(1) Metabolic acidosis
advertisement
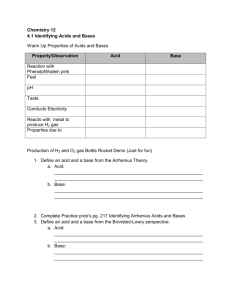
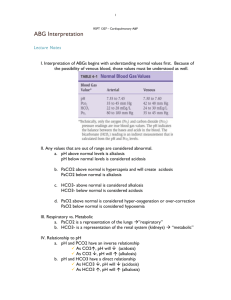
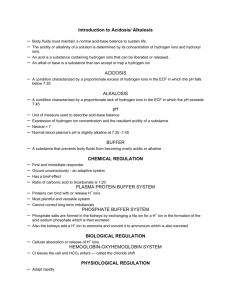
Section 2. Simple types of acid-base disturbance (1) Metabolic acidosis (2) Respiratory acidosis (3) Metabolic alkalosis (4) Respiratory alkalosis 1 (1) Metabolic acidosis 1) Concept It is defined as a primary decrease in plasma [HCO3¯], the pH tends to decrease. [HCO3 ¯] in serum pH = pKa + lg ---------------[H2CO3] The meaning of “primary” indicates the change happened firstly compared with ”secondary” change of another parameter. The metabolic acidosis is the most common type of acid-base imbalance. 2 In metabolic acidosis, the [HCO3¯] in plasma is decreased firstly, the pH tends to decrease. The [H2CO3] will decrease secondly. The pH may be in normal arange (compensatory acidosis). The pH may be less than 7.35 (decompensatory acidosis) 3 2) Classification Metabolic acidosis is classified into two types: (a)metabolic acidosis with normal AG ( with increased Cl ¯ ) and (b) metabolic acidosis with high AG (with normal Cl ¯). An increased AG means the accumulation of nonvolatile acids in the body. 4 3)Causes and Pathogenesis (a) The decreased [HCO3¯ ] (b) More acids buffered by [HCO3¯ ] (c) Hyperkalemia 5 (a) The decreased [HCO3¯ ] The decreased [HCO3¯ ] is caused by a) increased loss of HCO3¯ from kidneys, b) increased loss of HCO3¯ from intestinal tract, c) excessive production of Cl¯ d) dilution of HCO3¯ . 6 a) Increased loss of HCO3¯ from kidneys In proximal renal tubular acidosis (II type of tubular acidosis), the activity of CA is reduced. H+ -Na+ exchange is reduced. The reabsorption of HCO3¯ is reduced, which leads to a massive bicarbonate leak from kidney. 7 In distal renal tubular acidosis (I type), the capability of H+ excretion (H+-ATPase) is decreased. 8 b) Increased loss of HCO3¯ from intestinal tract The main extrarenal loss of HCO3¯ is from intestinal tract, like diarrhea and fistula in intestinal tract, because there is more HCO3 ¯ in intestinal juice than in serum. (gastric juice has more H+) (Effect of carbonic anhydrase in mucous membrance of stomach) 9 c) Excessive production of Cl¯ If excessive amount of substances (ammonium chloride and lysine hydrochloride ) have been administered, those substances can yield hydrochloric acid . For electrical neutrality, the [HCO3¯] is reduced after the [Cl¯] increased. 10 Replenish 0.9% NaCl to increase the [Clˉ] in plasma. [Na+] [Cl-] ( mmol/L) --------------------------------------------------------0.9%NaCl 154 154 Plasma 140 104 --------------------------------------------------------11 (b) More acids buffered by [HCO3¯ ] The accumulation of organic acids (nonvolatile acid) in blood due to more acids: a) decreased excretion of organic acids b) overproduction of organic acids. 12 a) Decreased excretion of organic acids Nonvolatile acids are filtered off through the glomerular membrane. In acute (less renal flow) and chronic renal failure (less permeability and area), the GFR is reduced, which results in the retention of nonvolatile acids in blood, so the AG is increased. 13 b) Incomplete catabolism of carbohydrates and fatty acids. Normally the complete catabolism of carbohydrates and fatty acids produces CO2 and water. The increased anaerobic glycolysis due to hypoxia(shock, severe anemia, pulmonary edema) results in lactic acidosis. Can increased production of lactic acid definitely cause metabolic acidosis? 14 In insulin lack, the catabolism of carbohydrates is reduced, the lipolysis ( catabolism of fat) is increased, the ketogenesis is accelerated. If the production of keto-bodies is more than the catabolism and excretion of keto-bodies, accumulation of keto-bodies will result in diabetic keto-acidosis. 