesia nor be given oxytocin during labor and should not be allowed to have the father of the baby attend the delivery without undergoing an educational process and signing an agreement to abide by a number of rules of behavior.
Fortunately, over time, with the help of print and electronic media, as well as continued pressure from patients, consumer groups and practicing obstetricians, Obstetric
Anesthesiologists were convinced that the
LDR process was a safe and rewarding experience and all of the once placed restrictions on patients wanting a birthing room experience were lifted.
Perinatol Neonatol
1986; 10: 25.
Abortions at Vanderbilt
Roe v Wade 1973
Planned Parenthood 1973 (Sept.)
Director Dr. Angus Crook
Gestational Age Limits 1980
Only Indicated Cases 1980
1978
Creation of Maternal Fetal Medicine
Division
Co-Directors:
Al Killam, M.D and Frank Boehm, M.D.
Fellows Trained
Jeffrey M. Barrett, MD
James E. Brown, MD
Salvatore Lombardi MD
Periclis Roussis, MD
Richard Rosemond, MD
Cornelia Graves, MD
Eric Dellinger, MD
Thomas Wheeler, MD
David Fox, MD
Tracy Papa, DO
Audrey Kang, MD
7/1/80-6/30/82
1/1/84-12/31/86
7/1/86-6/30/88
7/1/88-6/3-/90
7/1/90-6/30/92
7/1/91-6/30/93
7/1/92-6/30/94
7/1/93-6/30/95
7/1/94-6/30/96
7/1/95-6/30/97
7/1/96-6/30/98
Another significant obstacle to advancing the concept of modern obstetrics was our inability to care for obstetric patients in our labor and delivery rooms who were critically ill.
What we needed was the ability to provide this same type of medical intensive care to our pregnant patients on labor and delivery where highly trained obstetric doctors and nurses could continuously provide simultaneous modern obstetric technology with the technology of medical intensive care usually provided in surgical and medical intensive care units in other parts of the hospital.
With this in mind, I asked one of our first year
Maternal Fetal Medicine fellows, Dr. Connie
Graves if she would be interested in learning the art and science of medical and surgical intensive care and help us set up an intensive care unit for critically ill obstetric patients on the labor and delivery floor. After an enthusiastic yes, Dr. Graves began a three month rotation in Vanderbilt's surgical intensive care unit, under the supervision of its Director, Dr. John Morris.
What was also needed, however were obstetric nurses who had interest and skill to also care of these extremely complicated patients. One of our nurses, Nan Troiano, had an interest in this type of intensive care and began the task of selecting a group of obstetric nurses for intensive care training.
Ms Troiano, along with Dr. Graves, trained nurses as well as Ob/Gyn residents on how to properly take care of pregnant women requiring intensive care monitoring and treatment.
Thus began one of the country’s first
Obstetric Intensive Care Units providing care for critically ill pregnant women on a labor and delivery floor.
Dr. Connie Graves and Nan Troiano became Directors of our Obstetric
Intensive Care Unit and began taking care of approximately 50 patients a year.
Critical Care Obstetrics. Dildy GA, ed. 4
th
Ed. 2004; Blackwell; Malden.
Numerous other exciting programs began to surface at Vanderbilt Hospital as a result of the introduction of modern obstetrics. In 1982, the
Department of Obstetrics and
Gynecology received a grant to participate in a multicenter preterm birth prevention project.
Certain unborn babies become severely anemic because of Rh disease and may die as a result. Previous attempts to transfuse these fetuses using x-ray equipment were difficult and frequently unsuccessful.
In 1986, Vanderbilt doctors were able to directly transfuse a fetus while still in its mother's uterus. Real time ultrasound technology allowed doctors to direct a needle into the unborn's umbilical cord and directly transfuse blood into the anemic child with considerable success.
In January 1987, a Hendersonville,
Tennessee woman, Darlene Hawkins, gave birth at Vanderbilt Medical Center to the first quintuplets ever born in
Tennessee
The delivery came 24 weeks into the pregnancy with the babies weighing about 1 1/3 pounds each.
Tragically, only the first born, Stephen, survived, yet the event catapulted
Vanderbilt's Obstetric and Newborn services to a national audience.
We have kept in touch with the Hawkins family and, 16 years after his birth,
Vanderbilt's labor and delivery staff gave Stephen a birthday party at the hospital. Today he is a healthy and delightful young man.
The introduction of a new method for early prenatal testing called CVS
(chorionic villi sampling) made
Vanderbilt a pioneer in the field of early prenatal testing.
We were unwilling, however, to perform
CVS on pregnant patients without first gaining experience.
We therefore, requested that Planned
Parenthood of Nashville allow us to perform this procedure on women who were to undergo an abortion. Fifty patients at Planned Parenthood accepted a monetary gift allowing us the opportunity to perform and perfect this new and innovative procedure.
In 1987 our Obstetric Division began offering CVS to pregnant patients
Am J Obstet Gynecol
1993;168:1766
Since those early days, patients have come to Vanderbilt Medical Center from all parts of Tennessee and surrounding states and we have performed over
3,000 CVS procedures.
In 1987, the Vanderbilt Perinatal Parent
Education Program began formal classes to help children understand pregnancy so they could be prepared to witness the birth of a sibling. Many parents told us that watching siblings being born would be a learning experience for their children and would enhance the feeling of being a part of an important family and life cycle event.
Vanderbilt House Organ
1989
In 1990, doctors at Vanderbilt Medical
Center performed a surgical procedure called a cerclage on a patient who had just delivered an extremely premature twin. This was the first time such an operation, under these circumstances, had been performed in the United
States and it saved the life of a middle
Tennessee newborn.
J Reprod Med
1992;37 :986
In 1990, the Maternal Fetal Medicine
Division recruited Dr. Joseph Bruner to
Vanderbilt Medical Center in order for him to develop a fetal surgery program.
In-utero surgery of the unborn was becoming technologically feasible and a number of birth defects were amenable to surgical correction while the fetus remained in its mother's uterus.
Within seven years, Dr. Bruner and
Pediatric Neurosurgeon, Dr. Noel
Tulipan, performed the first in-utero surgical repair of fetal spina-bifida
This historic event was followed by 178 fetal surgical repairs of spina-bifida at
Vanderbilt Medical Center resulting in the publication of several landmark scientific publications pointing to some improvement in outcome for the newborn.
JAMA
1999;282:1819
The National Institutes of Medicine is now funding and sponsoring a randomized research project along with two other major teaching centers, to ascertain the evidence based scientific value of such a procedure based on rigid research criteria. This study is now in progress.
OC3 began March , 1999 at Vanderbilt
Centralized management of pregnant women infected with the human immunosuppressive virus (HIV) and delivering 150 babies not infected with the AIDS virus during the past 6 years
One of the first Certified Nurse Midwife programs in the area was added to our hospital and now delivers approximately
60 babies each month at Vanderbilt.
Vanderbilt's Division of Maternal Fetal
Medicine began in 1975 a yearly two day seminar called the High Risk
Obstetric Conference.
First guest speaker was Dr. Ed Hon, inventor of the electronic fetal monitor.
It has become the longest running, as well as the most attended, post graduate Obstetric course in America.
Modern obstetrics has improved the lives of countless mothers and babies over the past 34 years. I am confident that in the future the staff at Vanderbilt
Medical Center will continue to combine modern technology with a humane, family oriented approach to childbirth in an attempt to bring and maintain excellence and safety to the process of giving birth.