Diapositiva 1 - WordPress.com
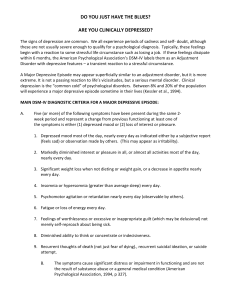
advertisement

1st CME Mood Disorders Anne Washington Derry (1927) Oil on canvas by Laura Wheeler Waring(1887 - 1948) Assumption No dichotomy between mind and body/ mind and brain All mental processes, even the most complex psychological processes, derive from operations of the brain. The central tenet of this view is that what we commonly call mind is a range of functions carried out by the brain. (Kandel, 1998) René Descartes: Res Cogitans VS Res Extensa Biopsychosocial model Engel (1977) Social factors Biological factors Psychological factors Mental Status Examination • Appearance (hygiene, dressing) • Behavior (psychomotor acitivity) – Cooperation/ Attitude • Speech (to much, dysartric, disorganized, prosody) • Thought Process/Form (Circumstantiality, Tangentiality, flight of ideas, Idiosyncracies, loose of association) • • • • • Thought Content (delusions, obsessions) Perceptions (illusion, hallucinations) Mood and Affect Insight and Judgment Cognitive Functioning and Sensorium Mood Disorders: Prevalence Disorders Major Depression Dysthymia Bipolar I Biploar II Prevalence 4.9% 3.2% 0.8% 0.5 MDD (Postpartum) 13% Kenian Data Our data Depression longer: 18,6 months = 1,5 years Association with gastric pain and headache Mood Disorders (DSM-IV) • Depressive Disorders -Major Depressive Disorder -Dysthymic Disorder -Depressive Disorder, Not otherwise specified • Bipolar Disorders -Bipolar I Disorder -Bipolar II Disorder -cyclothymic Disorder 1) Major Depressive Disorder Diagnostic Criteria for Major Depressive Episode: A) 5 of following symptoms, must include one of first two, occurred almost every day for two weeks • Depressed mood • Pleasure or interest/ Loss • Appetite • Sleep disturbance, too much or too little • Agitation or retardation • Fatigue • Feelings of worthlessness or guilt • Difficulty concentrating or deciding • Recurrent thoughts of death, suicide C) Significant distress or impairment in social, occupational or other important areas of functioning D) Exclusion effect of: - Substance: drugs, medications (benzodiazepines, beta-blockers, narcotics and steroids - general medical condition (es. Hypothyroidism, diabetes, cancer) E) Not better account by a bereavement (only after 2 months or with marked impairement) Other sintoms of depression • Mood irritable gastrits, headache, backpa • Less libido • Somatic complains: persistent pain, strange sensation in the head like warms, insects DSM modified criteria for Sub-saharian Africa (Berstchy et al., 1992) • Diziness, fainting, loose of memory • Paranoid ideas (persecution) Major Depressive Disorder MDD, Single episode • 1 major depressive episode • Absence of mania or hypomania MDD, Recurrent • 2 major depressive episodes, separated by at least a 2 month period with more or less normal functioning/mood Major Depressive Disorder: Etiological Theories • Biological (genetic, brain structures, neurotransmitters) 30 % Genetic power • Behavior and cognition • Emotion • Social and cultural factors • Developmental factors • Life events Depression is a sistemic disorder Mood depression BIOLOGICAL BASIS 5HT - NEDA neurotrasmettitorial HPA - HPT hormonal NK - IL immunological BDNF - NGF neurotrophic Major Depression - Treatment • Farmacotherapy: Antidepressants • Psychotherapy (Behavioural,Cognitive, interpersonal, dinamic) Combined! • Electroconvulsive therapy (ECT) • Vagal Nerve Stimulation Preliminary assessment Identified patients at risk: - family or personal history of depression - multiple medical problems - unexplained physical symptoms - chronic pain - use of medical services that is more frequent than expected Sex: + F - Trauma or hard life events + Middle Age • Have you been consistently depressed or down, most of the day, nearly every day, for the past 2 weeks? NO YES • In the past 2 weeks, have you been much less interested in most things or much less able to enjoy the things you used to enjoy most of the time? NO YES • Screen for Depression if at least one of this 2 item is code yes Preliminary assessment • Exclude organic illness (Hypothyroidism, diabetes, cancer, neurological disease) • • • • Exclude Substance abuse disorder Medical and psychiatric history Physical and neurologic examination Mental status assessment Ask for suicidality!!! • C1 were dead? • C2 • C3 • C4 • C5 Think you would be better off dead or wish you NO YES 1 Want to harm yourself? NO YES 2 Think about suicide? NO YES 6 Have a suicide plan? NO YES 10 Attempt suicide? NO YES 10 1° steps • • • • Information Empathetic listening Reassurance psychological support (e.g. problem solving counselling) • referral to relevant social services and resources in the community. When to use antidepressants? • • • • • • • moderate to severe major depression functional impairment Long duration of illness/ Remittent course Severe somatic complains / concomitant chronic ilness Alcol or substance abuse Familiarity for mood disorders Psychotic sintoms Antidepressants Effective in around 60% of patients Explain! 3 weeks: improving/ 6-8 weeks full therapeutic effect. 