Female Reproductive System
advertisement
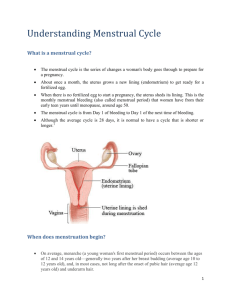
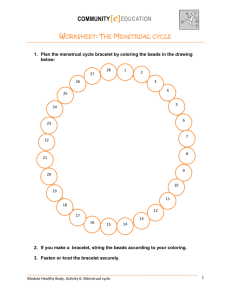
Female Reproductive System Functions Release ovum at puberty Coitus process Implantation in uterus and support of pregnancy (placenta) Parturition and puerperium (uterine involution) Lactation Reproductive organs Ovary Oviduct (Fallopian tubes) Uterus Cervix Vagina External genitalia Fetal Reproductive System Two undifferentiated gonads Two pairs of ducts Urogenital sinus Genital tubercle Vestibular folds Ovary Develop from gonadal cortex During fetal development, oogonia is formed by mitosis followed by meiosis with the production of millions of oocytes Atresia occurs due to hipoxia resulting in less number of oocytes Woman are born with a fix number of oocytes Function – to produce ova and the hormones progesterone and estrogen Oviduct Floats in mesosalpinx Consists of four segments: fimbriae – at the periphery of oviduct, functions to assist in supporting uterus infundibulum – funnel shaped sturcture near ovary, functions to catch ovulated ovum ampulla – distal oviduct and is enlarge , functions as site of fertilization - isthmus – proximal oviduct and is narrow, functions to connect oviduct to uterine cavity Uterus Simplex form in human Three layers – serus membrane, miometrium (thickest) and endometrium Functions for embryo implantation and to support and house fetus throughout pregnancy Cervix Sphincter muscle situated between uterus and vagina Most cervix have annular ring structure Contains goblet cells that secrete mucus and consistency varies with menstrual cycle Mucus consistency can be used to detect fertility Functions to stop entry of bacteria into uterine cavity Cervical canal usually closes, only opens during parturition Cervix also functions to form cervical plug during pregnancy Vagina 1. 2. Divided into 2 parts: Vestibule (external) Posterior vagina (internal) Hymen is a thin connective tissue which forms a transverse fold to partially close vaginal opening in virgins Functions to accept ejaculated semen from penis during coitus Also have an acidic environment to kill bacteria and foreign bodies Can also kill sperm External genitalia Consists of clitoris (small erectile organ at the end of the vulva – contains high number of sensory receptors – organ that causes orgasm – same function as penis and can be erected because has corpus cavernosa tissues), mons pubis, labia majora and minora, vestibular glands and vestibular vagina All these structures are grouped and called vulva Bartolin and vestibular glands secrete mucus for ease of coitus Mons pubis is the part that has the pubic hair Labia majora is the long fold on mons pubis with a labia minora in between Contains fats, smooth muscles, areolar tissue, oil glands and sensory receptors Labia minora has no fatty tissue and is not covered with hair Both labia forms the opening to vagina and urethral opening Oogenesis Process of ovum formation Occurs during fetal stage Primordial germ cells from genital ridge enters gonad to undergo mitosis and produce millions of oogonia, then undergoes meiosis Stops at meiotic prophase at 4N Resumption of meiosis occurs at puberty Folliculogenesis Occurs at puberty Arrested oogonia resumes meiosis Follicles containing the primary oocytes undergoes development to become secondary follicles One follicle becomes the Graffian or tertiary follicle, other follicles may undergo atresia and dies Ovum released from Graffian follicle through a process called ovulation and the production of a first polar body (PB) Remaining follicle left becomes corpus hemarrhagicum then corpus luteum then regress to become corpus albicans Ovum then becomes 2N with the other 2N in Ist PB 1 PB becomes 3 and 4 PB of which each is N Secondary oocyte or ovum once fertilized then will released 2 PB st rd th nd and ovum becomes haplod before fusion with sperm Hormonal influence FSH and LH released from anterior pituitary on directions from Gn-RH from hypothalamus FSH – promotes follicles to grow Mature follicles produces estrogen (granulosa cells) and androgens from thecal cells LH surge comes with positive feedback of high estrogen in blood Ovulation occurs Corpus luteum produces progesterone (P4) to maintain pregnancy if conception occurs, high P4 inhibit FSH release by negative feedback mechanism If not pregnant, prostaglandin 