Acid Base Disorders
advertisement

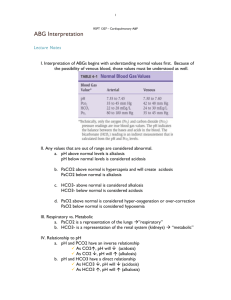
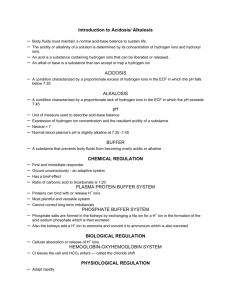
Acid Base Disorders Prof. Tahir Shafi Why should we know about acid base disorders What are acid base disorders How to interpret acid base disorder How to establish the cause Why to worry about acid base disorders Acid base homeostasis fundamental for maintaining life Extreme acidemia or alkalemia can ◦ alter tertiary protein structure affecting enzyme activities ion transport ◦ alter almost every metabolic pathway Extreme acidemia can ◦ depress cardiac function, impair the vascular response to catecholamines, and cause arteriolar vasodilation and venoconstriction, with resultant systemic hypotension and pulmonary edema. Alkalemia can cause ◦ cardiac arrhythmias, neuromuscular irritability, and contribute to tissue hypoxemia. ◦ fall in cerebral and myocardial blood flow ◦ respiratory depression ◦ potassium abnormalities a common accompaniment of acid-base disorders, also contribute to the morbidity. Identification of mild to moderate disorders can give you important clue to the presence of unsuspected but may be otherwise important medical conditions A patient has the following lab tests: ABG pH 7.4 PO2 100 mmHg PCO2 40 Bicarb 24 meq/l Sodium 140 Potassium 4,2 Chloride 80 Bicarb 24 Creatinine 0.9 Glucose 110 Which one of the following statements is correct A. He has normal acid base parameters B. He has metabolic acidosis and respiratory alkalosis C. He has metabolic alkalosis and respiratory acidosis D. He has metabolic acidosis and metabolic alkalosis Regulation of acid base status Acidity in the ECF measured by [H]+ H+ = 38-42 nEq/L Average = 0.00004 mEq/L = 40 nEq/L pH - negative log of H+ in moles Maintenance of arterial pH within normal range 7.38-7.42 with average pH 7.4 Henderson Hasselbach equation Base pH = pk + log Acid 6.1 + log HCO3 24 24 H2CO3 apCO2 1.2 a =0.03 Log 20 1.3 =7.4 Kassirer - Bleich Equation H+ = 24 x pCO2 HCO3 pH and H+ are inversely related h H+ results in i pH - Acidemia i H+ and hpH – Alkalemia Normal pH or H+ - Euphemia Types of acid base disorders Acidosis pCO2 Respiratory Alkalosis H+ = 24 x HCO3 Metabolic Alkalosis Acidosis Stabilization of H+ for every primary disorder there must be physiological compensation by the opposite system Compensations are predictable and can calculated Respiratory compensation H+ = 24 x Primary pH Initial event Met. Acidosis i Met. Alkalosis h pCO2 HCO3 Comp Resp Expected Cpmpensation iHCO3 ipCO2 For 1 meq iHCO3, pCO2 i by 1-1.3 mmHg PCO2 = HCO3+ 15 PCO2 = last 2 digits of pH pCO2 = (HCO3) x 1.5+8+2 Winter’s equation hHCO3 hpCO2 For 1 meq h HCO3,PCO2 h by 0.6 mmHg PCO2 =(HCO3 x 0.9) + 9 PCO2 =(HCO3 x 0.7) + 20 Metabolic compensation H+ = 24 x pCO2 HCO3 Primary pH Initial event Comp Resp Expected Cpmpensation Ac. Resp. Acidosis i hpCO hHCO3 For every 10 mmHg h PCO2 ,HCO3 h by 1 Ch. Resp. Acidosis i hPCO hHCO3 For every 10 mmHg h PCO2, HCO3 h by 3.5 Acute Resp Alkalosis h ipCO iHCO3 For every 10 mmHg i PCO2, HCO3 i by 2 Ch. Resp Alkalosis h ipCO2 iHCO3 For every 10 mmHg i PCO2, HCO3 i by 5 Rates of correction Buffers function almost instantaneously Respiratory mechanisms take several minutes to hours Renal mechanisms may take several hours to days 15 Classification acid base disorders Simple ◦ ◦ ◦ ◦ Metabolic acidosis Metabolic alkalosis Respiratory acidosis Respiratory alkalosis Primary change in one component Secondary change in the other component within physiological range Change in ph in the direction of primary change Mixed ◦ Double Primary change with incomplete or over compensation with other component ◦ Triple ◦ Quadruple Normal acid base homeostasis Metabolic acidosis Exogenous load HCl Other acids Types of metabolic acidosis Addition of acid other than HCl ◦ Serum chloride normal, bicarbonate low ◦ High anion metabolic acidosis Addition of HCl ◦ Serum chloride high, bicarbonate low ◦ Normal anion or hyperchloremic metabolic