1)Amitriptyline 50 mg NOCTE: gold standard Contraindications Not tollerate side effects 2) Fluoxetine 20 mg OD Amitriptyline Start with: 25 mg NOCTE 1/12 * 2 weeks If problem to review soon Monitoring acute treatment Psychological counseling *If Severe Depression start with 50 mg: -25 mg 1° week - 50 mg 2° week 4-6 weeks Evaluation of response to treatment Remarkable emprouvement Long term therapy at least 6-8 months Light emprouvement NO emprouvement + 25 mg every week (max: 200 mg) Change antidepressan Refer Psychiatrist Amitriptyline Contraindication: : Pregnancy and breast feeding, Glaucome, hyperthyroidism, prostatic hypertrophy, Stenosis pillorica, heart failure, serious rhythm disturbances, Hypotension, treatment with thyroid ormons, liver diseases, Dementia. Inform patients about side effects - Dosage in elders Fluoxetine Start with: 20 mg die 1/12 * *Better 10 mg 1° week 20 mg 2° week 2 weeks Monitoring acute treatment Psychological counseling Administer in morning or after lunch 4-6 weeks Evaluation of response to treatment Remarkable emprouvement Long term therapy at least 6-8 months Light emprouvement NO emprouvement + 10 mg every week (max: 40-60 mg) Change antidepressan Refer Psychiatrist Fluoxetine Contraindication: Pregnancy and breast feeding, Hypersensibility Bipolar Disorders • Bipolar I Disorder • Bipolar II Disorder • Cyclothymic Disorder Hypomanic Episode: Diagnostic Criteria A. B. • • • • • • A distinct period (at least 4 days) of abnormally and persistently elevated, expansive, or irritable mood. Different from usual non depressed mood. Mood disturbance plus three of the following symptoms (four if the mood is only irritable): Inflated self esteem or grandiosity Decreased need for sleep More talkative than usual or pressure to keep talking Flight of ideas, or racing thoughts Distractibility Increase in goal directed activity Excessive involvement in pleasurable activities C. Unequivocal change in functioning that is uncharacteristic of the person when is not sintomatic D. Disturbance in mood and the change in functioning are observable by others E. Not organic Disease or substanec Manic episode: Diagnostic Criteria • All the criteria of a Hypomanic episode plus: • Marked impairment (psychotic sintoms, explosive behaviour, high social-occupational disfunction, hospitalisation) Bipolar Disorder Sex: + M Genetic power: 80% High familiarity Bipolar I • Alternation of full manic and depressive episodes • Average onset is 18 years • Tends to be chronic • High risk for suicide Bipolar II • Alternation of Major Depression with hypomania • Average onset is 22 years • Tends to be chronic • 10% progess to full biploar I disorder Our data Major Depressive Episode in Bipolar 2 Mood Stabilizers + 200 mg every week Controindication: serious liver, kidney, heart disease, history of aplasia, pregna Monitoring after 2 and 6 weeks If effetictive: long term therapy: at least 2 years Not effective: + dosage or add an antidepressant hepatic enzyme induction. Carbamazepine Start with: 200 mg NOCTE 1/12 * 2 weeks If problem to review soon Monitoring acute treatment Psychological counseling *If Severe Depression start with 400 mg: -200 mg 1° week - 400 mg 2° week 4-6 weeks Evaluation of response to treatment Remarkable emprouvement Long term therapy at least 2 years Light emprouvement NO emprouvement + 200 mg every week (max: 800 mg) - Add an antidepressan - Refer Psychiatrist if no emprouvement Before and during carbamazepine therapy, monitoring: • full blood count • liver and renal function tests • pregnancy test. If not feasible • Regularly medical examination, • recent medical history that may help recognize symptoms suggesting the development of blood or renal or hepatic abnormalities. Questions to do • Have you ever had a period of time when you were feeling 'up' or 'high' or ‘hyper’ or so full of energy or full of yourself that you got into trouble, or that other people thought you were not your usual self? Have you ever been persistently irritable, for several days, so that you had arguments or verbal or physical fights, or shouted at people outside your family? Have you or others noticed that you have been more irritable or over reacted, compared to other people, even in situations that you felt were justified? (Do not consider times when you were intoxicated on drugs or alcohol.) Hypomanic Episode (Bipolar 2 ) • ACUTE TREATMENT: Haloperidol 5-10 mg nocte PO + Carbamazepine 200 mg nocte (see 2a) Resolution of Hypomanic Episode • LONG TERM TREATMENT: Continue only with Carbamazepine (see 2a) Manic Episode (Bipolar 1 ) • ACUTE TREATMENT: Haloperidol 10 mg IM or Chlorpromazine: 150-200 mg IM Untill patient can not be managed PO POST-ACUTE TREATMENT: Haloperidol 5-10 mg Nocte PO + Carbamazepine (see 2a) Resolution of Manic Episode • LONG TERM TREATMENT: Carbamazepine (see 2a); if not enough add Haloperidol 5-10 mg Nocte PO Bipolar 1 Manic Episode ACUTE: • Haloperidol 10 mg IM • Clorpromazine: 150-200 mg IM LONG TERM: • Haloperidol 5-10 mg PO nocte Asante sana for your attention Utopia lies at the horizon. When I draw nearer by two steps, it retreats two steps. If I proceed ten steps forward, it swiftly slips ten steps ahead. No matter how far I go, I can never reach it. What, then, is the purpose of utopia? It is to cause us to advance.” For any suggestion: jean.84@libero.i 0735525429 Eduardo Hughes Galeano