2 from uterus released to kill CL, P4falls and cycle starts all over again Menstrual Cycle Menstrual cycle Normal menstrual cycle - 28 days but cycles with 19 / 35 days still considered normal Cycle not regular at puberty,(maybe long/short, sometimes heavy or light) May get pre-menstrual syndromes - changes in physical and psychological - aggravated by smoking, high salt and sugar diets and caffeine Hygiene is very important during menses Cycle may change if stressed, diseased or change in lifestyle Divided into endometrial cycle and ovarian cycle Hormonal influence FSH and LH released from anterior pituitary on directions from Gn-RH from hypothalamus FSH – promotes follicles to grow Mature follicles produces estrogen (granulosa cells) and androgens from thecal cells LH surge comes with positive feedback of high estrogen in blood Ovulation occurs Corpus luteum produces progesterone (P4) to maintain pregnancy if conception occurs, high P4 inhibit FSH release by negative feedback mechanism If not pregnant, prostaglandin 2 from uterus released to kill CL, P4falls and cycle starts all over again Endometrial cycle Menstrual phase: 1 – 5 days (Dead tissue from endometrial walls sloughed off with blood due to no implantation) Proliferative phase : Day 6-13 (Endometrium starts to thickened due to high levels of estrogen) Secretory phase: Day 14-28 (Thickened endometrial wall with high glycogen deposits and blood vessels (spiral arteries) in anticipation of zygote implantation) Ovarian cycle 1. Follicular phase: Day 1 – 13. FSH and LH release with follicular formation. Mature follicles produces estrogens 2. Ovulatory phase: Day 14. LH surge causes ovulation (release of ovum from follicle) 3. Luteal phase: Day 15 to 28. CL releases progesterone to build endometrium in readiness for implanting zygote Ovulatory Dysfunction 30-40% of female infertility Ovulation requires the coordination of several endocrine glands hypothalamus, pituitary, thyroid, adrenal glands, ovary Disorders of the hypothalamus (anorexia, bulimia, excessive exercise) Disorders of the pituitary (elevated prolactin) Disorders of the ovary: most common causes of ovulatory dysfunction, polycystic ovaries (PCO) Menstrual Cycle Problems Ammenorhea What is amenorrhea? Amenorrhea is a menstrual condition characterized by absent menstrual periods for more than three monthly menstrual cycles. Amenorrhea may be classified as primary or secondary. primary amenorrhea - from the beginning and usually lifelong; menstruation never begins at puberty. secondary amenorrhea - due to some physical cause and usually of later onset; a condition in which menstrual periods which were at one time normal and regular become increasing abnormal and irregular or absent. What causes amenorrhea? Several possible causes of amenorrhea, including: Pregnancy ovulation abnormality - cause of very irregular or frequently missed menstrual periods. birth defect, anatomical abnormality, or other medical condition If a young woman has not started to menstruate by the age of 16, a birth defect, anatomical abnormality, or other medical condition may be suspected. eating disorder Anorexia nervosa and/or bulimia nervosa causes amenorrhea as a result of maintaining a body weight that would be too low to sustain a pregnancy. As a result, as a form of protection for the body, the reproductive system "shuts down" because it is severely malnourished. over-exercise or strenuous exercise Experience absent menstrual cycles due to low body fat content. thyroid disorder Hypothyroidism or hyperthyroidism obesity result of excess fat cells interfering with ovulation Dysmenorrhea What is dysmenorrhea? A menstrual condition characterized by severe and frequent menstrual cramps and pain associated with menstruation. Dysmenorrhea may be classified as primary or secondary. primary dysmenorrhea - from the beginning and usually lifelong; severe and frequent menstrual cramping caused by severe and abnormal uterine contractions. secondary dysmenorrhea - due to some physical cause and usually of later onset; painful menstrual periods caused by another medical condition present in the body (i.e., pelvic inflammatory disease, endometriosis) What causes dysmenorrhea? Primary – due to chemical imbalance in the body (particularly prostaglandin and arachidonic acid - both chemicals which control the contractions