Document
advertisement
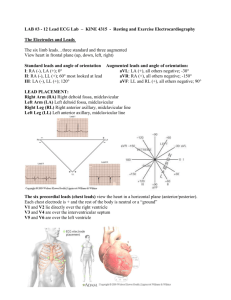
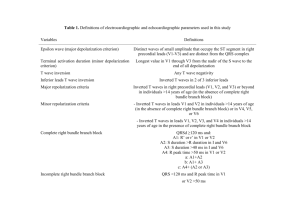
ECG Dr. Bernhard Arianto Purba, M.Kes., AIFO Textbooks • • • • • • Guyton, A.C & Hall, J.E. 2006. Textbook of Medical Physiology. The 11th edition. Philadelphia: ElsevierSaunders: 918-930, 961-977. Brooks, G.A. & Fahey, T.D. 1985. Exercise Physiology. Human Bioenergetics and Sts Aplications. New York : Mac Millan Publishing Company: 122-143. Foss, M.L. & Keteyian, S.J. 1998. Fox’s Physiological Basis for Exercise and Sport. 4th ed. New York : W.B. Saunders Company: 471-491. Astrand, P.O. and Rodahl, K. 1986. Textbook of Work Pysiology, Physiological Bases of Exercise. New York : McGraw—Hill. Braunwald, Pauci, et al.2008. Harrison's PRINCIPLES OF INTERNAL MEDICINE. Seventeenth Edition. New York : McGraw—Hill: Chapter 332, 333, 338. Jardins, Terry Des. 2002. Cardiopulmonary Anatomy & Physiology. The 4th edition. USA: Delmar, A Division of Thomson Learning Inc. ELECTROCARDIOGRAPHY (ECG) ECG A Brief introduction to ECG • • The electrocardiogram (ECG) is a time-varying signal reflecting the ionic current flow which causes the cardiac fibers to contract and subsequently relax. The surface ECG is obtained by recording the potential difference between two electrodes placed on the surface of the skin. A single normal cycle of the ECG represents the successive atrial depolarisation/repolarisation and ventricular depolarisation/repolarisation which occurs with every heart beat. Simply put, the ECG (EKG) is a device that measures and records the electrical activity of the heart from electrodes placed on the skin in specific locations What the ECG is used for? • • • • • • • Screening test for coronary artery disease, cardiomyopathies, left ventricular hypertrophy Preoperatively to rule out coronary artery disease Can provide information in the precence of metabolic alterations such has hyper/hypo calcemia/kalemia etc. With known heart disease, monitor progression of the disease Discovery of heart disease; infarction, coronal insufficiency as well as myocardial, valvular and cognitial heart disease Evaluation of ryhthm disorders All in all, it is the basic cardiologic test and is widely applied in patients with suspected or known heart disease Each small box = 1 mm = .04 Sec. 5 small boxes = 1 large box = 0.2 Sec. MEASURING ECG ECG commonly measured via 12 specifically placed leads Lead Configurations for ECG Measurement n Bipolar Leads Augmented Leads n Chest (V) Leads n Bipolar Leads: lead I + _ + vo _ Bipolar Leads: lead II + _ + vo _ Bipolar Leads: lead III + _ + vo _ ECG Limb Leads Augmented Leads: aVR + _ + vo _ Augmented Leads: aVL + _ + vo _ Augmented Leads: aVF + _ + vo _ ECG Augmented Limb Leads Unipolar Chest Leads v1 v2 v4 v3 v5 v6 v1: fourth intercostal space, at right sternal margin. v2: fourth intercostal space, at left sternal margin. v3: midway between v3 and v4. v4: fifth intercostal space, at mid clavicular line. v5: same level as v4, on anterior axillary line. v6: same level as v4, on mid axillary line. Unipolar Chest Leads (cont.) + _ + _ ECG Precordial Leads Current Lead Placement Conventions (22 Electrodes) H M V9 V8 V7 V3R V6R V5RV4R I E 6R I 5R 3R E Current clinical conventions may use 22 different leads ECG Lead Color Codes C (brown) RA (white) RL (green) LA (black) LL (red) Surface Cardiac Potentials taken at t = to suggests an equivalent dipole located within the heart Eindhoven’s Triangle -very crude solution to inverse problem using bipolar limb leads: _ lead I + RA _ LA _ lead II lead III + + LL NORMAL HEARTBEAT AND ATRIAL ARRHYTHMIA Normal rhythm Atrial arrhythmia AV septum Ventricular depolarization Ventricular depolarization (cont’d) Ventricular depolarization (cont’d) Ventricular repolarization - + - + + -+ + - - + - + - + - +- + - + - + - + + -+ + + + + + Lead I Lead II Lead III Limb Leads Lead I (bipolar) Lead II Lead III aVR aVL aVF Unipolar Lead aVR aVL aVF Normal values Intrinsicoid deflection < 0.05” QT segment Men < 0.39” Wo < 0.40” ST segment Std: > 1mm Pre : > 2mm PR interval 0.12-0.20” P wave 00.8-0.11” U wave QRS duration 0.06-0.10” T wave Precordial leads V6 V1 V2 V3 V4 V5 Horizontal vs Vertical heart Horizontal vs Vertical heart Clockwise vs Counter clockwise rotation 3 4 2 Viewed from below the heart looking towards the apex in vertical heart P