Understanding Personality Disorders
advertisement
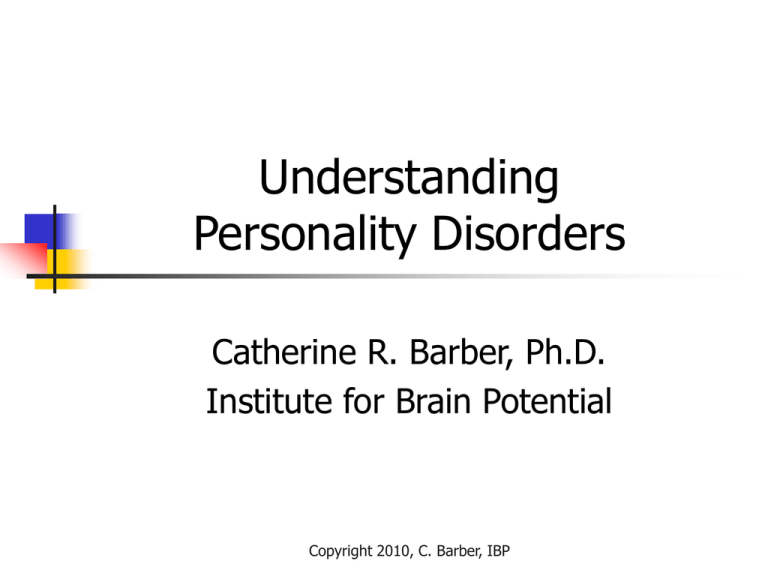
Understanding Personality Disorders Catherine R. Barber, Ph.D. Institute for Brain Potential Copyright 2010, C. Barber, IBP Primary Objectives 1. List key brain regions influencing social reasoning and conduct. 2. Identify features of and effective treatments for paranoid, schizoid, schizotypal, antisocial, borderline, histrionic, narcissistic, dependent, avoidant, obsessive-compulsive, passive-aggressive, and depressive personality disorders. Copyright 2010, C. Barber, IBP Primary Objectives (cont.) 3. Describe personality disorders that may underlie hypochondriasis, body dysmorphic disorder, selected eating disorders, and substance abuse. 4. Review principles that facilitate the transformation of personality. Copyright 2010, C. Barber, IBP Secondary Objectives 1. Differentiate categorical and dimensional models of personality pathology. 2. Describe basic theoretical models of personality disorder etiology. 3. Identify practical strategies for working with personality-disordered clients. 4. Recognize and learn to cope with countertransference. Copyright 2010, C. Barber, IBP Personality Style Consists of the ways in which a person relates to others, world, and self. Traits (internal tendencies – mostly inherited) Habits (behavioral tendencies – mostly learned) These may be adaptive or maladaptive, depending on the context. Copyright 2010, C. Barber, IBP Personality Disorder Enduring and pervasive pattern of perception, thought, and behavior Falls outside social/cultural norms Inflexible and maladaptive Causes impairment or distress Copyright 2010, C. Barber, IBP Disorder or Quirk? No clear line! Some people are just “eccentric.” Level of impairment/distress is usually the determining factor. Example: Grey Gardens Copyright 2010, C. Barber, IBP Models of Personality Pathology Categorical: DSM-IV-TR Dimensional: “Big Five” Prototypical: SWAP Copyright 2010, C. Barber, IBP DSM: A (Mostly) Categorical Model DSM-IV-TR Personality Disorders Cluster A Cluster B Cluster C Paranoid Antisocial Avoidant Schizoid Borderline Dependent Schizotypal Histrionic Obsessive-Compulsive Narcissistic Copyright 2010, C. Barber, IBP What makes DSM categorical? Well-defined criteria Cut-off scores indicate presence/ absence of disorder “Clusters” are based on common features Copyright 2010, C. Barber, IBP DSM: Pros Most widely used system Excellent tool for facilitating communication Easy to use Many categories match well-established clinical syndromes Copyright 2010, C. Barber, IBP DSM: Cons Possibility of multiple diagnoses Overlap in criteria Polythetic criteria set greater heterogeneity within diagnostic categories Cut-offs established by consensus (not empirically) “Reification” trap: Not all categories represent true constructs Copyright 2010, C. Barber, IBP Big Five: A Dimensional Model 5 higher-order personality dimensions Extraversion Agreeableness Conscientiousness Neuroticism/Emotional instability Openness to Experience 30 sub-dimensions Personality disorders are on a continuum with normal personality Copyright 2010, C. Barber, IBP Personality in Two Dimensions Neuroticism Introversion Extraversion Emotional Stability Copyright 2010, C. Barber, IBP Dimensional Model: Pros Empirically-based Dimensions appear to be heritable Provides more information Can be used to predict behavior Recognizes personality strengths (not just pathology) Copyright 2010, C. Barber, IBP Dimensional Model: Cons Can be unwieldy No clear cut-off for determining the presence of disorder Not user-friendly for clinicians who use DSM categories Copyright 2010, C. Barber, IBP SWAP: A Prototypical Model From Westen, Shedler, and Bradley, 2006 Descriptions of personality disorder “prototypes” (similar to DSM descriptions) Clinician rates the degree to which a patient matches the prototype Very good match – patient exemplifies diagnosis Good match – patient has diagnosis Significant match – patient has significant features Slight match – patient has minor features Little or no match – diagnosis does not apply