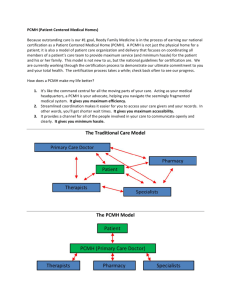
Identify Patients for Care Management
advertisement

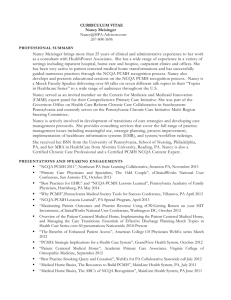
Your Partner in Practice Delving Into PCMH Standards (Working with Elements 3, 4 & 6) OP User’s Conference April 23-25, 2015 © 2015 The Verden Group Agenda Connect the dots in Elements 3 & 4 to understand the requirements Selecting patients for ‘care reminders’ (3D) Selecting patients for ‘clinical decision support’ (3E) A look at Comprehensive Health Assessments (3C) Determining patients for ‘care management’ and managing that care (Element 4A & B) Utilizing the Workbook (3C, 4B, 4C) Setting up performance measurement and quality improvement processes (Element 6) © 2015 The Verden Group Connecting the Dots © 2015 The Verden Group Connecting the Dots 3C reads as if you must implement ‘comprehensive health assessments’ (CHAs) for ALL your patients. You can, but realistically you will use the CHAs for data mining for 3D and 3E, and 4A and 4B. So we start at 3D & 3E and then implement 3C for those ‘conditions’ selected. Connect the dots this way: • • • 3.C (comprehensive health assessments) are used on the patients selected in 3.D and 3.E 3.D (care reminders) • 2 different preventive care services • 2 different immunizations • 3 chronic / acute conditions 3.E (clinical support / evidenced based medicine) • 1 mental health • 1 chronic condition • 1 acute condition • 1 unhealthy behavior condition • 1 well child care © 2015 The Verden Group Connecting the Dots For 4A you use the same patients identified in 3D/E and 4B utilizes the patients ‘discovered’ in 4A. You can also use 3E6 (overuse) and 4A for improvement measures in 6B. Connect the dots this way: • 4.A • • • • (identifying patients needing care management) Behavioral health High cost / utilization Poorly controlled / complex conditions Outside referrals • 4B (care planning & self support) Data mining the patients in 4A, you must utilize the CHAs (3C) to ensure that care planning and self-care support is addressed © 2015 The Verden Group Choosing & Working With Preventive & Acute Care, Immunizations and Overdue Patients for Point of Care Reminders © 2015 The Verden Group PCMH 3D: Use Data for Population Management At least annually practice proactively identifies populations of patients and reminds them, or their families/caregivers, of needed care based on patient information, clinical data, health assessments and evidenced-based guidelines including: 1. 2. 3. 4. 5. At least two different preventive care services.+ At least two different immunizations.+ At least three different chronic or acute care services.+ Patients not recently seen by the practice. Medication monitoring or alert. + Stage 2 Core Meaningful Use Requirement © 2015 The Verden Group PCMH 3D: Scoring MUST-PASS 5 Points Scoring • 4-5 factors = 100% • 3 factors = 75% • 2 factors = 50% • 1 factor = 25% • 0 factors = 0% © 2015 The Verden Group PCMH 3D: Documentation Documentation • F1-5: 1) Reports or lists of patients needing services generated within the past 12 months (Health plan data okay if 75% of patient population) AND 2) Materials showing how patients were notified for each service (e.g., template letter, phone call script, screen shot of e-notice). • Practice must perform these functions at least annually. © 2015 The Verden Group Choosing Preventive Measures Keep it simple and use what’s readily available. OP recommends using: PCMH/OP Reports: Demographic Analysis/Recall Event Chronology PCMH CQMs © 2015 The Verden Group Choosing Preventive Measures © 2015 The Verden Group Choosing Chronic / Acute Services 3 services must be targeted and can be related to only one condition. Chronic care management services consider a practice’s entire population. Practices may focus on three chronic care services related to one condition. Examples in Pediatrics include services related to chronic conditions such as asthma, ADHD, ADD, obesity and depression. Example: One condition, three services could be Asthma • Flu shot reminder • Medication follow up • 6-month visit follow up (newly diagnosed patient) © 2015 The Verden Group Choosing & Working With Conditions and Behaviors for Evidence-Based Decision Support (3E) © 2015 The Verden Group PCMH 3E: Implement Evidence-Based Decision Support The practice implements clinical decision support+ (e.g., point of care reminders) following evidence-based guidelines for: 1. A mental health or substance use disorder. (CRITICAL FACTOR) 2. A chronic medical condition. 3. An acute condition. 4. A condition related to unhealthy behaviors. 