15 Alcoholic keto-acidosis occurs as the result of accelerated lipolysis due to reduced insulin secretion. Starvation causes metabolic acidosis due to the accelerated lipolysis, which leads to the overproduction of keto- bodies (accelerated ketogenesis). 16 c) Administration of excessive fixed acids Salicylate水杨酸盐 (for stop pain and antiinflammation) can be converted to salicylic acid in the body. NH4Cl urea+HCl 甲醇(假酒) 代谢成甲醛,再代谢成甲酸在体内的积 累,甲醇在体内可抑制某些氧化酶系统,使糖的需氧分解 及机体代谢发生障碍,导致乳酸及其他有机酸在体内积聚, 引起代谢性酸中毒 d) 喝醋? 17 (c) Hyperkalemia 18 4) Compensation of metabolic acidosis (a) Compensation by buffering systems (b) Respiratory compensation (c) Renal compensation (d) Compensation by cells and bone 19 (a) Compensation by buffering systems Buffer pair (buffer system) consists of a weak acid and its’ salt, such as NaHCO3 ------------H2CO3 Na2HPO4 -------------NaH2PO4 Hb--------HHb H2SO4 + NaHCO3 = Na2SO4 + H2CO3 A strong acid becomes a weak acid after combining to NaHCO3 -. 20 The HCO3¯ will decrease and the production of H2CO3 will increase, H2CO3 can be resolved into CO2 and H2O. H2CO3 → CO2 +H2O The CO2 will be eliminated by respiration. [ H+]e will decrease, pH will increase. 21 Na2HPO4 -------------NaH2PO4 Hb-------HHb The other buffer alkaline (like HPO4 2¯/H2PO4 ¯) will be eliminated from kidneys. The [H+]e will reduce, the pH will increase. The HHb will keep H+ within RBC , the [H+]e will reduce, the pH will increase. 22 Low pH central chemoreceptors (b) Respiratory compensation Via stimulate the respiratory center increase the depth of respiration more carbon dioxide can be eliminated from lung normal pH Decreased pH will stimulate the chemoreceptors located in respiratory center (central) and in carotic body (peripheral), and enhance the ventilation. 23 Kussmaul respiration (deep sighing respiration) is for increasing CO2 excretion. More CO2 will be eliminated. The [H2CO3] will decrease secondarily to the decrease of [HCO3¯ ]. The ratio of [HCO3¯ ]/[H2CO3] will tend to normal. The pH will tend to normal. 24 Predicted compensatory formula ΔPaCO2(mmHg) Secondary compensation = 1.2 x ΔHCO3- ±2 primary change Or: PaCO2=1.5xHCO3-+8 ±2 PaCO2 can decline maximal to 10 mmHg. Value measured > value predicted: with respiratory acidosis Value measured < value predicted: with respiratory alkalosis 25 (c) Renal compensation Renal compensation begins from several hours after the addition of acid load, and it may take 3~5 days to reach the maximum of this compensatory capacity. The reabsorption of HCO3¯ is increased. Net acid excretion with urine is increased. 26 a) In metabolic acidosis, the activity of carbonic anhydrase (CA) increases, the H+ production is increased, the H+-Na+ exchange is increased, the reabsorption of HCO3¯ is increased in proximal tubule, 27 b) in distal tubule. In metabolic acidosis, the activity of carbonic anhydrase (CA) increases, the H+ excretion is increased, the reabsorption of HCO3¯ is increased. 28 c) In metabolic acidosis, the activity of glutaminase is increased, more glutamine will be decomposed into HCO3¯ and NH4+. More NH4+ is excreted into tubular lumen. Thus more HCO3¯ will be reabsorpted to the blood. 29 d) In metabolic acidosis, more H2PO4¯ is in the end urine, the end urine is more acidic in metabolic acidosis. Thus more HCO3¯ will be reabsorpted to the blood. 30 (d) Compensation by cells and bone When [H+] in ECF (serum) is increased in metabolic acidosis, the H+ will move into the cells, as a exchange for electrical neutrality, K+ will shift from ICF to the ECF. 31 In chronic metabolic acidosis, bone salt [Ca3(PO4)2] is also utilized as a buffer base, but the expense is decalcification of bone and osteoporosis (loose and soft bone). It is not a good way of regulating acidbase balance. 