Copyright 2010, C. Barber, IBP Coming (not so) soon to a bookstore near you: DSM-5! Expected to be published ca. 2013 “Best of both worlds”: Dimensional and Prototype models may be included Proposed “types” include antisocial/ psychopathic, avoidant, borderline, obsessive-compulsive, and schizotypal (all pending empirical validation) Copyright 2010, C. Barber, IBP Assessment Tools: Semi-structured Interviews Examples: SCID-II, SIDP-IV, DIB-R Pros: Very thorough Diagnoses generally map onto DSM constructs Highly reliable Cons: May require extensive training Validity is only as good as DSM construct validity Can take a long time to administer Copyright 2010, C. Barber, IBP Assessment Tools: Objective Personality Tests Examples: MMPI-2, PAI, MCMI-III Pros: Empirically-based Self-administered Well-studied Useful for describing and predicting behavior Cons: Not all objective measures provide diagnoses Can be complex to interpret Copyright 2010, C. Barber, IBP Assessment Tools: Projective Tests Examples: Rorschach, TAT, Projective drawings, sentence-completion tests Pros: Especially useful for psychodynamic work May tap unconscious processes Useful for testing defensive clients Cons: More subjective interpretation Do not provide a diagnosis Copyright 2010, C. Barber, IBP Caveats! Gather enough information: Don’t rely on a single encounter to tell you everything about a person’s personality. Don’t diagnose from afar: Beware of the “US Weekly” phenomenon. Not all difficult people have a personality disorder! Copyright 2010, C. Barber, IBP Caveats! Don’t rely on diagnosis alone—a label cannot capture the uniqueness and complexity of the individual. Bottom line on diagnosis and treatment: Try to identify, understand, and address problematic thoughts, emotions, behaviors, motivations, etc., rather than simply assigning a diagnosis. Copyright 2010, C. Barber, IBP A Few More Basics About PDs Community sample prevalence estimates range from 0.5-2.5% to 1015% (10-30% in clinical samples). PDs emerge in childhood/adolescence, but caution is used in diagnosing before 18 years of age. Considerable stigma still attaches to PDs. Copyright 2010, C. Barber, IBP A Few More Basics About PDs Treatment is challenging but not impossible. Treatment involves modification and management of patterns and tendencies, not “cure” of illness. Nature AND nurture appear to cause and contribute to PDs. Copyright 2010, C. Barber, IBP Theories of Personality Disorders Psychodynamic/ Psychoanalytic Theories: Developmental explanations Role of the unconscious Defense mechanisms Example: Object Relations Theory Copyright 2010, C. Barber, IBP Theories of Personality Disorders Cognitive-Behavioral Elements: Automatic thoughts Schemas Cognitive distortions Principles of reinforcement Observation and modeling Copyright 2010, C. Barber, IBP Theories of Personality Disorders Biological elements Everything we do has a biological basis! The brain responds to stimuli—it is constantly receiving and processing information. Both physical and environmental factors cause brain processes to go awry, leading to symptoms. Physical factors: Genetics, head injury, medical diseases Environmental factors: Learning history, trauma Copyright 2010, C. Barber, IBP Theories of Personality Disorders Biological elements Virtually all aspects of brain functioning are involved in personality. Examples: perception, memory, speech, executive functioning, social reasoning, etc. No single region is associated with any personality disorder. However, key regions include the prefrontal cortex and the limbic system. Copyright 2010, C. Barber, IBP Prefrontal Cortex From http://universe-review.ca/I10-80-prefrontal.jpg Executive functioning center Planning Decision making Behavioral activation Behavioral inhibition Reasoning Implementation of plans Copyright 2010, C. Barber, IBP Limbic System From http://www.geocities.com/hotsprings/3468/9/brain-limbic.jpg Cortical and subcortical structures that support and regulate: Emotion Long-term memory Autonomic functions Reward center Copyright 2010, C. Barber, IBP Brain – Behavior Links: