Wade, William Douglas - Medical Council of New South Wales
advertisement

MEDICAL COUNCIL OF NSW LISR4RY PROFESSIONAL STANDARDS COMMITTEE INQUIRY CONSTITUTED PURSUANT TO PART 8 of THE HEALTH PRACTITIONER REGULATION NATIONAL LAW (NSW) No 86a To HOLD AN INQUIRY INTO A COMPLAINT IN RELATION TO Dr William Douglas Wade Date of Inquiry: S May 2012 Committee members: Mr Robert Kelly, Chairperson Ms Maria Kelly Or John Murray Wright Dr Susan Messner Legal Officer assisting Ms Dornarina Azad Committee: Appearance for Health Care Ms Jaimee Dinihan, Legal Officer Complaints Commission: Appearances for Dr William Mr Warwick Hunt of Counsel instructed by Ms Francesca Douglas Wade: Davis, Senior Solicitor (Avant Law Pty Ltd) Date of decision: 19 September 2012 Publication of decision: Refer to page 60 of this Decision for details of nonpublication directions. SUMMARY The Committee found all of the Particulars, with the exception of Particular 1.4.4 proven to the requisite standard and determined that Or Wades conduct amounted to unsatisfactory professional conduct within the meaning of section 1390 (1) (a) of the Health Practitioner Regulation National Law (NSL4)(the National Law (NSLI9). The Committee exercised its power pursuant to section 146B (1) (a) to reprimand Dr Wade. COMPLAINT A complaint dated 21 October 2011 against Dr William Douglas Wade MED0001067919 was referred by the NSW Health Care Complaints Commissioner to be dealt with by a Professional Standards Committee pursuant to the Health Practitioner Regulation National Law (NSW) (the National Law). 2. The Medical Council of New South Wales (the Council) constituted a Professional Standards Committee (the Committee) to inquire into the Complaint. At the commencement of the Inquiry on S May 2012 leave was granted to amend the Complaint. 1 The Amended Complaint was prosecuted before the Committee by the Health Care Complaints Commission’s Director of Proceedings acting as nominal complainant. AMENDED COMPLAINT 3. The Amended Complaint alleges that Dr Wade: Has been guilty of unsatisfactory professional conduct within the meaning of section 1398 of the National Law in that: he has demonstrated that the knowledge, skill or judgment possessed, or care exercised, by him in the practice of medicine is significantly below the standard reasonably expected of a practitioner of an equivalent level of training or experience; 2 and/or ii) he has engaged in improper or unethical conduct relating to the practice of medicine . 3 PARTICULARS OF THE AMENDED COMPLAINT & The Particulars of the Amended Complaint are as follows: At all relevant times, the practitioner conducted practice as a psychiatrist in NSW The practitioner was Patient A’s treating psychiatrist between about 1999 and 2001 originally on a fortnightly basis decreasing to monthly consultations. Patient A was referred to the practitioner in relation to a worn related mailer. The practitioner treated and managed Patient A in that period for various complaints including: chronic post traumatic stress relating to a history of childhood sexual abuse; mood instability; The amendment was not opposed by the Respondent. The amendments comprised the addition of the words at or’ as underlined in Particular 14. 2 Paragraph i) reflects section 1396 (1) (a) of the National Law. Paragraph ii) reflects section 139 B (I) (I) of the National Law. chronic major depression; and borderline personality disorder. The practitioner Provided Patient .4 with care which included counselling and prescription of medication. In August 2002 the practitioner recommenced treating Patient A intermittently until 2003 mostly in relation to prescription and management of psychiatric medication. In 2005 the practitioner consulted with Patient A on one occasion for the purpose of preparing a report for a motor vehicle accident claim. In May 2006, the practitioner consulted with Patient A in relation to a Workcover claim and anxiety. It is alleged that the practitioner. 1. Failed to observe proper professional boundaries in that: 1.1 In 2007 the practitioner: 1.1.1 exchanged messages of a personal nature with Patient A on the RSVP website; 1.1.2 after contact with Patient A on the RSVP website, spoke with Patient A by telephone and/or exchanged emalls with Patient A and discussed personal matters. 1.2 Between about I and 12 October 2008 the practitioner made telephone calls and sent text messages to Patient A in which the practitioner. 1.2.1 suggested that the practitioner and Patient A have a personal and/or sexual relationship; 1.2.2 suggested that the practitioner and Patient A meet for coffee or have dinner together. 1.3 On or about 12 October 2008 the practitioner met Patient A for dinner; 1.4 On or about 12 October 2008, at or after having dinner with Patient A, the practitioner: 1.4.1 kissed and/or hugged Patient A; 1.4.2 touched Patient A on the inner thigh; 1.4.3 commented on Patient A’s physical appearance including, in particular, her breasts; 1.4.4 suggested that the practitioner and Patient A have a personal and/or sexual relationship. THE MEANING OF UNSATISFACTORY PROFESSIONAL CONDUCT 5. Section 139B of the National Law provides, in part: "Meaning of ’unsatisfactory professional conduct" of registered health practitioner generally [NSWJ 1) Unsatisfactory professiinial conduct of a registered health practitioner includes each of the following(a) Conduct significantly below reasonable standard Conduct that demonstrates the knowledge, skill or judgment possessed, or care exercised, by the practitioner in the practice of the practitioner’s profession is significantly below the standard reasonably expected of a practitioner of an equivalent level of training or experience. (I) Other improper or unethical conduct Any other improper or unethical conduct relating to the practice or purported practice of the practitioner’s profession." 6. The phrase "significantly below" is not defined in the National Law. However, some guidance as to the meaning of the phrase may be found in the Second Reading speech introducing various amendments to the Medical Practice Act 1992 (the Act)4 - the relevant antecedent legislation to the National Law. These amendments included a similar definition of unsatisfactory conduct to that which is now contained in the National Law. "The first main purpose of the bill is to refocus the Health Care Complaints Commission (I-ICCC) on investigating serious complaints about health service providers. To achieve this, Commissioner Walker recommended that unsatisfactory professional conduct be redefined so that only significant instances involving lack of skill, judgment, or care will result in an investigation or disciplinary action --- the reference to ’significant’ in that context may refer to a single act or omission that demonstrates a practitioner’s lack of skill, judgment or care, or it may refer to a pattern of conduct In any individual case, that will depend on the seriousness of the circumstances of the case." The meaning of "significantly below" in context of the Act was considered by the Medical Tribunal of NSW in Re A Medical Practitioner and the Medical Practice Act (40010 of 2007). The Tribunal observed at paragraph 12: ’As a general principle, the use of the term ’significant’ may in law be taken to mean not trivial, of importance, or substantial." ONUS AND STANDARD OF PROOF 8. The HCCC bears the onus of establishing that Dr Wade has been guilty of unsatisfactory professional conduct. 9. For the Complaint to be proved, the Committee must be reasonably satisfied on the balance of probabilities that Dr Wade’s conduct satisfies the statutory definition of unsatisfactory professional conduct. As stated by the Dixon J (as he then was) in Briginshaw V Bflginshaw (1938)60 CLR 336 at 361-362: 25 October 2004 "Reasonable satisfaction is not a state of mind that is attained or established independently of the nature and consequence of the fact or facts to be proved The seriousness of an allegation made, the inherent unlikelihood of an occurrence of a given description, or the gravity of the consequences flowing from a particular finding are considerations which must affect the answer to the question whether the Issue has been proved to the reasonable satisfaction of the tribunal. In such matters reasonable satisfaction’ should not be produced by inexact proofs, indefinite testimony, or indirect inferences". 