wave V1 Atrial Enlarge ment Left atrial enlargement P mitral Wide and notch Biphasic with (-) terminal component V1 Atrial Enlarge ment (cont’d) Right atrial enlargement Tall and peaked P wave Tall and peaked P wave V1 Electrical axis qRS = +3 Lead I qRS = +1 aVF The QRS Bundle of His LBB Anterosuperior division Posteroinferior division RBB The QRS QRS vectors: • Initial depolarization • Terminal depolarization • S-T segmen • Re-polarization 4 2 1 3 V1 V6 Myocardial injury Electrical forces are directed away from a injured area A Normal B Minimal C Subendocard D Transmural E Subepicard Myocardial injury ST segment deviated towards the surface of injured tissue A Normal B Minimal C Subendocard D Transmural E Subepicard Myocardial infarction Zones of myocardial infarction: • Necrosis • Injury • Ischaemia 4 3 2 1 3 1 22 1 3 4 Myocardial infarction (cont’d) ECG parameters of myocardial infarction: • Necrosis • Injury • Ischaemia 4 2 1 3 V1 V6 Myocardial infarction (cont’d) Phases of myocardial infarction: • Hyperacute phase - Slope elevation of the ST sement - Tall widened T wave - Increased ventr. activation time • Fully evolved phase - Pathological Q wave - Coved, elevated ST segment - Inverted symetrical T wave • Old infarction - Pathological Q wave - ST segment and T wave return to normal Myocardial Localization of infarcted areas infarction (cont’d) 2 1 V1 V2 V3 3 II, III, aVF I aVL V4 V5 V6 Right ventri cular hyper trophy 4 2 3 V1 1 V6 Left ventri cular hyper trophy Diatolic overload 4 2 3 V1 1 V6 Left ventri cular hyper trophy Systolic overload 4 2 3 V1 1 V6 RBBB LBBB 1b QT interval Prolonged QTc • Hypocalcemia •Acute rheumatic carditis Shortened QTc • Hypercalcemia • Digitalis effect • Hyperthermia • Vagal stimulation Normal QT does not exclude the diagnosis of QTc= QT R-R • Acute myocardial infarction • Acute myocarditis of any causes • Sympathetic stimulation • Procain effect Atrial Septal Activation Disturbances of impulse formation Sinus rhythms • Sinus arrythmia • Sinus tachycardia • Sinus bradycardia Ectopic atrial rythms • Atrial extrasystole • PAT • Atrial fibrilation • Atrial flutter AV nodal rythms • AVn extrasystole • Paroxysmal AVn tachycardia • Idionodal tachycardia Ventricular rhytms • V-extrasystole • V-tachycardia • V-flutter • V-fibrilation • Idioventricular tachycardia Arrhyth mias Disturbances of impulse conduction A-V block S-A block Reciprocal rythms WPW syndrome (Wolf-Parkinson-White) LGL syndrome (Lawn-Ganong-Levin) Arrhyth mias 2nd disorders of rythms A-V dissociation Atrial escape Aberrant ventricular conduction AVn escape Ventricular escape Arrhyth mias Diagnostic approach To be continued next week Insyaa Allah Arrhyth mias 4 2 3 V1 1 V6 Arrhyth mias 4 2 3 V1 1 V6 Arrhyth mias 4 2 3 V1 1 V6 Arrhyth mias 4 2 3 V1 1 V6 Arrhyth mias 4 2 3 V1 1 V6 Electrocardiogram The Waves P wave atrial depolarization duration 0.11s amplitude < 3mm detects atrial function SA node Electrocardiogram The Waves QRS Complex ventricular depolarization duration 0.10s detects ventricular function Q wave first downward stroke R wave first upward stroke S wave any downward stroke preceded by an upward stroke T wave ventricular repolarization Intervals and Segments PR segment end of P wave to start of QRS measures time of depolarization through AV node PR interval start of P wave to start of QRS measures time from start of SA conduction to end of AV node conduction normal 0.12-0.20s Intervals and Segments ST segment end of QRS complex to start of T wave measures start of ventricular repolarization elevated in MI’s ST interval end of QRS to end of T wave represents complete time of ventricular repolarization QT interval start of QRS to end of T wave duration of ventricular systole < 1/2 of the RR interval Intervals and Segments Intervals the timing for depolarizations/repolarizations can be interpreted from the EKG P-R 0.12-0.2 sec measures the time between the start of atrial depolarization and the start of ventricular depolarization a long P-Q interval is a sign of AV node dysfunction QT interval, about 0.4 sec start of QRS to end of T wave QRS 0.08-0.1 sec wider with ventricular dysfunction ST segment (don’t worry about time) elevated with acute MI Electrocardiogram The waves more on the QRS note that the Q or the R or the S wave is not always present name according to direction of