of the uterus). Secondary - caused by other medical conditions, most often endometriosis (a condition in which tissue that looks and acts like endometrial tissue becomes implanted outside the uterus resulting in internal bleeding, infection, and pelvic pain). Other possible causes of secondary dysmenorrhea include pelvic inflammatory disease (PID), uterine fibroids abnormal pregnancy (i.e., miscarriage, ectopic), infection, tumors, or polyps in the pelvic cavity Who is at risk for dysmenorrhea? females who smoke, drink alcohol during menses (alcohol tends to prolong menstrual pain), overweight, menstruating before the age of 11 What are the symptoms of dysmenorrhea? Symptoms may include: cramping in the lower abdomen, pain in the lower abdomen, low back pain, pain radiating down the legs, nausea, vomiting, diarrhea, fatigue, weakness, fainting, headaches etc. Pre-menstrual syndrome (PMS) What is premenstrual syndrome? Most females experience some unpleasant or uncomfortable symptoms during their menstrual cycle. Some are significant, some short, some long and disturb normal function. Although the symptoms usually cease with onset of the menstrual period, in some females, symptoms may last through and after their menstrual periods. Who is affected by PMS? 75 % of females, during their reproductive years. What are the symptoms of PMS? psychological symptoms – irritability, nervousness, lack of control, agitation, anger, insomnia, difficulty in concentrating, lethargy, depression, severe fatigue, anxiety, confusion, forgetfulness, decreased self-image, paranoia, emotional hypersensitivity, crying spells, moodiness, sleep disturbances fluid retention - edema (swelling of the ankles, hands, and feet), periodic weight gain, oliguria (diminished urine formation), breast fullness and pain respiratory problems – allergies, infections eye complaints - visual disturbances, conjunctivitis gastrointestinal symptoms - abdominal cramps, bloating, constipation, nausea, vomiting, pelvic heaviness or pressure, backache skin problems – acne, neurodermatitis (skin inflammation with itching), aggravation of other skin disorders, including cold sores neurologic and vascular symptoms – headache, vertigo, syncope (fainting), numbness, prickling, tingling, or heightened sensitivity of arms and/or legs, easy bruising, heart palpitations, muscle spasms Others - decreased coordination, painful menstruation, diminished libido (sex drive), appetite changes, food cravings, hot flashes What causes PMS? - related to fluctuations in estrogen and progesterone levels in the body, hyperprolactinemia, excessive aldosterone, or ADH, carbohydrate metabolism changes, retention of sodium and water by the kidneys, hypoglycemia, allergy to progesterone, psychogenic factors Preventing premenstrual syndrome symptoms: simple lifestyle changes helps to reduce the occurrence of PMS symptoms eg., regular exercise, well-balanced diet (increase their intake of whole grains, vegetables, and fruit, while decreasing their intake of salt, sugar, caffeine, and alcohol). adequate sleep and rest How to diagnose premenstrual syndrome: Complete medical history and physical and pelvic examination, diagnostic procedures for PMS are currently very limited. Knowing your menstrual cycle is very important. Treatment for PMS: Specific treatment for PMS will be determined based on: age, overall health. and medical history, extent of the condition, severity of symptoms, tolerance for specific medications, procedures, or therapies Give prostaglandin inhibitors to reduce pain Sedatives Dietary modifications Vitamin supplements (i.e., vitamin B6, calcium, and magnesium) Regular exercise Antidepressants (or other medications) Infections of the Reproductive Tract Vaginitis – infections of the vagina Most common types of vaginitis: candida or "yeast" infection bacterial vaginosis trichomoniasis vaginitis chlamydia gonococcal vaginitis viral vaginitis noninfectious vaginitis Sexually Transmitted Diseases 20 altogether Common ones – AIDS, Gonorrhea, Chlamydia infections, Trichomoniasis, Syphillis, Genital Herpes, Genital Warts Other diseases that may be sexually transmitted include the following: bacterial vaginosis, chancroid, cytomegalovirus infections, granuloma inguinale (donovanosis), lymphogranuloma venereum, molluscum contagiosum, pubic lice, scabies, vaginal yeast infections