32 Changes of laboratory parameters Primary decrease of [HCO3 ]: AB,SB,BB ??? AB ?? SB BE ? Secondary compensation: PaCO2 ? pH ? 33 Changes of laboratory parameters Primary decrease of [HCO3-]: AB,SB,BB all reduced AB<SB BE increased negative value Secondary compensation: PaCO2 reduced pH decreased (tendency) 34 5)Effects on the body The main manifestations are: (A) effects on the cardiovascular system. (B) depression of mental activity (C) hyperventilation 35 (A) Effects on the cardiovascular system (a) Impairment of myocardial contraction (b) Arrhthmias (c) The hemodynamic effect 36 (a) Impairment of myocardial contraction Ca2+ combining with troponin肌钙蛋白 will start the myocardial contraction. ①H+ is a competitive inhibitor for Ca2+ combining with troponin. After H+ moves into the myocardial cells, the myocardial contraction is impaired. Severe acidosis may cause myocardial failure and low blood pressure because of the low cardiac output. 37 ② The protein expression of L-type of voltage-dependent calcium channel in myocardial cell membrane is reduced. Ca2+ inflow is reduced. ③ The protein expression of calcium channel in sarcoplasmic reticulum(SR) membrane is reduced.The release of Ca2+ from SR is reduced. 38 (b) Arrhthmias due to hyperkalemia Causes of hyperkalemia: H+-K+ exchange of cell Increased renal excretion of H+ Effect of hyperkalemia: Arrhthmias 39 (c) The hemodynamic effect: Low BP Catecholamine (dopamine, adrenalin, noradrenalin) can lead to the arteriole contraction,and increase the BP. The reaction of arteriole to catecholamine is decreased in acidosis, which leads to the blood dilatation ,decrease of peripheral resistance, Reduced venous return, Impairment of myocardial contraction Hypotension. 40 (B) Depression of mental activity (a) Manifestations: obtundation (thinking slowly), confused. (b) Mechanisms a) Increased [H+] causes cerebral vasodilatation. More blood supply will increase the CHP, then cause brain edema and high intracranial pressure. b) High [H+] increases the permeability of cerebral blood vessels. Decreased plasma COP and increased interstitial COP can lead to brain edema. c) Reduced ATPl production. 41 Glutamic acid Glutamate decarboxylase r-GABA, r- gama aminobutyric acid r-GABA transaminase Succinic acid琥珀酸 Kreb’s cycle d) The production of GABA (gama aminobutyric acid,γ-氨基丁酸, a inhibitory transmitter) is increased due to the activity of enzyme for the production is increased, and the activity of enzyme for the decomposition is decreased in low pH (acidosis). 42 (C) Hyperventilation for compensation. Kussmaul respiration (deep sighing respiration) is for increasing CO2 excretion. 43 (6) Principle of treatment For metabolic acidosis” 1) Treat the primary diseases which cause metabolic acidosis. 2) Replenish alkaline (HCO3¯ ) to the patients with normal respiratory function. Sodium lactate 乳酸钠?? (liver function) 44 3) Prevent the hypokalemia during treatment. (reason?) After the correction of acidosis, the [K+] will fall down rapidly by moving into the cells. The hypokalemia can cause lifethreatening cardiac arrhthmias. 45 4) In acidosis, [Ca2+] increases, [Ca2+] reduces during the correcting of acidosis. OHCa2+ ------→combining calcium Ca2+ ←------combining calcium H+ 46 Case Discussion 1. A 36-year-old man was hospitalized with a 3-day history of fever and watery diarrhea. His blood pressure was 90/60 mmHg, the pulse was 112/min, temperature is 38.0℃. The abdomen was distended and low skin elasticity. The laboratory results were: pH=7.21, PaCO2=28 mmHg, PaO2= 108 mmHg. [Na+]=135 mmol/L [K+] =3.0 mmol/L [HCO3-] = 16 mmol/L ΔPaCO2(mmHg) = 1.2 x ΔHCO3- ±2 Secondary compensation primary change =1.2X8=8~12 47 The patient’s problems were: (1)isotonic dehydration (2) decompensatory metabolic acidosis (3)hypokalemia. (after the correction of acidosis?) 48