Schizophrenia PPT
advertisement

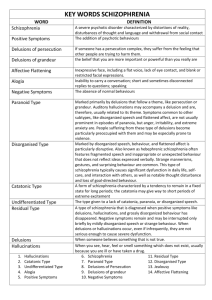
Schizophrenia Chapter 16 Schizophrenia • Fascinated and confounded healers for centuries • One of most severe mental illnesses – 1/3 of population – 2.5% of direct costs of total budget – $46 billion in indirect costs History of Schizophrenia • 1800s - Eugene Kraeplin named it “dementia praecox.” • 1900s - Eugen Bleuler named it schizophrenia (split minds). More than one type. • Kurt Schneider - First rank (psychosis, delusions) and second rank (all other experiences) Schizophrenia Diagnosis • During a one-month period at least two of the five – Positive (delusions, hallucinations, etc.) – Negative (alogia, anhedonia, flat affect, avolition) • One or more areas of social or occupational functioning Types of Schizophrenia Text Box 16.1 • Paranoid • Disorganized • Catatonic • Undifferentiated • Residual Schizophrenia Positive Hallucinations Delusions Disorganization Negative Avolition Alogia Anhedonia Flat Affect Ambivalence Neurocognitive Impairment Attention Memory Exec Function Positive Symptoms: Excess of Normal Functions • Delusions (fixed, false beliefs) – Grandiose – Nihilistic – Persecutory – Somatic • Hallucinations (perceptual experiences) • Thought disorder • Disorganized speech • Disorganized or catatonic behavior Negative Symptoms: Less Than Normal Functioning • Affective blunting: reduced range of emotion • Alogia: reduced fluency and productivity of language and thought • Avolition: withdrawal and inability to initiate and persist in goal-directed behavior • Anhedonia: inability to experience pleasure • Ambivalence: concurrent experience of opposite feelings, making it impossible to make a decision Neurocognitive Impairment • Evidence that neurocognitive impairment exists, independent of positive and negative symptoms Neurocognition • • • • Memory (short-, long-term) Vigilance (sustained attention) Verbal fluency (ability to generate new words) Executive functioning – – – – volition planning purposive action self-monitoring behavior Impaired in schizophrenia • Memory (working) • Vigilance • Executive functioning Neurocognitive Impairment Often Seen as “Disorganized Symptoms” • Confused speech and thinking patterns • Disorganized behavior • Examples of disorganized thinking – – – – – – Echolalia (repetition of words) Circumstantially (excessive detail) Loose associations (ideas loosely connected) Tangentially (logical, but detour) Flight of ideas (change topics) Word salad (unconnected words) Disorganized Symptoms • Examples of disorganized thinking (cont.) – Neologisms (new words) – Paranoia (suspiciousness) – References ( special meaning) – Autistic thinking (private logic) – Concrete thinking (lack of abstract thinking) – Verbigeration (purposeless repetition) – Metonymic speech (interchange words) Disorganized Symptoms • Examples of disorganized thinking (cont.) – Clang association (repetition similar sounding words) – Stilted language (artificial, formal) – Pressured speech (words forced) • Examples of disorganized behavior – Aggression – Agitation – Catatonic excitement (hyperactivity, purposeless activity) Disorganized Symptoms • Examples of disorganized behavior (cont.) – Echopraxia (imitation of others movements) – Regressed behavior – Stereotypy (repetitive, purposeless movements) – Hypervigilance (sustained attention to external stimuli) – Waxy flexibility (posture held in odd or unusual way) Schizophrenia in Children • Rare in children • If appears in children aged 5 or 6, symptoms same as for adults • Hallucinations visual, delusions less well-developed • Other disorders considered first Schizophrenia in Elderly • For those who have had schizophrenia most of their life, this may be a time that they experience improvement in symptoms. • Late-onset schizophrenia – Diagnostic criteria met after 45 – Most likely include positive symptoms Epidemiology • 0.5%-1.5% of population • 300,000 acute episodes each year • Cluster in lower socioeconomic group • Homelessness is a problem. Epidemiology • Across all cultures • In the United States, African Americans have a higher prevalence rate (thought to be related to racial bias). • Men are diagnosed earlier. • EOS: Diagnosed late adolescence • LOS: Diagnosed > 45 years Maternal Risk Factors • Prenatal poverty • Poor nutrition • Depression • Exposure to influenza outbreaks • War zone exposure • Rh-factor incompatibility Infant and Childhood Risk Factors • Low birth weight • Short gestation • Early developmental difficulties • CNS infections Familial Differences • First-degree biologic relatives have 10 times greater risk for schizophrenia. • Other relatives have higher risk for other psychiatric disorders. Comorbidity • Increased risk of cardiovascular disorders • Association between insulin-dependent diabetes and schizophrenia • Depression and pseudodementia • Increased substance abuse • Cigarette smoking • Fluid imbalance Disordered Water Balance • Prolonged periods of polydipsia, intermittent hyponatremia, polyuria • Etiology – unknown • Prevention of water intoxication • Promotion of fluid balance Biologic Factors • Genetic – 10% first-degree relative • Stress-diathesis model proposed by O’Connor • Neuroanatomical