5 EXHIBITS 10. The Committee was provided with a number of documents prior to the hearing. The Complainant provided one folder of documents tabbed 1 t 15 (Exhibit A). The Respondent, Dr Wade provided one folder of documents Further documents were tendered at the tabbed 1 to 5 (Exhibit 1). commencement of the Inquiry. There were no objections to any of the documents. INTERIM NON-PUBLICATION DIRECTION 11. At the commencement of the Inquiry on 8 May 2012, the Chairperson issued an interim non-publication direction pursuant to Clause 7 of Schedule SD of National Law (NSW) in relation to the following matters: the name and address of the original complainant/patient; 2. any evidence relating to the subject matter of the Complaint which may identify the original complainant/patient. ISSUES 12. The issues to be determined by this Committee are: a) Whether the Committee is reasonably satisfied that the Particulars of the complaint are proven. b) In the light of any proven Particulars the Committee must then decide whether the Complaint against Dr Wade is proven. 6 c) If the Committee determines that the subject-mailer of the Complaint is proven, the Committee must decide whether it is appropriate to exercise any of the disciplinary powers conferred on it pursuant to Part S Division 3 Subdivision 3 of the National Law. The Balance of Probabilities was considered in by the NSW Court of Criminal Appeal in Gianoutsos v Glykis [2006] NSWCCA 137 at [47) - 151] What is required is that when loading the scales appropriate weight is given to the mailers to which Dixon J referred’ per McClellan CJ at CL (Sully J and Hislop J agreeing); See also In Re Dr Suman Sood [2006] NSWMT 1 at [10] The Committee can look at all the conduct found proven either separately or cumulatively when making a determination as to whether the conduct amounts to unsatisfactory professional conduct (Duncan v Medical Disciplinary Committee [1986) 1 NZLR 513 at 545, 546 and 547). BACKGROUND Dr Wade - Professional Training and Experience 13. Dr Wade graduated MBBS from the University of New South Wales in 1982. He gained his Fellowship of the Royal Australian College of Psychiatrists in 1989. 14. Following graduation Dr Wade undertook intern training at Sydney Hospital. He worked as a RMO at Hornsby Hospital in 1983. From 1984 -1988 he worked as a Registrar in Psychiatry at Macquarie Hospital. This period included terms in consultation liaison psychiatry and developmental psychiatry at Royal North Shore Hospital and significant time as a Registrar at the Arndell Children’s Unit at Macquarie Hospital. In 1989 he moved to the Mid North Coast to establish a private practice. According to Dr Wade "[TJhe private practice became increasingly dominated by patients suffering from PTSQ. such that I attended many conferences and joined the Australian and International Trauma Study Groups’ . 7 In 2001 Dr Wade moved to Lake Macquarie and commenced practice at Belmont. In 2010 Dr Wade relocated his practice to Toronto. 15. Dr Wade has remained in private practice since 1989. Dr Wade describes himself as practising general adult psychiatry with special interest in chronic Post Traumatic Stress Disorder, as well as Obsessive Compulsive Disorder, as well as treating other general adult psychiatric disorders - Bipolar Disorder, Schizophrenia, Major Depression and other anxiety disorders.’ Registration Status 16. Dr Wade was first registered in NSW on 3 March 1982. He is currently registered as a Medical Practitioner on the National Register of Practitioners in the General and Specialist categories. 9 Background to the Amended Complaint 10 17. Patient A first consulted Dr Wade in 1999.14 At that time Patient A was aged 44 The referral from Patient As general practitioner noted that she had ’suffered a psychological injury at work in June 1995" and included the following request: "Could you please see her for 12 ongoing psychiatric management". 18. Dr Wade treated Patient A for Post Traumatic Stress Disorder (PTSD) and related issues. During the course this treatment Patient A disclosed to Dr Wade that she had been sexually abused as a child. Initially Dr Wade saw Dr Wade’s curriculum vitae Exhibit 1 tab 2. ibid. Australian Health Practitioner Regulation Agency: Confirmation of Registration Status. 30 April 2012, Exhibit A tab 2. ’0 Where relevant the background reflects the Committee’s determination of the Facts having regard to the documentary and oral evidence adduced for the purposes of the Inquiry. In her statement dated 9 February 2011 Patient A states that the first consultation occurred in 1996. Dr Wade’s written statement and oral evidence supported by his medical records indicate that the first consultation occurred in 1999. 12 Exhibit A tab 4 at page 81. Patient A about monthly then less frequently until 2001 when she moved to He saw Patient A intermittently during 2002 and in early 2003. 19. Dr Wade saw Patient A once in 2005 for the purpose of preparing a report for a motor vehicle accident that occurred in 2002. 20. Dr Wade’s wife died in February 2006 from an illness that was first diagnosed in early 2005. As a result of Dr Wade using the internet service RSVP during 2007 communications took place between Dr Wade and Patient A. 13 Dr Wade next saw Patient A on 15 May 2008 in relation to a workers compensation claim. 21. The Amended Complaint sets out various Particulars and allegations concerning Dr Wade’s conduct at that consultation, his communications with Patient A and his subsequent attendance at a dinner with Patient A on 12 October 2008. The relevant facts are dealt with in the context of the Committees findings in relation to the Particulars. EVIDENCE 22. The Committee heard evidence from Dr Peter KIug the HCCCs Expert Peer, Patient A, Dr Bruce Chenoweth 14 and Dr Wade. Dr Peter KIug - HCCC Expert Peer 23. Dr Kiug graduated MBBS from the University of Queensland. He is a Fellow of the Royal Australian and New Zealand College of Psychiatrists (RANZCP). He has a number of current professional involvements including: Consultant and Forensic Psychiatrist at the Kiug Medical Practice; VMO and Consultant at the Mood Disorders Unit at Northside Clinic, Greenwich; Member, Forensic and Civil of the Mental Health Review Tribunal (NSW); Accredited Supervisor of Trainees in Psychiatry, Northern Sydney Area at RANZCP; Accredited Medical Specialist at the Workers Compensation Commission (NSW); Medical Assessor at the Motor Accident Authority, Medical Assessment Service; Assessor of Permanent Impairment at the Motor Accident Authority (NSW); Federal RANZCP Representative at Medicines Australia; Foundation member, Faculty of Forensic Psychiatry, RANZCP; Lecturer, ECT Training Program, Northside Clinic Greenwich; Consultant to BarCare. In summary Dr lug has "extensive experience in many areas of psychiatry - acute, chronic, Dr KIugs community-based, administrative, psycho geriatric and forensic." current main interests are "forensic psych/any and the treatment of severe 15 mood and traumaticrelated psychiatric illnesses." 24. Dr Kiug was retained by the HCCC to provide an independent review of documentation provided to him by the HCCC "and comment on the appropriateness of Dr Wade’s relationship both personal and professional with The circumstances and nature of this contact are dealt within the context of the Particulars, Dr Chenoweth had provided a written reference in support of Dr Wade for the purposes of the Inquiry. Further details of Dr KIugs professional experience are set out in his curriculum vitae at Exhibit A tab 6. 14 [Patient A]". 