Temporal Lobe Epilepsy (TLE) Most frequent form of partial epilepsy in adults. Characterized by abnormal electrical changes in temporal lobe, including amygdala. Emotional disturbances (e.g., fear, anxiety) are common after seizures. Some evidence suggests increase in obsessional traits in TLE. “Interictal” personality is controversial: Minimal evidence suggests a link between other proposed behaviors and epilepsy. Copyright 2010, C. Barber, IBP Brain – Behavior Links: Frontal Lobe Damage Damage to frontal lobes is often associated with disinhibition. Some individuals with frontal lobe damage display “acquired psychopathy.” However, deterioration of moral and social behavior is likely due to damage to other areas in addition to the frontal lobes (e.g., temporal lobes). Copyright 2010, C. Barber, IBP Neurotransmitters and Personality: Serotonin Regulation of mood and behavior Related to appetitive behaviors Low serotonin cravings for sweets and carbohydrates Implications for emotional eating and binge eating Copyright 2010, C. Barber, IBP Neurotransmitters and Personality: Norepinephrine Modulation of basic bodily processes and behavioral tendencies Plays a starring role in the “fight or flight” response (with its relative, epinephrine) Implicated in risk-taking behaviors Involved in the “rush” experience Copyright 2010, C. Barber, IBP Neurotransmitters and Personality: Dopamine Involved in pleasure-seeking and exploratory behaviors Appears to be related to brain’s natural opioids Highly reinforcing when released Also implicated in hallucinations and delusions Copyright 2010, C. Barber, IBP An Integrative Approach Characteristics and prevalence Defense mechanisms Object relational patterns Cognitive schemas Key biological mechanisms Copyright 2010, C. Barber, IBP Cluster A: Odd/Eccentric Paranoid Schizoid Schizotypal Copyright 2010, C. Barber, IBP Paranoid Personality Disorder 0.5-2.5% of general population. (*4.4%) Projection, projective identification, reaction formation. Others are dangerous or “users.” “I’m vulnerable.” More common in relatives with schizophrenia. Copyright 2010, C. Barber, IBP Schizoid Personality Disorder 1.7-4.9% of general population. (*3.1%) Withdrawal, intellectualization. The social world is engulfing. “I’m a misfit.” May be more prevalent in relatives of people with schizophrenia. Copyright 2010, C. Barber, IBP Schizotypal Personality Disorder 0.6-3.3% of the general population. Withdrawal, fantasy. Others are experienced as piecemeal and incoherent. “I am defective.” Dopamine (excess – psychotic symptoms; deficit – cognitive symptoms); ventricular enlargement. Copyright 2010, C. Barber, IBP Cluster B: Dramatic/Emotional Antisocial Borderline Histrionic Narcissistic Copyright 2010, C. Barber, IBP Antisocial Personality Disorder 0.7-1.0% of the general population. (*3.6%) Omnipotent control. Others are selfish, manipulative, and not worthy of respect. “I’m vulnerable.” Serotonin involved in impulse control and aggression; decreased autonomic arousal; overactive pleasure center. Copyright 2010, C. Barber, IBP Psychopathy, ASPD, and Criminality Psychopathy involves: Manipulation and deception Grandiosity Shallow emotions Lack of empathy and remorse Impulsive, irresponsible lifestyle Persistent violation of social norms and expectations People with ASPD may or may not be psychopaths. Many criminals don’t meet criteria for either. Copyright 2010, C. Barber, IBP Borderline Personality Disorder 0.7-1.6% of the general population. (*5%) Splitting, projective identification. Others are unpredictable and inconstant. “I’m defective.” “I’m vulnerable.” “I’m helpless.” “I’m bad.” Serotonin implicated in impulse control and emotion regulation. Differences in brain functioning (reduced response in anterior insula, which senses violation of social norms) less social cooperation/baseline trust. Copyright 2010, C. Barber, IBP Identifying At-risk Youths Developmental Psychopathology Oppositional defiant disorder Conduct disorder Non-suicidal self-injury Copyright 2010, C. Barber, IBP Histrionic Personality Disorder <1.0-2.0% of the general