5. Well child or adult care. 6. Overuse/appropriateness issues. © 2015 The Verden Group PCMH 3E: Scoring and Documentation 4 Points Scoring • • • • • 5-6 factors (including factor 1) = 100% 4 factors (including factor 1) = 75% 3 factors = 50% 1-2 factors = 25% 0 factors = 0% Documentation • Factors 1-6: Provide Conditions identified by the practice for each factor and Source of guidelines and Examples of guideline implementation © 2015 The Verden Group Developmental and Behavioral: • Mental / substance abuse in Peds • ADHD Depression Substance abuse (tobacco, alcohol, drugs) Condition related to unhealthy behaviors Pediatric Obesity Great resource for information and guidelines: Section on Developmental and Behavioral Pediatrics http://www2.aap.org/sections/dbpeds/screening.asp © 2015 The Verden Group Acute and Chronic Conditions: Focus on chronic or recurring conditions such as asthma, eczema, allergic rhinitis, pharyngitis, bronchiolitis, sinusitis, otitis media and urinary tract infection Some examples OP recommends using: • Asthma • • • Pharyngitis ADD/ADHD Depression Tie them back to your MU measures if you are already making clinical decision support rules © 2015 The Verden Group Well Child Measure: Any age well child visit can be used for this measure. • Utilize Bright Futures as the clinical decision support guidelines. • Protocol templates are included in the OP EMR and based on Bright Futures • Update orders on templates • Adjust Care Plan to meet your practice’s needs © 2015 The Verden Group Overuse / Appropriateness May include ER visits Redundant imaging or lab tests Prescribing generic medications vs. brand name medications Number of specialist referrals. © 2015 The Verden Group Comprehensive Health Assessments (3C) © 2015 The Verden Group PCMH 3C: Comprehensive Health Assessment To understand the health risks and information needs of patients/families, the practice collects and regularly updates a comprehensive health assessment that includes: 1. Age- and gender appropriate immunizations and screenings. 2. Family/social/cultural characteristics. 3. Communication needs. 4. Medical history of patient and family. 5. Advance care planning (NA for pediatric practices). 6. Behaviors affecting health. © 2015 The Verden Group PCMH 3C: Comprehensive Health Assessment (cont.) 7. Mental health/substance use history of patient and family. 8. Developmental screening using a standardized tool (NA for practices with no pediatric patients). 9. Depression screening for adults and adolescents using a standardized tool. 10. Assessment of health literacy. © 2015 The Verden Group PCMH 3C: Scoring 4 Points Scoring • • • • • 8-10 factors = 100% 6-7 factors = 75% 4-5 factors = 50% 2-3 factor = 25% 0-2 factors = 0% NOTE • Factor 5 (NA for pediatric practices) • Written explanation needed for NA responses. © 2015 The Verden Group PCMH 3C: Documentation Documentation • F1-10: Report with numerator and denominator based on all unique patients in a recent three month period indicating how many patients were assessed for each factor. OR • F1-10: Review of patient records selected for the record review required in elements 4B and 4C, documenting presence or absence of information in Record Review Workbook. NOTE: USE THE WORKBOOK! © 2015 The Verden Group Working With Care Management & Support (4A & B) © 2015 The Verden Group PCMH 4: Care Management and Support Intent Meaningful Use Alignment The practice systematically identifies individual patients and plans, manages and coordinates care, based on need. • Practice implements evidence-based guidelines • Practice reviews and reconciles medications with patients • Practice uses eprescribing system • Patient-specific education materials © 2015 The Verden Group PCMH 4: Care Management and Support 20 Points Elements • Element A: Identify Patients for Care Management • Element B: Care Planning and Self-Care Support- MUST PASS • Element C: Medication Management • Element D: Use Electronic Prescribing • Element E: Support Self-Care and Shared DecisionMaking © 2015 The Verden Group PCMH 4A: Identify Patients for Care Management The practice establishes a systematic process and criteria for identifying patients who may benefit from care management. The process includes consideration of the following: 1. Behavioral health conditions. 2. High cost/high utilization. 3. Poorly controlled or complex conditions. 4. Social determinants of health. 5. Referrals by outside organizations (e.g. insurers, health system, ACO), practice staff or patient/family/caregiver. 