16 Dr KIug was specifically requested to advise whether he considered Dr Wade’s conduct fell below the standard described in section 1396 (1) (a) of the National Law. 25. In a report to the HCCC dated 14 April 2011 Dr Kiug summarised the documentation and opined as follows: "OPINION The relationship Dr Wade developed with [Patient A], in my view, was inappropriate. The details of the personal contact between [Patient A] and Dr Wade, in the various documents are generally compatible. It is clear she first consulted Dr Wade many years ago, however. She notes that it was in 1996 and he notes that it was in 1999. He therefore had treated her for about four to five years at that time I regard it as irrelevant as to whether Dr Wade knew he had established contact with a former patient on the internet dating service, ’RSVP’. The main issue is his response to [Patient A] once he had identified her as a former patient. Dr Wade states that he had continued to treat [Patient A] on a semiregular basis until 2003, had little contact with her thereafter, seeing heron one occasion in June 2005 and again in May 2008The type of correspondence between them, mainly via the internet and then by text (mobile phone) was inappropriate. Dr Wade actually notes himself that it was ’highly inappropriate. There was one episode of physical contact between them, probably in October 2008. They met and discussed the likelihood of having a relationship, which I understand was at his instigation. He states that the physical contact between the two of them was in a public place and constituted ’a cuddle or a hug and maybe a kiss on the cheek’. He said he can recall commenting on her breasts, but there is no indication that he recalls touching her in other ways. I note that there is some difference in the description of the nature of this contact in [Patient As] statements. It is of note, however, that Dr Wade, in his file documentation concerning [Patient A], regards her as having suffered from the following: * elements of post traumatic stress disorder * mood instability indicating a possible bipolar disorder type 2 * bordefline personality disorder. In a social security application (in a treating doctor’s report to Centrelink) he notes that she suffers from: ’ The documentation included Patient As initial written complaint, statement and statutory declaration and Dr Wade’s responses to the HCCC dated 21 October 2010 and February 2011. See HCCC’s letter (undated) Exhibit A tab 5 chronic PTSD chronic major depression somatic disorder (sic). He was aware that she was a victim of childhood sexual abuseDr Wade, in his final response of 1 February 2011 expresses remorse and contrition about his behaviour. He acknowledges that he contemplated a relationship with her stating that he could not explains [sic] his lapse of judgement’. It is of relevance, however, that Dr Wade had been exposed to significant stressful life events as follows: the death of his wife following acute myeloid leukaemia in February 2006, diagnosed in late October 2005 death of his mother at some time in early 2006 disrupted extended family relationships subsequent to his mother’s death, which he described as acrimonious and leading to breakdowns in his relationships with his brother and his father who cut him out of his life. Although the death of wife and his mother within a short time of each other in early 2006 cannot be disregarded as significant stresses, they were nevertheless approximately 2% years prior to his inappropriate contact with [Patient A] in the second half of 2008 when the situation escalated. He notes that he began using the RSVP website in 2007, however I therefore regard his contact with [Patient A] as inappropriate, despite the fact that he had not been her treating doctor for years. It is inappropriate because of the nature of the therapeutic contact with [Patient A] from 1999 (I assume his file notes are correct with respect to the commencement of treatment) to 2003. It is particularly inappropriate given that he diagnosed her with severe psychiatric illnesses, a personality disorder and knew that she was a victim of childhood sexual abuse. In response to your specific enquiries: (a) his behaviour fell below the standard expected of a practitioner of an equal level of training or experience and which was so at the time of his conduct (b) it is my view that his standard of behaviour was significantly below what is reasonably expected of a practitioner with the same training or experience as Dr Wade at the time of the events of the subject complaint (c) his departure from the standard does not incur my strong criticism." Or Kiug’s Oral Evidence 26. Or KIug gave oral evidence to the following effect. 27. In responding to questions in examination-in-chief Dr KIug confirmed that being a treating doctor" or being in a "doctor/patient relationship" were the "essentially same thing’ If a patient was formally transferred to another practitioner he would regard the treating relationship as having ended, however, if a patient subsequently saw a practitioner on an ad hoc basis he considered that the treating relationship has not been ended. 28. Or KIug opined that the professional relationship between Or Wade and Patient A had been maintained given the intense nature of Patient A’s contact with Or Wade and the nature of her problems. As Or Wade had seen Patient A in May 2008 he considered that the doctor/patient relationship "still pertained" at the time of the dinner in October 2008. 29. When asked whether this opinion would change if the consultation in May 2008 was only for the purposes of a workers compensation claim Or KIug responded that his opinion would not change substantially because of the intense nature of the treating relationship. He further noted that Patient A had been referred to Or Wade by her general practitioner and not by a legal institution and this indicated a treating relationship. 30. Or Kiug was asked to opine on Or Wade’s conduct assuming that the doctor/patient relationship no longer existed at the time of Or Wades contact with Patient A via the RSVP website but Or Wade had initiated the dinner, discussed a relationship with Patient A and hugged although not touched or kissed Patient A. He responded that he did not find this question easy to answer but considered that Or Wade’s conduct was not appropriate and still fell significantly below the expected standard because Dr Wade initiated the contact which was of a personal nature 31. Or KIug was asked how the "significant stressful life events" referred to in his report may have been relevant to Or Wade’s circumstances. Or KIug explained that these events raised the issue of whether Or Wade was suffering from some form of psychiatric problem such as a major depressive episode or an intense or prolonged grief reaction in the context of significant stressors. If so, he considered that this may have been likely to influence his judgment and could have been a mitigating factor. However, Or KIug acknowledged that he was not in a position to comment on whether Or Wade was in fact affected by these events. Or KIug noted that a person does not He need a formal psychiatric diagnosis to have impaired judgment. considered that Or Wade had still fallen below the requisite standard but there would be mitigating factors to be taken into consideration. In addition there would be a need to look at how predatory a person was and at a person’s motivation. 32. In cross-examination Or KIug agreed that whilst it seems likely there were mitigating factors contributing to the events in 2007 - 2008, there was no evidence that was the case. Or KIug also agreed that there would be less need for protective orders in circumstances where the stressors were unique 10 to a specific period of time (2007 - 2008), had subsequently ameliorated and there had been no other reported misbehaviour. 33. Dr KIug acknowledged that the statement in his report 1 therefore regard his contact with [Patient A] as inappropriate, despite the fact that he had not been her treating doctor for years" was poorly phrased. He explained what he had meant to say was that Dr Wade had not seen Patient A for years as a treating doctor but in 2008 the doctor/patient relationship still pertained. 34. Dr KIug considered that the major issue is the ’inequality of the relationship established in a doctor/patient relationship which is why abuse of the relationship is unacceptable because one party is dominant and the other is not... That unequal relationship will always be there and it is not extinguished by frequency... 