population. Repression, regression, conversion, sexualizing, acting out. Same-sex others are of little value; those of the opposite sex are powerful, exciting, “I’m nothing.” Biological mechanisms unknown. Copyright 2010, C. Barber, IBP Narcissistic Personality Disorder <1.0% of the general population. (*6%; M>F) Subtypes: Malignant/Oblivious, Fragile/Shy/ Hypervigilant Idealization, devaluation. Others are better than I am; I must be better than they are to feel good. “I’m inferior.” Biological mechanisms unknown. Copyright 2010, C. Barber, IBP Cluster C: Anxious/Avoidant Avoidant Dependent Obsessive-Compulsive Copyright 2010, C. Barber, IBP Avoidant Personality Disorder 5.0-5.2% of the general population. (*2.4%) Displacement, projection, rationalization, avoidance. Others who are more powerful can provide safety. “I’m undesirable.” Related to social phobia; dopamine deficits? Copyright 2010, C. Barber, IBP Dependent Personality Disorder 0.6-1.5% of the general population. Regression, reversal. Others are powerful and their care is essential. “I’m helpless.” Biological mechanisms unknown. Copyright 2010, C. Barber, IBP Obsessive-Compulsive Personality Disorder 2.0-2.4% of the general population. (*7.9%) Isolation of affect, reaction formation, moralizing, undoing. Others try to exert control, which must be resisted. “My world can go out of control.” Biological mechanisms unknown. Copyright 2010, C. Barber, IBP Other Problematic Styles Passive-Aggressive (Negativistic) Personality Deny negative emotions while acting them out in a covert or indirect way. Prevalence estimates unreliable (e.g., 20% of adolescents!) Projection, externalization, rationalization, denial. Others require conforming to their rules. “I should only have to do what I want; others’ needs are not as important.” Biological mechanisms unknown. Copyright 2010, C. Barber, IBP Other Problematic Styles Depressive Personality Self-criticism, judgment, intense guilt, dejection. Prevalence estimates unreliable. Introjection, reversal, idealization of others, devaluation of the self. Others will criticize, reject, or abandon. “I am fundamentally bad.” Biological mechanisms unknown. Copyright 2010, C. Barber, IBP Copyright 2010, C. Barber, IBP Common Co-Morbid Conditions Hypochondriasis Involves somatic/physical expression of emotions. Common in people with Histrionic, Dependent, Obsessive-Compulsive PD’s. Functions: obtain attention, keep others close, express emotions. Fears are not easily assuaged by “proof” of no illness. CBT appears to be an effective treatment. Interpersonal function of symptoms must also be addressed; expressive writing may also be helpful. Copyright 2010, C. Barber, IBP Common Co-Morbid Conditions Body Dysmorphic Disorder Involves severely distorted perceptions of one’s appearance Often comorbid with Borderline and Avoidant PD’s Treatment focuses on modifying distorted thoughts and preventing problematic responses. Plastic surgery is rarely effective. Psychopharmacology (especially SSRI’s) may be helpful. Copyright 2010, C. Barber, IBP Common Co-Morbid Conditions Eating Disorders Several diagnoses: anorexia nervosa, bulimia nervosa, binge-eating disorder. Borderline PD is a common diagnosis. Obsessive-compulsive PD may be involved in anorexia. CBT, DBT, family therapy can be helpful. Presence of PD greatly complicates treatment of eating disorders. Copyright 2010, C. Barber, IBP Common Co-Morbid Conditions Substance Abuse A large percentage of people with PD’s abuse substances. Especially common in Antisocial and Borderline PD’s. Presence of PD makes treatment significantly more difficult. Dual diagnosis-focused programs may be most appropriate. Interesting developments in psychopharmacology, e.g., cocaine vaccine. Copyright 2010, C. Barber, IBP Treatment Models Pharmacotherapy Schema Therapy (Young et al.) Mentalization-Based Therapy (Batement & Fonagy) Motivational Interviewing (Miller & Rollnick) Dialectical Behavior Therapy (Linehan) Many others! Copyright 2010, C. Barber, IBP Pharmacotherapy: Benefits Antidepressants Depression, anxiety Common for Clusters B, C