findings – Decreased blood flow to left globus pallidus – Absence of normal blood increase in frontal lobes – Atrophy of the amygdala, hippocampus and parahippocampus – Ventricular enlargement • Neurodevelopmental – Prenatal exposure (2nd trimester) – Late winter, early spring births Neurotransmitters, Pathways and Receptors • Hyperactivity of the limbic area (dopamine mesolimbic tract) related to positive symptoms • Hypofrontality or hypoactivity of the prefrontal and neo-cortical areas (dopamine mesocortical tract related to negative and positive symptoms) • Does not result from dysfunction of a single neurotransmitter Psychosocial Theories • Do not explain cause • Disservice to families • Useful in family interaction – Expressed Emotion (EE) • High emotion associated with negative communication and overinvolvement • Low emotion associated with less negativity and less overinvolvement Priority Care Issues • Suicide • Safety of patient and others • Initiate antipsychotic medications Family Response to Disorder • Mixed emotions – shock, disbelief, fear, care, concern and hope • May try to seek reasons • Initial period very difficult Interdisciplinary Treatment • The most effective approach involves a variety of disciplines. • There is considerable overlap of roles and interventions. • Nursing’s contribution is significant. Nursing Management: Biologic Domain Assessment • Present and past health status • Physical functioning • Nutritional assessment • Fluid imbalance assessment • Pharmacologic assessment Medications (prescribed, OTC, herbal, illicit) Abnormal motor movements – DISCUS – AIMS – Simpson-Angus Rating Scale Nursing Diagnosis: Biologic Domain • Self-care deficit • Disturbed sleep pattern • Ineffective therapeutic regimen management • Imbalanced nutrition • Excess fluid volume • Sexual dysfunction Nursing Interventions: Biologic Domain • Promotion of self-care activities – Develop a routine of hygiene activities. – Emphasize its importance; help motivate the patient. • Activity, exercise and nutrition – Help counteract effects of psychiatric medications. – Appetite usually increases, so help with food choices. • Thermoregulation – Teach patient to wear clothing according to weather; dress for winter and summer. – Observe patient’s response to temperature. • Promotion of normal fluid balance – Water intoxication protocol (Text Box 18.5) Pharmacologic Interventions • Newer antipsychotics more efficacious and safer (block dopamine and serotonin) – – – – – – Risperidone (Risperdal) Olanzapine (Zyprexa) Quetiapine (Seroquel) Ziprasidone (Geodone) Aripiprazole (Abilify) Clozapine (Clozaril) - second line • Monitoring and administering medications – – – – Takes 1-2 weeks to work (some improvement immediately) Adequate trial - 6-12 weeks Adherence to prescribe medication is best prevention of relapse. Discontinuation is rare. Pharmacologic Interventions: Monitoring Side Effects • Parkinsonism – Identical symptoms to Parkinson’s – Caused by blockade of D2 receptor in basal ganglia – Treated with anticholinergic medications – Taper anticholinergic meds if discontinued • Dystonia – Imbalance of DA and ACH, with more ACH – Young men more vulnerable – Oculogyric crisis, Torticollis, Retrocollis Monitoring Side Effects • Akathesia – Restlessness, jumping out of skin, uncomfortable – Reduce dose of antipsychotic. – Treat with a -blocker (propranolol). • Tardive Dyskinesia – Impairment of voluntary movement, constant motion – Occurs 6-8 months following initiation of antipsychotics – Facial-buccal area -- lip smacking, sucking, etc. – Movements in trunk, rocking – No real treatment Monitoring Side Effects • • • • • • • Orthostatic hypotension Prolactinemia Weight gain Sedation New-onset diabetes Cardiac arrhythmias (QTc prolongation) Agranulocytosis Drug-drug Interactions • Medications metabolized by 1A2 enzymes include olanzapine and clozapine. • Inhibitors: fluvoxamine (Luvox) • Inducers: cigarette smoking • Medications metabolized by 3A4 include clozapine, quetiapine and ziprasidone. • Inhibitors: ketoconazole, protease inhibitors, erythromycin • Inducer: carbamazapine • Medications affected by 2D6 include risperidone, clozapine and olanzapine. • Inhibitors: fluoxetine, paroxetine (not usually clinically significant) Medication Teaching Points • Consistency in taking medication • Medication and symptom amelioration • Side effects and management • Interpersonal skills that help patient and family report medication effects Medication Emergencies: Neuroleptic Malignant Syndrome • Severe muscle rigidity, elevated temperature • Recognizing symptoms – Elevated temperature, changes in level of consciousness, leukocytosis, elevated creatinine phosphokinase), elevated liver enzymes or myoglobinuria • Nursing interventions – – – – Stop administration of offending medications. Monitor vital signs. Reduce body temperature. Safety, protect muscles Supportive measures – IV fluids – Cardiac monitoring – Dantrolene (Dopamine agonist) Neuroleptic Malignant Syndromes • Acute reaction to dopamine receptors blockers • Prevalence 2 to 2.4% • Death – 4 to 22%, mean = 11% • Etiology: – Drugs block striatal dopamine receptors; disrupt regulatory mechanisms in the thermoregulatory