35. Dr KIug acknowledged that the reference in his report to Dr Wade having been Patient A’s treating doctor for 15 years was based on Patient A’s statement. He accepted that the reference was incorrect given that Dr Wade’s medical records relating to Patient A indicate that he saw her for the first time in 1999. 36. Dr KIug was asked whether he was not strongly critical of Dr Wade’s conduct because it was social contact and a sexual relationship was not pursued. He responded "n pad" but his main reason for not being critical was of the "motivational aspect" and the emotional issues related to bereavement which he considered would have had an impact on Dr Wade. 37. Dr KIug considered that involvement with a supportive peer review group would be relevant to the protective aspect of the Committee’s jurisdiction. 38. In responding to questions from the Committee Dr KIug explained that he was not strongly critical of Dr Wades departure from the expected standards because from his reading of the documents provided to him by the l-ICCC there did not appear to be a strong predatory aspect to Dr Wade’s behaviour. In his opinion Dr Wade’s statement and correspondence with the HCCC was "not disingenuous". He considered that even though the conduct had taken place "a couple of years later" Dr Wade had been subjected to multiple stressors and there may have been a connection between his behaviour and the nature and severity of these stressors. 39. Dr KIug acknowledged that if a person had suffered a significant depressive episode further stressful circumstances in the future may impact on their judgment. Dr Kiug agreed that any possible future reoccurrence would not be resolved merely by the passage of time although he noted that hypothetically if a person has insight and seeks assistance their judgment could improve. 40. Dr KIug was asked to clarify the "motivational issues" which informed his reasoning for not being strongly critical of Dr Wade’s conduct. Dr KIug explained that he did not know the details of Dr Wades mental state, however, in terms of motivational issues "one needs to have some appreciation of how predatory a person is" and how much they are preying on a vulnerable person. He noted that with severe cases this would involve dominating another person. He said that it seemed to him that Dr Wade was endeavouring to reconstruct his life by re-establishing relationships and he saw Patient A as a 11 sympathetic ca?; his "impression’ was that Dr Wade had introduced personal issues and this "allowed him to abandon his role as a doctor’i If true, he considered this to be "a far cry from a person who is predatory’. 41. Dr Kiug agreed that the significance of the treating relationship between 1999 - 2003, especially given the intensity and nature of Patient A problems outlined in the documents, was such that the proscription of any other relationship between Patient A and Dr Wade would not be extinguished. 42. Dr KIug agreed that with his knowledge and background Dr Wade should have been aware that his conduct was inappropriate. 43. In re-examination Dr Kiug agreed that the best person to comment on Dr Wade’s state of mind would be his psychologist. 44. In response to further questions from Dr Wade’s counsel Dr KIug agreed that engagement with a peer group review process would reduce the risk of reoccurrence and that discussion of possible future stressors, insight, selfexamination and effective participation in discussion of these matters with such a group would reduce the risks of inappropriate conduct in the future. Patient A 45. Patient A’s evidence primarily comprised her written statement dated 9 February 2011 and her oral evidence in examination-in-chief." Although clearly anxious and at times tearful when giving her oral evidence Patient A presented as being thoughtful and honest in her endeavours to respond to the questions put to her. 46. Patient A’s written statement included the following, in part: "3. (first consulted Dr William Wade in approximately 1996. ... I attended him for psycho therapy [sicj treatment for post traumatic stress disorder I had recently moved to from Sydney and it was recommended I seek the treatment of male therapist. / had suffered post traumatic stress following a workplace incident where I was threatened. 4. During this therapeutic relationship / revealed to Dr Wade issues I had suffered as a child, that I had been sexually abused. I revealed this information quite early on as / had already disclosed this information to a therapist in the past 5. 1 saw Dr Wade quite regularly during this period and consulted him over a few years. (can’t remember when this began to taper off. 6. In April 2002 / was hit by a car and as a In 20011 moved to result / was diagnosed as suffering from serotonin syndrome. It was around this time / was had a discussion with my GP ... and I believe he mentioned to me Dr Wade was now practicing in Belmont. " Exhibit A also included Patient A’s letter of complaint dated 27 August 2010 and an undated Statutory Declaration. 12 7. / was referred back to Dr Wade and / saw him again at his practice at Belmont. I was consulting with him Throughout 2002, / cannot recall how regularly or for over what period of time this occurred. / recall his wife was his receptionist up until the last few appointments. After a while I stopped seeing him as / was getting over the therapy process. 8. It had been some years since / saw Dr Wade therapeutically when / was on RSVP and received a kiss’ from someone who had their photo locked / sent a message to him and received the photo of him and immediately recognised him as Dr Wade. 9. I can? remember WI initiated The email but I recall I informed him I knew him. His reply back to me was that he didn’t recognise me from my photo. We corresponded over emails for a shod while. These emails were nothing sexual and I think I recall him telling me his wife had died. 10. He called me and we began speaking over the phone. It felt a bit strange talking to him or entertaining the thought of a relationship with him because he knew so much about me. We never actually met for a date, but I felt there was an intention them to pursue me as he was on RSVP which is a dating site. I can? recall the exact context of our conversations. 11. 1 felt sony for him as his wife had died and I offered to set him up with some of my friends. He declined this offer. After a short while this relationship just stopped, without any real reason or issue. 12 In 2007 / suffered a mental breakdown and was hospitalised. At this time there had been some years since / had last consulted him and around about 6 months since meeting him on RSVP. / was admitted into the James Fletcher hospital for about two weeks. 13. 1 cant recall if it was that year or a little while later, but I was having difficulty with The combination of medications I was taking. I recall / sort [sic] Dr Wade to seek medication from him. He didn’t prescribe me anything, I think he was just so off the track [sic] my therapy. 14. I recall he initiated a conversation with me about howl felt about meeting each other on RSVP. I was shocked about this and was not happy that he spent almost the entire time talking about RSVP. I did tell him I was flattered but this was an attempt to distance myself from him. 15. 1 recall leaving this consultation and contacting my then boyfriend quite upset and confused telling him my Doctor had just hit on me. 16. Sometime after this / began receiving phone calls from Dr Wade. I recall during one of those conversations he informed me he was moving in with his girlfriend. He also said to me ’I have a proposition for you, will you be my mistress? , 17 I discussed these phone calls with my sister and we were both concerned That Dr Wade was not ready to move on so soon after his wife’s awful death. 13 18. Around this time I met him for dinner at his request. / thought! will meet him and see what he has to say and tell him what I think. / expected to see this grieving man but over three hours he told me about his new gin’friend and their life together. 19. After dinner he walked me to my car and his kissed me on the lips good bye. He then ran one hand down the inside of my thigh and said, ’Nice tits. ’This made me feel uncomfortable. 