Mood stabilizers Mood lability, aggression Common for Cluster B Antipsychotic agents Paranoia, illusions, odd beliefs Common for Clusters A, B Copyright 2010, C. Barber, IBP Pharmacotherapy: Drawbacks Insufficient for changing complex behavior patterns. Polypharmacy is common but carries greater risk. Potential for medication misuse is high. Copyright 2010, C. Barber, IBP Schema Therapy Maladaptive Coping Styles Overcompensation Avoidance Surrender Copyright 2010, C. Barber, IBP Schema Therapy Strategies for change Cognitive Behavioral Experiential Copyright 2010, C. Barber, IBP Mentalization-Based Therapy What is mentalization? How is this different from perspectivetaking? Promoting mentalization through modeling and empathy. Copyright 2010, C. Barber, IBP Motivational Interviewing Stages of Change model Precontemplation Contemplation Preparation Action Maintenance/Relapse Copyright 2010, C. Barber, IBP Motivational Interviewing Resistance is interpersonal (not intrapersonal) “Rolling” with resistance Eliciting and strengthening change talk Help! This sounds like “therapese.” Does this work outside of therapy? Copyright 2010, C. Barber, IBP A Biopsychosocial Framework for Understanding BPD Temperamental vulnerabilities Invalidating environment Emotion dysregulation and its effects on behavior Copyright 2010, C. Barber, IBP Components of DBT Individual psychotherapy Skills training Telephone consultation Case consultation meetings for therapists Ancillary treatments Copyright 2010, C. Barber, IBP The DBT Framework Functions of DBT: Enhance patient capabilities Improve patient motivation Generalize learning to all relevant contexts Structure the environment Enhance therapist capabilities and motivation From Linehan, 1993 Copyright 2010, C. Barber, IBP The DBT Framework Stages of Treatment (and associated goals): Level 1: Behavioral control Level 2: Non-anguished emotional experiencing Level 3: Ordinary happiness and unhappiness Level 4: Capacity for joy and freedom From Linehan, 1993 Copyright 2010, C. Barber, IBP The DBT Framework Stage 1 Target Hierarchy: Decrease life-threatening behaviors Decrease therapy-interfering behaviors Decrease quality of life-interfering behaviors Increase behavioral skills From Linehan, 1993 Copyright 2010, C. Barber, IBP DBT Skills Training Overview Skills Training Target Hierarchy: Reduce therapy-destroying behaviors Increase skill acquisition and strengthen skills Reduce therapy-interfering behaviors From Linehan, 1993 Copyright 2010, C. Barber, IBP DBT Skills Training Overview PROBLEMS in BPD SKILLS in DBT Identity confusion Core mindfulness skills Impulsivity Distress tolerance Emotional instability Emotion regulation Relationship problems Interpersonal effectiveness Self-punishment Self-management Copyright 2010, C. Barber, IBP Core Mindfulness Skills States of Mind Emotion mind Reasonable mind Wise mind From Linehan, 1993 Copyright 2010, C. Barber, IBP Core Mindfulness Skills “What” Skills Observe Describe Participate “How” Skills Non-judgmentally One-mindfully Effectively Copyright 2010, C. Barber, IBP From Linehan, 1993 Interpersonal Effectiveness Involves the balancing act of obtaining/ maintaining: One’s personal objectives (i.e., “wants”) A healthy relationship One’s self-respect From Linehan, 1993 Copyright 2010, C. Barber, IBP Interpersonal Effectiveness Describe Express Assert Reinforce Mindfully Appear confident Negotiate Gentle Interested Validate Easy manner Fair Apologies (no undue) Stick to values Truthful From Linehan, 1993 Copyright 2010, C. Barber, IBP Emotion Regulation Involves managing emotions through: Identifying and labeling emotions Decreasing vulnerability to negative emotions Increasing positive emotions through behavioral activation Decreasing suffering through mindfulness of emotions Changing emotions through opposite action From Linehan, 1993 Copyright 2010, C. Barber, IBP Distress Tolerance Crisis Survival Skills Distraction Self-soothing Improving the moment Pros and cons From Linehan, 1993 Copyright 2010, C. Barber, IBP Distress Tolerance Guidelines for Accepting Reality Observing