acidosis Anion gap Albumin is a major source of unmeasured anions! Corrected AG = Observed AG + 2.5 x (4.5 – measured albumin) If serum albumin is high, corrected anion gap will be lower Metabolic Acidosis Causes of high Anion Gap metabolic acidosis K Diabetic Ketoacidosis U S S M A U L Uremia Salicylate intoxication Starvation ketosis Methanol ingestion Alcohol ketoacidosis Unmeasured Osmoles, Ethylene Glycol, Paraldehyde Lactic acidosis MUDPILES Methanol, Uremia, DKA, Paraldehyde, INH/Iron toxicity, Lactic acidodis, Ethanol/Ethlene glycol, Salicylate toxicity Metabolic Acidosis Causes of normal Anion Gap metabolic acidosis H A R D U P Hyperalimentation Acetazolamide Renal tubular acidosis Diarrhoea Uretero sigmoidostomy Pancreatic fistula D – Diarrhea U – Ureteral diversion R – Renal tubular acidosis H – Hyperalimentation A – Acetazolamide M - Miscellaneous (toluene, amphotericin B Hyperchloremic metabolic acidosis Normal or high ammonia excretion Decreased ammonia excretion Urine anion gap Negative urine anion gap positive urine anion gap Urine osmolal gap Measured urine osmolality – calculated urine osmolality Calculated urine osmolality = 2 (UNa + UK )+ Urea 6 < 150 mosm /l= impaired NH4 excretion >150 mosm/l = increased NH4 excretion Urine ammonia level = half urine osmolal gap Metabolic acidosis & osmolal gap Ethyl Alcohol Acetaldehyde Acetic Acid Methyl Alcohol Ethylene Alcohol Glycoaldehyde Glycooxalic acid Oxalic acid OSMOLAL GAP = Measured osmolality- calculated osmolality Normal = < 10-15 mOsmol/Kg of H2O Formaldhyde Formic Acid Glycolic acid Urea BS Calculated serum osmolaliy = 2(Na) + 6 + 18 Metabolic alkalosis Addition of base or loss of acid from body High pH, high bicarbonate, high pCO2 Metabolic alkalosis Saline responsive alkalosis Saline resistant alkalosis Low urinary Cl- (<10 mmol/l) High Urinary Cl- (>10 mmol/l) Normal or low BP Normal BP vomiting Post diuretics After hypercapnia K+ depletion Refeeding alkalosis Bartter’s syndrome Diuretics Mg++ depletion Severe K+ depletion High BP Reno vascular disease Conn’s syndrome Cushing’s syndrome More then one problem? The “gap-gap” or “delta-delta” ratio In the presence of a high AG metabolic acidosis, ? another metabolic acid base disorder Comparing the AG excess to the HCO3 deficit - D AG =D HCO3 D AG = (Observed AG – 12) D HCO3 = (Observed – Normal HCO3) Mixed metabolic acid base disorders Coexistent Metabolic alkalosis delta/delta > 1 hh D AG D HCO3 hh Coexistent Hypercholemic acidosis delta/ delta <1 Mixed metabolic acid base disorders Corrected bicarbonate = observed biacrbonate + D AG > 24 meq/l g Metabolic Alkalosis < 24 meq/l g Metabolic Acidosis Respiratory acid base disorders Respiratory acidosis Hypoventilation H+ = 24 x Respiratory alkalosis Hyperventilation pCO2 HCO3 Primary event Change in pCO2 Respiratory Alkalosis or Acidosis Neuro respiratory control ◦ Central hypo or hyperventilation ◦ Intrinsic lung disease A-a gradient (Alveolar arterial gradient) Alveolar O2 =(760 – 47) * 0.21* PCO2/0.8 =100 Atmospheric pressure – water vapor pressure * FiO2* PaCO2 Arterial (a) =100 A-a gradient normal is < 10 in adults and < 20 in elderly Respiratory Alkalosis Low pCO2, low bicarbonate, high pH ◦ A–a difference >10 mm Hg (>20 mm Hg in elderly) - Hyperventilation with intrinsic lung disease, ventilation–perfusion mismatch, or both (e.g., pneumonia, pulmonary embolism) ◦ A–a difference <10 mm Hg (<20 mm Hg in elderly) Hyperventilation without intrinsic lung disease (e.g., fever, pregnancy) Respiratory Acidosis High pCO2, high bicarbonate, low pH ◦ A–a difference >10 mm Hg (>20 mm Hg in elderly) Hypoventilation with intrinsic lung disease, ventilation–perfusion mismatch, or both (e.g., pneumonia, pulmonary embolism) ◦ A–a difference <10 mm Hg (<20 mm Hg in elderly) - Hypoventilation without intrinsic lung disease (CNS suppression) Approach to Acid Base Disorders History Physical examination Serum electrolytes ◦ Anion gap ◦ Delta/delta ratio Arterial