20. / am really unsure of how things eventuated and in what sequence but my overall memory is that Dr Wade was making advances towards me for me to be his mistress. I recall at one point I said to him, "How long do you expect me to be your mistress?’ And he said ’Until you find someone.’ There was never a physical or intimate relationship between us but my belief is he just wanted sex from me. 21. / have today produced my old mobile phone where I have stored text messages I had received from Dr Wade. These were stored under the name Doug Wade. 22 This phone shows a message sent to me from Dr Wade on the 13 October 2008 at B. 58am which said, Hi ..., also enjoyed last night, much lust and desire, doubtful if you are cut out for the ambiguity of the role, main thing is for you to be selfish and decide what’s for you. Regards and Kisses Doug’ 24. This makes me think / had contacted him first to talk about the night before when we had gone on the dinner I have already mentioned. 26. The next message on my phone from Dr Wade was received on the same day at 3. 54pm. This message says, ’Hiya, sony but / am in no position to vouch for you for anything with any third party. Regards Doug’ 26. The next message on my phone from Dr Wade was received on the 15 October 2003 at 12. 55pm. This message read, ’Hi ..., thinking all a mistake taking you out of comfort zone, doubting own motivation. Sony but I think need to let go of fantasy of safe secret relationship. Regards Doug.’ 27. At no time did / enter or wish to enter a secret relationship with Dr Wade. / felt uncomfortable because he knew so much about me and my personal life. 28. Even though / had not had a therapeutic relationship with Dr Wade for a period of time / still considered him my treating psychiatrist He knew of all my past trauma. 29. I decided to make a complaint following my birthday last year when I woke up very distressed. A young friend of mine had committed 14 suicide and so I began to reflect on all the negative things that had happened to me. 1 reflected on the circumstances of his approaches to me. / began to become concerned that Dr Wade may had [sic] done this to other vulnerable woman [sic] and so I lodged this complaint" 47. Patient A gave oral evidence in evidence-inchief to the following effect. 48. Patient A confirmed that Dr Wade was not the first psychiatrist she had consulted. Patient A recalled that she had experienced her first "breakdown" at about aged 40 and as a consequence in the period between 1995 - 1997 she had consulted a female psychiatrist practising at Bondi Junction before moving back to the North Coast of New South Wales to be closer to her children. 49. Patient A was taken to various paragraphs in her written statement dated 9 February 2011. Patient A conceded the reference to first consulting Dr Wade in 1996 may not be accurate. She said that it was hard to remember that far and Sydney and back but she had attended group therapy in had consulted Dr Wade for 4 - 5 years from 1999-2003. She recalled that when she first consulted Dr Wade she saw him twice monthly and consultations were usually for 1 hour but sometimes 45 minutes. The frequency of consultations reduced over tire. She was unable to recall whether Dr Wade made notes during the consultations. 50. Patient A said that her first psychiatrist had suggested she should see a male therapist so that she could "learn to trust men again". Patient A explained that she had been sexually abused from the age of 3. In addition she had married her first boyfriend who was mentally and physically abusive. 51. Patient A was referred to paragraph 14 of her statement. Patient A was asked why she had told Dr Wade she was "flattered". She explained that she did not want to go to the consultation but had been having problems with her medications. At the consultation Dr Wade had talked about the coincidence of their meeting via RSVP but all she wanted was some medication from him. She had been taking Aropax which had reacted badly with the Tramal she was also taking. She said that she had serotonin poisoning, problems with digestion, pain in the liver area, had put on weight and wanted something different to Aropax. She said she had been taking Aropax for 10 years and did not want to take it anymore. Her general practitioner had suggested that she see Dr Wade. 52. Patient A confirmed that Dr Wade did not prescribe any medication at this consultation. She said that she "walked away empty handed" and all Dr Wade had done was to just ask her how she felt abdut him. She confirmed that she had not raised the issue of their contact via RSVP with Dr Wade. 53. Patient A said that she had suffered a psychotic breakdown" in 200718. She had been admitted to James Fletcher Hospital and required 10 days off work. She recalled that she had informed Dr Wade of this when she next saw him. Patient A recalled, in particular, that Dr Wade was critical of the resident In subsequent evidence Patient A said that this had occurred in about July 2007 at the time of the "Newcastle Floods". 15 psychiatrist at the James Fletcher Hospital because he had prescribed Aropax for her. Dr Wade had spoken about textbook medicine" and "textbook psychiatrists’ saying "no one in their right mind would prescribe this". Patient A again noted at that time she had been taking Aropax for 10 years. 54. Patient A was referred to paragraph 28 of her statement and asked to clarify why she considered that Dr Wade was stil her treating doctor. Patient A responded that it was the same as with other doctors who have been her treating doctors. She explained that she has an orthopaedic surgeon and rheumatologist who are both excellent and caring and she would go straight back to them if she necessary, commenting "they are still my doctors - it does not matter how many years have lapsed". Patient A noted that even if there had been a break in time she would never consider that Or Wade was not her treating psychiatrist. 55. Patient A confirmed that Dr Wade had never informed her that she did not need to see him anymore. She recalled that lie had told her that she was sick and had to see him. 56. Patient A confirmed that she did not go back to consult Dr Wade after the dinner in October 2008. She said that at the dinner she had expected to find a man in "terrible grief’ but she did not find that at all. 57. Patient A confirmed that it had been necessary for her to see another psychiatrist since her last consultation with Dr Wade. Patient A explained that she had 7ust had a breakdown" about 3-4 weeks prior to the Inquiry and was "still getting over it". This had occurred at Coffs Harbour and had involved four calls to the local Mental Health Crisis Team. Patient A said that she did not wish to be admitted to hospital; she had ceased taking her medications and had experienced suicidal thoughts. Patient A said that it had taken two months to get an appointment with a psychiatrist and she had seen up to nine general practitioners before finding a general practitioner who specialised in mental health. This general practitioner is also associated with the Black Dog Institute. In addition she had eventually secured an appointment with a for 11 May 2012- She had also seen a male psychiatrist in counsellor a few times but concluded they were "not suited" because she was not interested in the particular therapies that he was offering. 58. Patient A said that she was apprehensive about the forthcoming consultation with the psychiatrist on 11 May because he is a male and she had "to be able to trust him". 59. Other than her recent breakdown Patient A described her mental health as having been "pretty good for the last few yeait’ but said that she has "suffered stress’ Patient A attributed the cause of her recent breakdown to a "total family breakdown" which had caused a lot of stress together with the pressure related to the prospect of giving evidence in the present proceedings and whether she would be believed. 60. Patient A said that she has worked "on and off’ but has realised that she is better off not working with certain personalities and only working on her own or with a small team. 16 61. Patient A was asked whether she expressed any interest in a personal relationship at her last consultation with Dr Wade in May 2008. She replied She said that she was shocked "not at all I simply went to get medication." and embarrassed when Dr Wade had asked her how she felt about a relationship and did not know what to say other than that she was flattered. 