Holter and Stress Certification Board Worksheet
advertisement
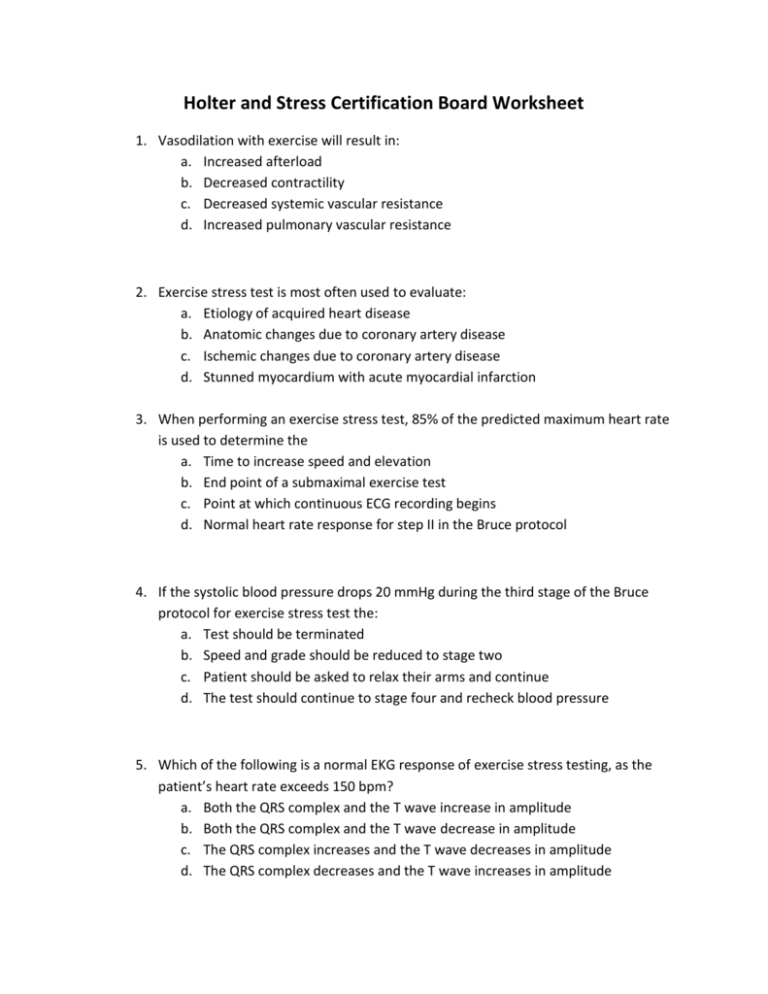
Holter and Stress Certification Board Worksheet 1. Vasodilation with exercise will result in: a. Increased afterload b. Decreased contractility c. Decreased systemic vascular resistance d. Increased pulmonary vascular resistance 2. Exercise stress test is most often used to evaluate: a. Etiology of acquired heart disease b. Anatomic changes due to coronary artery disease c. Ischemic changes due to coronary artery disease d. Stunned myocardium with acute myocardial infarction 3. When performing an exercise stress test, 85% of the predicted maximum heart rate is used to determine the a. Time to increase speed and elevation b. End point of a submaximal exercise test c. Point at which continuous ECG recording begins d. Normal heart rate response for step II in the Bruce protocol 4. If the systolic blood pressure drops 20 mmHg during the third stage of the Bruce protocol for exercise stress test the: a. Test should be terminated b. Speed and grade should be reduced to stage two c. Patient should be asked to relax their arms and continue d. The test should continue to stage four and recheck blood pressure 5. Which of the following is a normal EKG response of exercise stress testing, as the patient’s heart rate exceeds 150 bpm? a. Both the QRS complex and the T wave increase in amplitude b. Both the QRS complex and the T wave decrease in amplitude c. The QRS complex increases and the T wave decreases in amplitude d. The QRS complex decreases and the T wave increases in amplitude 6. In stage three of the Bruce protocol the treadmill is set at: a. 2.4 mph and a 12% grade b. 2.4 mph and a 14% grade c. 3.4 mph and a 12% grade d. 3.4 mph and a 14% grade 7. With exercise, what two factors increase and lead to an increase in cardiac output? a. Heart rate and stroke volume b. Pulmonary and systematic resistance c. Systolic and diastolic blood pressure d. End diastolic and end systolic volumes 8. A positive chronotropic effect will result in: a. A decrease in heart rate b. An increase in heart rate c. A decrease in force of contraction d. An increase in force of contraction 9. Which of the following procedures would you have a patient perform prior to exercise stress testing to rule out normal ST-T wave changes? a. Hyperventilation b. Valsalva maneuver c. Jog in place for three minutes d. Raise arms above head for three minutes 10. Which of the following methods for stress testing would provide the most predictable work load? a. Steps b. Cold pressor c. Pharmacologic d. Bicycle regometer 11. Which of the following is an ABNORMAL response to exercise? a. Decrease ventricular afterload b. Decrease arterial blood pressure c. Decrease in the core temperature d. Decrease systemic vascular resistance 12. Blood pressure from what artery is normally monitored during an exercise stress test? a. Radial b. Femoral c. Brachial d. Popliteal 13. The ability of a positive exercise stress test to correctly identify patients with documented coronary artery disease is known as the test: a. Sensitivity b. Specificity c. Relative risk d. Predictive value 14. The normal electrocardiographic response to exercise is: a. Increase PR and QT interval b. Decrease PR and QT intervals c. Increase PT interval and decrease QT interval d. Decrease PR interval and increase QT interval 15. Which of the following would NOT be an indication to stop an exercise stress test? a. Progressive chest pressure b. Blood pressure reaches 180 mm Hg c. Sustained ventricular tachycardia d. Occasional runs of ventricular premature contractions 16. Which of the following is used in the formula to predict the maximal heart rate for an exercise stress test? a. Age b. Prothrombin time