6. The practice monitors the percentage of the total patient population identified through its process and criteria. (CRITICAL FACTOR) © 2015 The Verden Group Identifying Patients for Care Management • Identify all patients in practice with conditions referenced in 4A, Factors 1-5. • Patients may “fit” more than one criterion (Factor). • Patients may be identified through electronic systems (registries, billing, EHR), staff referrals and/or health plan data. • Review comprehensive health assessment (Element 3C) as a possible method for identifying patients. • Factor 6 is critical - NO points if no monitoring The concept is to use 3C: CHAs, to help identify these patients. © 2015 The Verden Group PCMH 4A: Scoring and Documentation 4 Points Scoring • • • • • 5-6 factors (including factor 6) = 100% 4 factors (including factor 6) = 75% 3 factors (including factor 6) = 50% 2 factor (including factor 6) = 25% 0-1 factors (or does not meet factor 6) = 0% Documentation • F1-5: Documented process describing criteria for identifying patients for each factor • F6: Report with - Denominator = total number of patients in the practice - Numerator = number of unique patients identified in denominator as likely to benefit from care management. © 2015 The Verden Group 4A1: Behavioral Health Pediatric populations Practices may identify children and adolescents with special health care needs, defined by the U.S. Department of Health and Human Services Maternal and Child Health Bureau (MCHB) as children “who have or are at risk for chronic physical, developmental, behavioral or emotional conditions and who require health and related services of a type or amount beyond that required generally.” (Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, American Academy of Pediatrics, 3rd Edition, 2008, p. 18.) © 2015 The Verden Group PCMH 4B: Care Planning and Self-Care Support Care team and patient/family/caregiver collaborate (at relevant visits) to develop and update an individual care plan that includes the following features for at least 75 percent of the patients identified in 4A. 1. Incorporates patient preferences and functional/ lifestyle goals. 2. Identifies treatment goals. 3. Assesses and addresses potential barriers to meeting goals. 4. Includes a self-management plan. 5. Is provided in writing to patient/family/caregiver. © 2015 The Verden Group 10 PCMH 4B: Scoring and Documentation 4 Points Scoring • • • • • 5 factors = 100% 4 factors = 75% 3 factors = 50% 1-2 factors = 25% 0 factors = 0% Documentation • F1-5: Submission of Record Review Workbook and Examples of how each factor is met (e.g. copy of a care plan) © 2015 The Verden Group Using the Record Review Workbook © 2015 The Verden Group Workbook © 2015 The Verden Group Determining What & How to ‘Measure & Improve’ © 2015 The Verden Group PCMH 6: Measure and Improve Use all the same measures from Element 3D! © 2015 The Verden Group PCMH 6A4: Vulnerable Populations 4. Performance data stratified for vulnerable populations (to assess disparities in care). • The data collected by the practice for one or more measures from factors 1–3 is stratified by race and ethnicity or by other indicators of vulnerable groups that reflect the practice’s population demographics, such as age, gender, language needs, education, income, type of insurance (i.e., Medicare, Medicaid, commercial), disability or health status. • Vulnerable populations are “those who are made vulnerable by their financial circumstances or place of residence, health, age, personal characteristics, functional or developmental status, ability to communicate effectively, and presence of chronic illness or disability,” (AHRQ) and include people with multiple co-morbid conditions or who are at high risk for frequent hospitalization or ER visits. © 2015 The Verden Group 6A – Identifying Vulnerable Populations Also look back to 4A to help determine ‘vulnerable’ patients. They may include: • • • • • • • • High level of resource use e.g. visits, medication, calls Frequent visits for urgent or emergent care (2 or more visits in the last 6 months) Frequent hospitalizations (2 or more in the last year) Multiple co-morbidities, including mental health Non-compliance with treatment or medications Terminal illness Multiple risk factors Psychosocial status, lack of social or financial support that impedes ability for care © 2015 The Verden Group PCMH6B: Resource Use Look back to 4A2 for utilization measures affecting costs. © 2015 The Verden Group PCMH 6D: Implement Continuous QI Utilize previous measures: 3D, 3E tracked to 6A and 4A2 to 6B – reuse and recycle! 6D flows to 6E MUST PASS! © 2015 The Verden Group PCMH6C: Continuous Improvement The practice sets goals and acts to improve performance, based on clinical quality measures (Element A), resource measures (Element B) and patient experience measures (Element C). The goal is for the practice to reach a desired level of achievement based on its selfidentified standard of care. • 6A ties to 3D and 3E • 6B ties to 4A2 USE the ‘Quality Measurement and Improvement Worksheet’ © 2015 The Verden Group PCMH 6C: NCQA Quality Measurement and Improvement Worksheet © 2015 The Verden Group PCMH 6C: NCQA Quality Measurement and Improvement Worksheet © 2015 The Verden Group Q&A Contact Information The Verden Group, Inc Your Partner in Practice www.TheVerdenGroup.com Susanne Madden, MBA, NCQA CEC madden@theverdengroup.com Julie Wood, MSc, NCQA CEC julie@theverdengroup.com © 2015 The Verden Group