Systems Change: From a “Good Idea” to a Practice Culture
advertisement

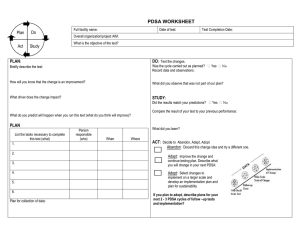
Systems Change: From a “Good Idea” to a Practice Culture Your name, institution, etc. here YOUR LOGO HERE (can paste to each slide) …dedicated to eliminating children’s exposure to tobacco and secondhand smoke Objectives • To understand the importance of creating a system to address parental tobacco use and SHS exposure of children • To understand how to implement changes in your clinical system using the Plan-Do-Study-Act Cycle Barriers to Change • The system is designed • For children with acute issues • To provide preventive care and acute illness management • To support a single service encounter • Lack of time • Reimbursement issues What Can We Do? • We have the tools and the knowledge • Evidence-based treatments exist • Unique opportunities to use treatments exist • How do we incorporate this into the day-to-day operations of our practices? • Implementation strategies exist Think of Your Practice as a “System” • Include all the parts that make the practice run • Staff, clinical and administrative • Records, paper and electronic • Rooms, hallways, waiting rooms • Resources in the community and beyond Analyze System Flow Patient checks in and goes to registration or waiting room Patient returns to waiting room after registration or to triage Registration Labs drawn Follow-up appointments scheduled LAB Check In Triage Waiting Room Check Out Exam Vitals signs Diagnoses and taken lab results entered in chart Rx Prescription written and/or filled Be Thoughtful In Your Implementation • Understand the current system • Research the areas most in need of change in your practice • Start with the end in mind…how do you want your system to function? Decision Support* is CRUCIAL • You need support from the top AND the bottom • Who’s in charge of Implementation? Supplies? Tracking outcomes? • New tasks shouldn’t be added to anyone’s (already too long) list – make time and space for them *AKA “buy in” Team Involvement Is CRITICAL • Involve your staff early! • First meet with key staff, then invite participation by staff at all levels • Be sure to include: • Front desk • Nursing and clinical staff • Administration Get Input • Brainstorm about implementation and barriers • Invite ideas on logistics of asking and advising • Develop implementation plans, using Plan-Do-Study-Act cycles The PDSA Cycle The PDSA Cycle: Plan, Do, Study, Act • Prepare a plan for implementing one small step. • Keep it very small!! • Be very specific • Include staff • Prepare materials • Set a time for the test (like today!) Plans Have Components • How will success be measured? • What are we doing? • Who will be the subject(s)? • How will we start? Finish? • Where will it be done? • When will it be done? The PDSA Cycle: Plan, Do, Study, Act • Do it! • Test it on ONE “sample” • One family, visit, nurse, or doc • Observe flow of program in the office • Note places for improvement The PDSA Cycle: Plan, Do, Study, Act • Study it! • How did it go? • How was clinic flow affected? • Were all materials available and easy to access? • What adjustments need to be made? The PDSA Cycle: Plan, Do, Study, Act • Do another cycle • Slightly improved or completely new • Several cycles are typical • Step back and take a look at the “big” picture The PDSA Cycle: Plan, Do, Study, Act (Part 2) • Implement in the entire practice. • Inform staff • Prepare materials • Make needed changes to the office system • Prepare a routine review cycle Monitor and Feedback • Are procedures working as intended? • Are staff completing assigned tasks? • Is documentation evident? • Are patient materials kept up to date? • Does the team receive timely feedback and support for a job well done? Model for Improvement What are we trying to accomplish? How will we know that a change is an improvement? What changes can we make that will result in an improvement? Your Aim The Measures The Cycle for Learning and Improvement Now What? • Mobilize your team! • Start with an Aim statement…what do you want to accomplish? • Then develop small but measurable activities • Create a PDSA (Plan, Do, Study, Act) cycle Need more information? The AAP Richmond Center www.aap.org/richmondcenter Audience-Specific Resources State-Specific Resources Cessation Information Funding Opportunities Reimbursement Information Tobacco Control E-mail List Pediatric Tobacco Control Guide