blood gases Urinary electrolytes – Urinary anion gap urine osmolal gap Serum osmolal gap Acid Base Analysis Step 1 : Look at pH. acidemic or alkalemic? Step 2 : Look at pCO2 High – respiratory acidosis Low – respiratory alkalosis Step 3: Look at HCO3 High – metabolic alkalosis Low – metabolic acidosis Step 4: Determine primary event direction of pH Step 5: Is it simple or mixed disorder. compensatory response within physiological range ? Golden rules: 1- Mixed problem present if only one component abnormal 2- Normal pH – both components abnormal 3-Both components in same direction Step 6 : Look at base excess if available Step 7: If the respiratory disturbance is present, is it acute or chronic? Step 8 : Is there increased anion gap? Step 9 : If anion gap increased, calculate corrected HCO3 or delta/delta Step 10 : Calculate osmolal gap if ingestion of alcohols suspected Step 11: Calculate urine anion gap or osmolol gap Acid Base Disorders pH PCO2 HCO3 Na+ ClK+ 7.54 30 mmHg 25 meq/l 140 meq/l 92 meq/l 3.6 meq/l Acid Base Disorders A 55 years old man with renal failure presented with vomiting altered consciousness and fever pH pO2 PCO2 HCO3 Na+ ClK+ 7.25 70 mmHg 40 mmHg 17 meq/l 140 meq/l 89 meq/l 3.6 meq/l A. Respiratory acidosis B. Metabolic Acidosis C. Metabolic alkalosis + respiratory acidosis D. Metabolic acidosis + Respiratory acidosis E. D + Metabolic alkalosis Acid Base Disorders A ss years old man with renal failure presented with vomiting and pleuritic chest pain pH 7.25 pO2 70 mmHg PCO2 40 mmHg HCO3 17 meq/l Na+ 140 meq/l Cl89 meq/l K+ 3.6 meq/l AG 140-(89+17) =34 D AG = 34-10=24 D HCO3 = 24-17=7 High A-a gradient Acid Base Disorders 16 years old boy , a case of FSGS on diuretics and Steroids presented with BP 70/40 mmHg pH 7.4 PCO2 40 mmHg HCO3 24 meq/l Na+ 143 meq/l Cl95 meq/l K+ 3.6 meq/l S. Albumin 1 gram/dl A. no acid base disorder B. Respiratory acidosis C. Metabolic alkalosis + resp acidosis D. Metabolic acidosis + resp alkalosis E, None of the above Acid Base Disorders 16 years old boy , a case of FSGS on diuretics and Steroids presented with BP 70/40 mmHg pH 7.4 PCO2 40 mmHg HCO3 24 meq/l Na+ 143 meq/l Cl95 meq/l K+ 3.6 meq/l S. Albumin 1 gram/dl A. no acid base AG =143-(95+24) = 24 disorder Corrected AG= B. Respiratory acidosis 24+(4-C.Alb) * 2.5 =alkalosis 31.5 Metabolic Delta AG +=resp 21.5acidosis D. Metabolic Delta bicarb = 0 acidosis + resp alkalosis Mixed high anion gap E, None of the above metabolic acidosis + Alkalosis Glucose 90 mg/dl Urea 30 mg/dl Serum Sodium 136 meq/l Serum potassium 4 meq/l Calc osm 291 mosm/l Serum osm 311 mosm/l Osmolar gap =20 delta OG=10 460 mg/l of ethanol or 320 mg/l of methanol Acid Base Disorders HCO3 Na+ ClK+ 17 meq/l 140 meq/l 89 meq/l 3.6 meq/l If delta delta ratio =1 only high AG Met Acidosis Berend K et al. N Engl J Med 2014;371:1434-1445 Berend K et al. N Engl J Med 2014;371:1434-1445 Base Excess = 0.9287 (HCO3 - 24.4 + 14.83 (pH - 7.4)) Predicted pH = 7.4 + pCO2 * 0.08 pH = Actual pH – predicted pH Base Excess = pH *10/0.15 For each 0.15 unit difference in pH Base excess or deficit will be =10 Approach to Acid Base Disorders Traditional or Boston approach Copen Hagen approach ◦ Base excess Stewart / Physiochemical approach ◦ PCO2 ◦ Non-volatile weak ion acid buffer A Total Atotal = A- + AH (Albumin, Pi, SO4, Hb) ◦ Strong ion difference (SID) (Na+K+Ca+Mg) – (Cl+Lac) = A- + HCO3 = 40-42 The physiologic or “Boston” method ◦ uses measurements of arterial pH, pCO2, and [HCO3−] together with an analysis of the anion gap (AG) and a set of compensation rules. 2. The Base Excess (BE) or “Copenhagen” method uses ◦ measurements of arterial pH and pCO2, and calculation of the BE and the AG. 3. The physicochemical or “Stewart” method uses ◦ Measurements of arterial pH and pCO2 together with the calculated apparent (SIDa) and effective (SIDe) “Strong Ion Difference,” the “Strong Ion Gap” (SIG = SIDa-SIDe), and the total concentration of plasma weak acids (Atot).