ACLS_EKG_Lecture_08
advertisement
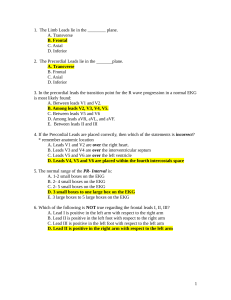
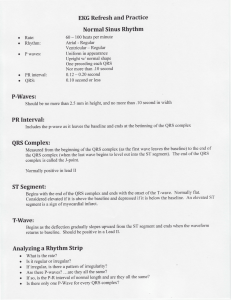
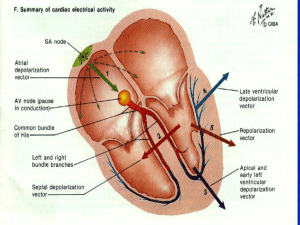
EKG for ACLS AMANDA HOOPER 2008-2009 Let’s start with some basics… V1: right 4th intercostal space V2: left 4th intercostal space V3: halfway between V2 and V4 V4: left 5th intercostal space, mid-clavicular line V5: horizontal to V4, anterior axillary line V6: horizontal to V5, midaxillar line Conduction System of the Heart Sinus node is the pacemaker of the heart, the dominant center of automaticity. Generates continuous regular depolarization stimuli at a rate of 60-100 bpm There are other potential pacemakers that can take over if SA node fails, and they have different intrinsic rates. These are in the atria, AV junction, and the ventricles. EKG Paper EKG machine moves at 25 mm/sec, each small box is 1 mm Small boxes represent 0.04 sec Large boxes represent 0.2 sec Five large boxes equal one second EKG Waves and Intervals P wave: the sequential activation (depolarization) of the right and left atria QRS complex: right and left ventricular depolarization (normally the ventricles are activated simultaneously) ST-T wave: ventricular repolarization PR interval: time interval from onset of atrial depolarization (P wave) to onset of ventricular depolarization (QRS complex) QRS duration: duration of ventricular muscle depolarization QT interval: duration of ventricular depolarization and repolarization Systematic Approach to ECG Interpretation Rate Rhythm Axis Intervals Hypertrophy Infarct (QRST Changes) Determining Rate R-R interval is ventricular rate p-p interval is atrial rate. Usually the same but not always Several ways to do this… 1) Count down the number of large boxes: 300, 150, 100, 75, 60, 50, .... Ex: this one is between 150 and 100, closer to 150 so we might say ~130-140 bpm 2) Count the number of large boxes and divide by 300 Ex: 300/2 = 150 but it is a little slower than that so we might say ~130-140 bpm 3) Count the number of small boxes between beats and divide into 1500 Ex: 1500/11 = 136 bpm Analyzing A Rhythm Strip Is the rhythm regular? What is the rate? Is the QRS complex narrow or wide? Are P waves present? Are P waves related to the QRS complexes? What is the PR interval ? Intervals PR interval From the onset of atrial depolarization to the onset of ventricular depolarization Normal between 0.12 and 0.20 sec—so should be less than a large box QRS interval: Time it takes for ventricular depolarization to occur Normal is 0.10 sec or less—so should be less than half of a large box QT interval From the beginning of ventricular depolarization to the end of ventricular repolarization Normal is les than half of a R-R interval (can’t always rely on this if rate is very tachycardic) Atrial Flutter with 2:1 AV Block Aflutter With Carotid Massage Supraventricular Tachycardia (SVT) Supraventricular rhythms start by definition at or above the AV node. If the QRS is narrow in all leads, you can almost be guaranteed the rhythm is supraventricular. Sinus rhythm, atrial fibrillation, atrial flutter, junctional/nodal rhythms, and PSVT PSVT is a reentry rhythm SVT Myocardial Infarction Look for QRST changes in each lead Note each lead where Q waves are found Look for R wave progression—transition normally occurs between V2 and V4 Look at ST segments and note depression or elevation Look for T wave inversion Q waves or T wave inversion may be a normal finding in leads III, aVF, aVL, aVR, and V1 Basic Lead Groupings Inferior leads: II, III, aVF Lateral (left-sided) leads: V4 to V6 and I, aVL Septal leads: V1, V2 Anterior leads: V2 to V4 Right coronary artery: SA node, IV septum, inferior heart, +/- posterior heart Left coronary artery: LAD- anterior heart Left circumflex- lateral heart 12 EKG with Acute MI Anteroseptal MI Inferior MI with RV Infarction From: Heart Disease 6th Edition. Braunwald E, Zipes D, and Libby P. 2001