62. Patient A was asked why she agreed to go to the dinner with Dr Wade. She described the situation when Dr Wade commenced telephoning her after the consultation as unreal" and ’really bizarre’ She said that when Dr Wade rang and had said that he had a proposition she thought this was odd because he was grieving and she thought that he was not ready to move in with his girlfriend. She had agreed to attend the dinner to "see what’s going on". Patient A described herself as having a lot of strengths but as also having compassion and being vulnerable. 63. Patient A was asked about her understanding of what Dr Wade wanted. She replied "for me to be his secret mistress". Patient A said that even if Dr Wade was not her treating psychiatrist she would not have entertained this type of relationship because ’it’s not worth if’. She referred to friends who had gone down "similar paths" which had resulted in "endless tears". 64. Patient A was asked whether she wanted any other type of relationship with Dr Wade, for example, a committed relationship. Patient responded "no". Patient A confirmed that no such relationship was offered to her by Dr Wade. 65. Patient A recalled that when Dr Wade walked to her car with her he had kissed her on the lips, albeit not passionately, hugged her, told her she had "nice tits" and run his hand up the side of her leg. She said that she had "frozen" said goodnight"j umped" into her car and went home. 66. Patient A said that she had sent Dr Wade a text the next day and thanked him for the dinner because she wanted finality". She said that she needed him to know that there would never be anything in the relationship and it was final and over and ’1 could see it for what it was". 67. Patient A recalled the conversation at dinner related to Dr Wades new relationship, his children, his recent trip overseas and his current work. She said that when "the mistress thing came up" she had squared her shoulders and looked him in the face" and said, "not in an encouraging way’ "how long do you intend this to go on for" and Dr Wade had replied "until you find someone". 68. In responding to questions from the Committee Patient A confirmed that her initial contact with Dr Wade via RSVP had been in the form of a couple brief emails". Patient A said that the profile provided by Dr Wade looked interesting but the photograph accompanying the profile was locked. She said that she had recognised that it was Dr Wade when the photograph was unlocked. She said she had thought ’that’s odd I wonder what has happened". She said that Dr Wade had told her that his wife had died and she had asked him when. Patient A said that she was looking for a permanent partner at that time. 69. Patient A said that she did not believe Dr Wade when he told her that he had not recognised her photograph on RSVP. She said that she had used the 17 same photographs on RSVP as she used on Facebook; the main photograph had been taken in 2006 and she did not think that she had changed dramatically. Patient A said that she had invited Or Wade to a barbeque at one of her girlfriends who was single but he had declined. She said that she "did not want to go on date with someone who knew about your mental health". 70. Patient A could not recall when Or Wade asked her out following their initial contact via RSVP She said that she had been shocked by the death of Or Wade’s wife and that he was asking her out on a date. She commented 1 would always be a patient - even on a date without sex I would always be a patient". 71. Patient A noted that Or Wade had given her his private phone number but she had not used it because she did not want to be classified as a "stalking kind of patient". 72. The Committee notes that at the conclusion of Patient A’s examination in chief and, in the absence of Patient A, counsel for Or Wade informed the Committee that pursuant to Or Wade’s instructions he did not intend to crossexamine Patient A because of Or Wades concerns for Patient A’s mental health. Counsel for Or Wade noted that there was a "factual divide" between some of the evidence given by Patient A and Or Wade’s evidence. Counsel for Or Wade indicated that Or Wade was not abandoning these factual disputes, however, he considered that there was "no profound discrepancy" that could not be dealt with other than by cross-examination. Counsel for Or Wade anticipated that where relevant these issues could be satisfactorily addressed in the Respondent’s written submissions. Or Bruce Chenoweth 73. Or Chenoweth had provided a written reference in support of Or Wade for the purposes of the Inquiry. 19 Or Chenoweth is currently a Senior Staff Developmental Psychiatrist with the Diagnostic and Assessment Service at St George Hospital. 74. Or Chenoweth’s reference reads in part "Icon firm that I am a registered Consultant Psychiatrist of some 37 years standing. Currently / am working in Intellectual Disability Mental Health in a major teaching hospital Previously, I had a busy private practice in Newcastle for 25 years, and in Brisbane prior to that My professional interests have been in adolescent mental health, psychotherapy, neurvpsychiatry, and family therapy. / have taught Registrars and published in my field I have also held administrative positions in public health and in private hospitals. / belong to a number of professional organisations and regularly present papers at national and international conferences. Exhibit 1 tab 4. The reference is undated but responds to a letter from Dr Wades solicitors Avant Law dated 22 March 2012, The Committee notes that Dr Peter Corrigan, a consultant psychiatrist, also provided a personal and professional reference dated 30 April 2012 in support of Dr Wade for the purposes of the Inquiry (Exhibit 1 tab4), ’9 18 I first met Dr Wade when he relocated to Newcastle from the midnorth coast approximately around 2001 He was invited to join our peer supervision group almost immediately on arrival and has remained a constant attendee at our fortnightly meetings ever since. This group is a forum to discuss all aspects of clinical practice, the difficult clinical issues, the ethical and personal aspects raised in the course of our work, and has a supportive function so necessary in a demanding and personally challenging vocation. In all ways, Dr Wade has been a wise and stable contributor to this group. His counsel has been measured, and cautious conservative and always insightful. He has been relied upon by other group members to a great extent for a compassionate and reliably ethical viewpoint My opinion, and one shared, I am sure by all his colleagues is that he is both professionally and personally a man of great ability and integrity highly respected by his patients and within his profession. Frequently, issues pertaining to moral and ethical behaviour would be raised by one of the group. Conflicts of interest and of boundary are frequent when one practices psychiatry in a relatively small city where there are relatively few Psychiatrists and where confidentiality can be von, difficult to preserve. Dr Wade always preserved strict adherence to tight professional boundaries and could be relied upon to counsel the group appropriately. It should be noted that the group recognised at the time the deep sorrow and despair experienced by Dr Wade over the prolonged terminal illness of his wife who finally died in the most distressing of circumstances. Their’s was a close and mutually supportive relationship and one in which Dr Wade depended heavily upon her for much of the running of his business and household Her loss left him quite lost’ for a period of time. He did not appear to have been clinically depressed then but perhaps, as a group we could have been more supportive at that time of vulnerability. In subsequent discussions regarding the complaints made, he has repeatedly expressed remorse and disbelief that his judgement could have been so compromised at that time. He, of all people has an understanding of the consequences of boundary violations" 75. Dr Chenoweth gave evidence by teleconference. His evidence was to the following effect. 