first deflection, second, etc Q waves are often absent lead V1 no Q small R large S lead V2 no Q large R small S Heart Rate Heart Rate defined as beats per minute easy way to estimate rate find an R wave on a thick line count off on the thick lines 300, 150, 100, 75, 60, 50 until you reach another R wave 75 100 150 300 in our example the middle R wave falls on the dark line the next R falls just before the 75, so estimate about 80 bpm Heart Rate Normal Sinus Rhythm heart rate between 60-100 bpm pacing by SA node. QRS after every P wave rhythm is regular Sinus Tachycardia heart rate > 100 bpm p wave is there but hidden by the T wave regular QRS rhythm Sinus Bradycardia heart rate < 60 bpm QRS after every P wave regular rhythm Wave Abnormalities ST segment elevation ischemia Q wave in some leads may indicate ischemia and necrosis T wave inversion late sign of necrosis and fibrosis Rhythm Abnormalities Atrial Fibrillation multifocal areas in atria firing no p waves and irregular heart rate Rhythm Abnormalities Complete (3rd degree) AV Block AV node cannot conduct impulse p waves and QRS not connected irregular heart rate Rhythm Abnormalities Premature Ventricular Contractions ventricles pace early early heart beat large QRS Rhythm Abnormalities Ventricular Tachycardia rapid ventricular pacing rapid, regular rate wide QRS Rhythm Abnormalities Ventricular Fibrillation multifocal ventricular beats irregular won’t last long Axis -90 QRS AXIS + — 180 0 another name for the vector of depolarization an axis is measured in degrees the axis is measured by adding the positive deflection and subtracting the negative deflection overall + is left axis direction overall - is right axis direction for lead one most of the QRS is positive, therefore it has a leftward axis if an MI caused the QRS to be mostly negative the lead would have a rightward axis +90 Axis -90 — 180 0 + +90 QRS AXIS lead II positive on left leg negative on right arm looking at the tracing we see that the QRS is mostly positive what does this mean? Axis -90 — 180 0 + +90 QRS AXIS lead III positive on left leg negative on left arm looking at the tracing we see that the QRS is mostly positive what does this mean? Axis -90 QRS AXIS lead I leftward axis lead II downward axis from this we can see that a normal QRS axis lies somewhere in between 0 and +90 degrees + — 180 0 + +90 remember that infarction will cause the axis to shift rightward (>+90) and that hypertrophy will shift the axis upward (between 0 and -90) The Anatomy of the Heart The Blood Supply to the Heart • Coronary circulation meets heavy demands of myocardium for oxygen, nutrients • Coronary arteries (right, left) branch from aorta base • Anastomoses (arterial interconnections) ensure constant blood supply • Drainage is to right atrium • Great, middle cardiac veins drain capillaries • Empty into coronary sinus Blood Supply to the Heart • Arteries include the right and left coronary arteries, marginal arteries, anterior and posterior interventricular arteries, and the circumflex artery • Veins include the great cardiac vein, anterior and posterior cardiac veins, the middle cardiac vein, and the small cardiac vein SA node activity and atrial activation begin. SA node Time = 0 Stimulus spreads across the atrial surfaces and reaches the AV node. AV node Elapsed time = 50 msec There is a 100-msec delay at the AV node. Atrial contraction begins. AV bundle Bundle branches Elapsed time = 150 msec The impulse travels along the interventricular septum within the AV bundle and the bundle branches to the Purkinje fibers. Elapsed time = 175 msec The impulse is distributed by Purkinje fibers and relayed throughout the ventricular myocardium. Atrial contraction is completed, and ventricular contraction begins. Elapsed time = 225 msec Purkinje fibers Coronary Circulation Coronary Circulation Coronary Circulation Figure 20.9a, b Coronary Circulation Figure 20.9c, d HOLTER MONITOR Technology • • • • • • 5 electrodes 2-3 leads Derived 12 lead available Digital or analog recording Digital transmission to analyzer Requires removal of Holter monitor to scan recording HOLTER MONITOR Uses: • Patients experiencing daily symptoms • Precise quantification of arrhythmias Positives: • 24-48 hours full disclosure available • Heart rate and AF burden graphs • Arrhythmia counts (ex., 10 PVCs per hour)