c. Height and weight d. Resting heart rate 17. During an exercise stress test, a 2.0 mm down sloping ST segment was observed six minutes into the Bruce protocol, this would be considered: a. A positive test b. A negative test c. A false positive test d. A false negative test 18. The Bruce protocol for an exercise stress test will: a. Increased speed every two minutes b. Increase grade every two minutes c. Increase speed and grade every five minutes d. Increase speed and grade every three minutes 19. When using Naughton protocol during exercise stress testing, the workload is increased every: a. 2 minutes b. 3 minutes c. 4 minutes d. 5 minutes 20. Which of the following is an absolute contraindication for exercise stress testing? a. Brachyarrhythmias b. Artificial pacemakers c. Patient taking digitals d. Unstable or crescendo angina 21. Why would you have a patient hyperventilate prior to exercise stress testing? a. Evaluate respiratory function and ability b. Document nonspecific S-T, T wave abnormalities c. Determine cerebral vascular response to increased oxygen d. Determine chronotropic effects of increased respiration 22. The purpose in placing one of the exploring leads of the Holter monitor on or near the V5 position is to: a. Minimize QRS configuration b. Minimize atrial depolarization c. Accentuate P wave configuration d. Accentuate ventricular depolarization 23. Somatic tremor is an artifact found in Holter recordings due to: a. An improper ground electrode b. Stress loops that are too tight c. Stress loops that are not secure d. Electrodes being placed over muscle 24. Where would you place the electrodes during a Holter hookup to reduce artifact produced by muscular movements? a. Over the ribs b. Between the ribs c. Low on the arms d. High on the arms 25. What leads are routinely checked to detect left atrial abnormality: a. V1 and V5 b. V4 through V6 c. V1 and Lead II d. Lead III and AVF 26. Patients receiving beta blockers will: a. Increase their R-R interval b. Decrease their R-R interval c. Increase their QRS duration d. Decrease their QRS duration 27. Which of the following drugs would most likely cause a false positive exercise stress test? a. Nitrates b. Digitalis c. Propranolol d. Calcium channel blockers Bonus: 28. A prolonged QT interval due to drug toxicity has an increased risk of: a. Atrial tachyarrhythmias b. Atrial bradyarrhythmias c. Ventricular bradyarrythmias d. Ventricular tachyarrhythmias 29. Atropine is used to control which of the following: a. Bradycardia b. Tachycardia c. Ventricular arrhythmias d. Supraventricular arrhythmias 30. Which of the following drugs is used in the treatment of ventricular arrhythmias? a. Digoxin b. Verapamil c. Lidocaine d. Nitroglycerin 31. Digoxin is commonly used to: a. Increase automaticity b. Decrease automaticity c. Increase contractility d. Decrease contractility 32. Nitrates are commonly used for the treatment of: a. Angina pectoris b. Ventricular arrhythmias c. Supraventricular arrhythmias d. Atrioventricular conduction blocks 33. Beta-blocking drugs will have what effect on heart rate and contractility? a. Increase both heart rate and contractility b. Decrease both heart rate and contractility c. Increase heart rate and decrease contractility d. Decrease heart rate and increase contractility 34. Amiodarone (Cordarone) is useful in the control of: a. Atrial fibrillation b. Ventricular fibrillation c. Atrial premature contractions d. Ventricular premature contractions 35. Which of the following is classified as a Beta Blocker? a. Calan (verapmil) b. Inderal (propranolol) c. Cardizem (Diltiazem) d. Procardia (Nifedipine







![Basic Arrhythmias rev2021 [Autosaved]](http://s1.studylib.net/store/data/025862374_1-2e797b7c05c40a8de1d5ad3bca2f7d13-300x300.png)