76. In examination-in-chief Dr Chenoweth adopted the contents of his reference. He confirmed that Dr Wade attended peer supervision groups on a fortnightly basis. He described Dr Wade as being punctual and meticulous in attending these meetings, usually being the first person there. 19 77. Dr Chenoweth was asked to outline the circumstances relating to Mrs Wade’s terminal illness and Or Wade’s reactions. Or Chenoweth recalled that he had met Mrs Wade socially and visited their home early in their acquaintance. He had been informed that Mrs Wade had a blood condition which would require a bone marrow transplant. An apparently compatible donor had been found in Germany, however, the transplant had not been successful. Mrs Wade’s immune system had been compromised; she developed fungal infections of the gut with loss of much of the internal lining of the gut and associated internal haemorrhaging in addition to rashes and dermatological conditions. He said that he did not see Mrs Wade during this time but was receiving regular updates from Or Wade. 78. Dr Chenoweth described Mrs Wade as a "great organiser with a strong personality". He noted that Mrs Wade had managed the household, the practice, the household accounts and the billing for Or Wade’s practice and was the organiser behind Dr Wade’s life". He said that Dr Wade was lost" after Mrs Wade’s death; he had no computer skills; the new practice manager was "not great" and Or Wade had to maintain his practice and his life in general." 79. It was put to Or Chenoweth that Or Wade had made some "poor decisions" in October 2008 and Or Chenoweth was asked whether Or Wade had discussed these with the peer review group. Or Chenoweth responded that Or Wade had not discussed these matters as they were unfolding, however, although not aware of any details the peer review group was aware of Or Wades desperation. Or Chenoweth observed that in retrospect he wished the peer review group had been more supportive as Dr Wade was extremely isolated and there were elements in his life that he was not coping with. 80. Or Chenoweth was asked to expand on his reference to the level of remorse expressed by Dr Wade in relation to his conduct concerning Patient A. Or Chenoweth explained that much of the remorse expressed by Or Wade was expressed to him privately. This often occurred whilst they were waiting for other members of the peer review group to arrive. Or Chenoweth recalled that Dr Wade had described himself as bloody stupid" and said "how could / have done that". 81. Or Chenoweth said that Or Wade had always been the "standard bearer" of the peer review group for ethical issues in relation to boundaries and transference situations and had focused on clarifying potential difficulties for others in the group and acted as a mentor. 82. Dr Chenoweth described Or Wade’s remorse as "self-flagellating". Dr Chenoweth commented that he could not believe "that this person could have this lapse in his vigilance". He considered that Or Wade did not hide or endeavour to minimise his conduct. 83. Relying on his personal and professional knowledge Or Chenoweth was asked to opine on the probability of future lapses by Or Wade. Or Chenoweth responded "most unlikely - whilst never absolutely certain". He explained that the peer review group will continue. He said there is a level of trust in the group, the members know a lot about each other at a personal level; it is a very supportive group and not afraid to confront each other including out of 20 hours if required. Dr Chenoweth commented that he thought the group had let Dr Wade down on this occasion. 84. In cross-examination Dr Chenoweth confirmed that there was no leader in the group and all members were considered equal peers. He confirmed that there was not a lot of socialising" outside the group other than special occasions such as the occasional birthday. 85. Dr Chenoweth was asked to expand on his comments in relation to practising psychiatry in a small city. Dr Chenoweth explained that he had practised in Newcastle for 25 years and had seen thousands of patients and as a consequence it is difficult to walk down the street without running into patients or families of patients about whom he may be privy to information. He said that he is "super cautious" but even then he might find that he is treating someone connected to a patient which gave rise to difficulties. He noted that the situation was even more serious when treating the families of colleagues. 86. Dr Chenoweth noted that there were many types of boundary issues in addition to sexual boundaries which could arise in a small town. He said that boundary violations were often discussed at peer review group meetings. He confirmed that he was not aware of Patient As complaint until after the event. He described Dr Wade as the most dynamic and psychoanalytical member of the peer review group. He considered that Dr Wade would be aware of transference issues. Dr Wade - The Respondent 87. By way of preliminary mailers relating to Dr Wade’s examination in chief the Committee was taken to several documents in the Exhibits. These documents included the following: Dr Wade’s medical records in relation to Patient A; 2 The HCCC’s letter to Dr Wade dated 15 October 2010:21 Dr Wade’s response to the HCCC dated 21 October 201 ;22 Dr Wade confirmed that the factual material and opinions set out in the letter were true. Dr Wade’s counsel asked that the Committee members have regard to the contents of the letter in their deliberations. Dr Wade’s letter dated 1 Februar’ 2011 to the HCCC responding to a request for further information . 2 Dr Wade confirmed the factual material and opinions set out in the letter were true. 2010.24 Dr Wade Dr Wade’s Curriculum Vitae dated 21 October confirmed that the contents of the document were true. 20 Exhibit A tab 4. Exhibit A tab 7. 22 Exhibit A tab S. 23 Exhibit A tab 9 24 Exhibit A tab 10. 27 21 The New South Wales Medical Board’s Code of Professional Conduct" . 25 Dr Wade confirmed that he was aware of the Code at the time of the allegations set out in the Amended Complaint. 88. 89. The Medical Council of New South Wales’ Policy Document Sexual Misconduct’ (In force from 4 December 1991 to November 2011).’ 6 Dr Wade confirmed that he was aware of the Policy and had access to the Policy. Dr Wade also confirmed that he was aware of the revised Policy Document promulgated by the Australian Health Practitioner Regulation Agency. .17 his Dr Wade adopted the contents of his undated written statement 2 curriculum vitae ’ and his record of Continuing Professional Development (CPD). 29 Dr Wade also adopted various admissions set out in a letter dated 30 April 2012 from his solicitors Avant Law addressed to the Committee’s legal off icer. 3 Dr Wade’s written statement reads, in part: ’9. Since the time of this complaint there have been changes in my personal life, I have supportive colleagues and a supportive partner who is a clinical psychologist My work and personal life is stable. In 2006 - 2008 1 was under a great deal of personal stress caused by the illness and death of my wife, my domestic situation in general, and the death of my mother with its subsequent impact on me and on my family. I note that Dr Kiug considers that These stressors, having occurred more than two years prior to the inappropriate contact with [Patient A] in 2008, seem to be less significant because of the time that had elapsed since 2006. It is conect that time had passed however in many ways the loss and trauma was almost as acute, as was the sense of isolation, panic, disconnectedness, guilt. My wife’s illness. Acute Myeloid Leukemia was very difficult on many levels, and her death was traumatic and left long lasting scars which I realised were in some elements, symptomatic of PTSD, and would take a long time to resolve and work through. I have worked through most of these issues and have difficulty looking back to The period between 2005-2008 as much of it seems very remote, or distant or surreal. io. For example, after my wife’s death I realised I was not caring for my own physical health and found myself referred by my GP to the same haematologist for treatment, and would be sitting in the same rooms as I had sat with my wife during her treatment These kinds of things added to the surreal sense I had fora long time after her death. II. In relation to [Patent A’s] statement which was written after my second response to the HCCC, I would like to say The following. 