center in hypothalamus and basal ganglia; heat regulation fails and muscle rigidity Medication Emergencies: Anticholinergic Crises • Potentially life threatening, anticholinergic delirium • Can occur in patients who are taking several medications with anticholinergic effects • Elevated temperature, dry mouth, decreased salivation, decreased bronchial, nasal secretion, widely dilated eye • Stop offending drug, usually self-limiting. May use inhibitor of anticholinesterase, physostigmine. Anticholinergic Crisis • Confusion, hallucinations • Physical signs - dilated pupils, blurred vision, facial flushing, dry mucous membranes, difficulty swallowing, fever, tachycardia, hypertension decreased bowel sounds, urinary retention, nausea, vomiting, seizures, coma • Atropine flush • Hot as a hare, blind as a bat, mad as a hatter, dry as a bone Treatment • Self-limiting – three days • Discontinuation of medication • Physiostigmine 1-2 mg IV, an inhibitor of cholinesterase, improves in 24-36 hours • Gastric lavage • Charcoal, catharsis Nursing Management: Psychological Domain Assessment – Responses • Socially stigmatizing • Prodromal symptoms evident (negative symptoms) • Tension and nervousness • Lack of interest in eating • Difficulty concentrating • Disturbed sleep • Decreased enjoyment • Loss of interest, restlessness, forgetfulness • Often not recognized as an illness • Denial common Nursing Management: Psychological Domain Assessment • Positive and negative symptoms • SAPS (positive symptoms) (Box 18.9) • SANS (negative symptoms) (Box 18.10) • PANNS (both symptoms) • Mental status • Appearance • Mood and affect (lability, ambivalence, apathy) • Speech • Thought processes (delusions, disorganized communication, cognitive impairments) • Sensory perception (hallucinations) • Memory and orientation • Insight and judgment • • • • Nursing Management: Psychological Domain Assessment (cont.) Behavioral responses Self-concept Stress and coping patterns Risk assessment – Command hallucinations – Self-injury risk, suicide – Homicide Nursing Diagnosis: Psychological Domain • Disturbed thought processes • Disturbed sensory perceptions • Disturbed body image • Low self-esteem • Disturbed personal identity • Risk of violence, suicide • Ineffective coping • Knowledge deficit Nursing Interventions: Psychological Domain • Counseling, conflict resolution, behavior therapy and cognitive interventions can be used. • Development of nurse-patient relationship – Centers on the development of trust and acceptance of the persons – Critical for optimal treatment of schizophrenia Nursing Interventions: Psychological Domain – Management of Disturbed Thoughts • Assessment content of hallucinations/delusions • Outcomes – Decrease frequency and intensity. – Recognize as symptoms of disorder. – Develop strategies to manage recurrence. • Experiences real to the patient – Validate that experiences are real – Identify meaning and feeling that are provoked • Teach patient that hallucinations and delusions are symptoms of illness. Nursing Interventions: Psychological Domain • Self-monitoring and relapse prevention – Monitor events, time, place, etc. of recurrence of symptoms. – Manage symptoms - getting busy, self-talk, change of activity. (Moller-Murphy Tool) • Enhancement of cognitive functioning – Recognize difficulty in processing information. – Improve attention (computer programs, one-to-one). – Help memory (make lists, write down information). – Improve executive functioning-simulation. Nursing Interventions: Psychological Domain • Behavioral interventions – Organize routine, daily activities. – Reinforce positive behaviors. • Stress and coping skills development – Counseling sessions – Teach and reward positive coping skills. • Patient education – – – – Errorless learning environment Minimal distractions Clear visual aids Skills training Family Interventions • Family support • Educate the family regarding lifelong disorder of schizophrenia. • Emphasize consistent taking of medication. Nursing Management: Social Domain Assessment • Functional status – Assessed initially and at regular intervals – GAF usually used • Social systems – Formal and informal support systems • Quality of life • Family assessment – Family assessment guide (Ch. 16) – Special consideration to the family where patient is the parent Nursing Interventions: Social Domain Promotion of Patient Safety • Monitoring for potential aggression • Administering medication as ordered • Reducing environmental stimulation • Approach to individual patients – Thorough history of violence – Help patient to talk directly and constructively with those with whom they are angry. – Set limits. – Involve patients in formal contracting. – Schedule regular time-outs. Nursing Interventions: Social Domain • • • • Support groups Milieu therapy Psychiatric rehabilitation Family interventions – Encourage to participate in support groups – Inform about local and state resources – Help negotiate provider system Continuum of Care • Treatment occurs across continuum. Patients are at high risk for getting lost in the system. • Inpatient-focused care (stabilization) • Emergency care (crisis) • Community care (most of care) • Mental health promotion