the breath Half-smile Awareness exercises Radical acceptance Turning the mind Willingness From Linehan, 1993 Copyright 2010, C. Barber, IBP Treatment of PDs: Principles 1. Social Awareness: Help clients recognize and modify maladaptive social behaviors. Self-monitoring – logs, diary cards, etc. Modeling, role-plays Judicious self-disclosure and feedback Copyright 2010, C. Barber, IBP Treatment of PDs: Principles 2. Disabling thoughts: Help clients modify thoughts and beliefs. Identifying automatic thoughts Examining and weighing the evidence Creating alternative, realistic, helpful thoughts Copyright 2010, C. Barber, IBP Treatment of PDs: Principles 3. Attributional Style: Help clients develop optimism. Optimism is associated with better physical health and improved mood. Strategies: Recognizing attributional biases (e.g., fundamental, depressive, borderline) Generating alternative explanations Testing new ideas with behavioral experiments Copyright 2010, C. Barber, IBP Treatment of PDs: Principles 4. Gratitude, empathy, and forgiveness: Help clients give thanks, take perspectives, and let go of grudges. Benefit-finding, focusing on positives, listing assets Mentalizing and perspective-taking Expressive writing about past wrongs Copyright 2010, C. Barber, IBP Treatment of PDs: Principles 5. Self-care: Help clients take care of their physical, emotional, and spiritual needs. Sleep hygiene Nutrition Exercise Productivity and mastery Finding meaning and purpose Copyright 2010, C. Barber, IBP Practical Strategies for the Helping Professions Managing counter-transference Using theory to increase empathy and decrease judgments Avoiding taking things personally Staying attuned to your own behavior and its role in the treatment Using consultation Copyright 2010, C. Barber, IBP Practical Strategies for the Helping Professions Dealing with “difficult” behavior Help-rejecting/resistance Applies to virtually all PD’s Strategies: “Tiffany’s” approach MI strategies Pros and cons Copyright 2010, C. Barber, IBP Practical Strategies for the Helping Professions Dealing with “difficult” behavior The “button radar” Especially common in Antisocial and Borderline PD’s Strategies: Practice acceptance of counter-transference Be curious with the patient about his/her button-pushing Copyright 2010, C. Barber, IBP Practical Strategies for the Helping Professions Dealing with “difficult” behavior Lack of trust Especially common in Paranoid PD and BPD Strategies: Provide objective information Address concerns directly Be as consistent as possible Copyright 2010, C. Barber, IBP Practical Strategies for the Helping Professions Dealing with “difficult” behavior Decreased attachment capacity Especially common in Schizoid and Schizotypal PD’s Strategies: Stay solution-focused (vs process-oriented) Provide a safe environment Engage in rapport-building throughout treatment Copyright 2010, C. Barber, IBP Practical Strategies for the Helping Professions Dealing with “difficult” behavior Attention-seeking Especially common in Histrionic, Narcissistic, and Borderline PD’s Strategies: Use non-pejorative language Refrain from reinforcing undesired behavior Determine motivation and help client find other ways to get needs met Copyright 2010, C. Barber, IBP Practical Strategies for the Helping Professions Dealing with “difficult” behavior Aggression (Active/Passive; others/self) Especially common in Antisocial PD but can be seen in Borderline PD and others Strategies Conduct a thorough risk assessment Create a safety plan Link behavior with consequences and desired goals Copyright 2010, C. Barber, IBP Practical Strategies for (almost) Anyone! Setting limits and boundaries (e.g., contract) Self-monitoring and judicious self-disclosure Providing rationales and practicing non-defensiveness Balancing validation with change Highlighting consequences Encouraging mentalizing Taking an empirical approach Copyright 2010, C. Barber, IBP Conclusions Q&A Evaluation Thanks for attending! Catherine R. Barber, Ph.D. Catherine.Romero.Barber@gmail.com Institute for Brain Potential Copyright 2010, C. Barber, IBP