25 Exhibit A lab 14 Exhibit A tab 15. 27 Exhibit 1 tab 1. The document was received by Avant Law in early April 2012 20 Exhibit 1 tab 2, 29 Exhibit 1 tab 3, This was expressed to be subject to the amendments made to the Amended Complaint with regard to paragraphs 1.4.3 and 1.4.4. 26 22 12. [Patient A] became my patient in 1999. I saw her in relation to a workers compensation claim. (treated her for PTSD and related issues and saw her about monthly, then less; until 2001, when she moved away / saw her Intermittently in 2002, until early 2003. After that 1 saw her in once in 2005 for The purpose of preparing a report for a motor vehicle accident That occurred in 2002. I did not see her again until 2008 when I saw her once, again in relation to a workers compensation matter. 13. After the death of my S te in February 2006, I used the Internet service known as RSVP sometime in 2007. The contact that was made wiTh IPatientA] was entirely accidental as I did not know it was her / sent a person a photo of me, that person was [Patient A] and she recognised me. I did not recognise her She thereafter contacted me by email in relation to my description of myself as a ’widower’. I then realised who she was. 14. There was no intention to pursue [Patient .4] as she states in paragraph 10 of her statement and the very minor amount of email correspondence or telephone contact that occurred at That time was simply to acknowledge that she had made contact with me and to inform her of The change in my professional and personal circumstances. My wife was the practice manager and receptionist and [Patient A] knew her slightly and she found it shocking that my wife, such a healthy and happy person, had died. [Patient A], now knowing that I was widowed, then offered to act as matchmaker, an offer which was declined. There was no ’relationship’ as she described i in paragraph 11. 15. Although this situation was a little awkward and was connected to my personal life I do not consider that my conduct in this regard could be considered a breach of any professional standard. 16. Subsequent to the accidental contact Through RSVP, [Patient A] made an appointment to see me, in May 2008 on a referral from Or... GP, for a work cover matter. It was months later and I had not had any contact with her in The meantime. Except for the report in 2005, I had not seen her as a patient foroverfrve years. 17. At the consultation in May 2008, [Patient A] did not give a recent history of a breakdown or hospitalisation since last seeing me. On the contrary she was adamant That she was well and was not in need of medication. She described her work situation which was the reason for the referral, ho we ver she said she was coping with it well. She said she did not need medication other Than The occasional Temazepam that she obtained from her General Practitioner. I did not prescribe anything, as there was no indication it was necessary. 18. My recollection of The consultation was that it was conducted in a methodical way, moving through a standard history taking, and a mental state examination. [Patient A] then brought up the subject of The RSVP coincidence She initiated The discussion at the end of what was a routine consultation. The discussion was in the context of how much she had moved on from her former role as a patient and how well she was. I spent some time explaining That it was accidental That I contacted her, and that it would not be appropriate to pursue a relationship. I did not attempt to ’hit on her’ as described in paragraph 14 and 15. 19. In October 2008 I did contact her. I do not have a clear recollection of Me timing or of the conversations but I did call her and I recollect she 23 was surprised to hear from me, given my comments in May about the inappropriateness of a relationship, transference and so on. I invited her to meet me and we met in a cafØ in Newcastle. 20. / have given This a great deal of thought and reflection and analysis. I have spoken to other colleagues who are clinical psychiatrists and my partner who is a clinical psychologist in order to put these Things into perspective and to understand why I behaved in an uncharacteristic and inappropriate manner My thinking at that time was sd/I very much affected by not just my i#e’s death but The months of emotional turmoil, anxiety, distress and drama of her illness before she died My sense of loss, and of fear of future loss was probably a motivational force. Taking [Patient A] up on her offer seemed a kind of insurance against more loss, but it was unrealistic an unfairon [Patient A]. 21. 1 recognised this but / did not handle The situation well. At the dinner I explained that after the trauma of losing my wife, I had met someone with whom / was compatible and with whom I was entering into a very serious relationship. This was actually causing me great anxiety and fear because I was committing to another person who / might lose- An affair with [Patient A] could be a kind of secret insurance policy against losing another wife, This is The context of The reference to a ’safe secret relationship’ in the text message. The discussion over dinner did revolve around my wife, her illness and my new relationship and / understand that! was overly open with [Patient A]. / recognise I took advantage of [Patient A’s] availability and apparent willingness to engage in a relationship with moon an adult basis. 22. After dinner we said goodbye. I do not recall kissing [Patient A], or touching her inappropriately. Any contact we had was appropriate for contact in public place and would have been slight 23. I should have realised That This characteristic of maturity and self reliance was in contradiction to what / knew about [Patient A] in the long term, as a patient, but I [sic] my ability to objectively self-observe and to observe others was affected by my personal circumstances and the length of time since I had seen her as a patient. / accepted her assurances That she was doing well. 24. 1 did not really intend to follow through with any relationship with [Patient A], and attempted to explain this The following day. 25. My explanation of the text messages is That the first message is self explanatory. After the dinner [Patient A] sent me a message and I replied. [Patient A] Then sent me a message asking me to do something in relation to some other matter. I recollect it was asking me to be a referee but / did not feel could do it, which is the reference to Third parties in The text 26. It did not seem to me that [Patient A] had been upset by my conduct. I apologised for it in another message a few days later; and thought that was accepted. The Complaint 27. It is alleged that I am guilty of unsatisfactory professional conduct for failing to observe proper- professional boundaries. I accept that although / was not [Patient A’s] treating psychiatrist at the time and had not been, 24 in a proper therapeutic, treating sense, for several years, That I should riot have allowed boundaries to be blurred in 2008. I accept that it is not conduct of a high standard. However I do not admit that I am guilty of unsatisfactory professional conduct In relation to the Particulars of The Complaint 28. I do not admit that / knowingly exchanged personal messages with a patient on RSVP. I do not admit that the exchange of personal information or discussions in the limited circumstances that it occurred, was a breach of professional boundaries, or unsatisfactory professional conduct 29. / admit I telephoned [Patient A] and suggested we meet. I admit we met and had dinner 30. I do not admit That I kissed [Patent A]. / admit I may have hugged her 31. / do not admit! touched heron the inner thigh. 32 1 do admit her breasts were mentioned in a conversational context. 33. I do admit that having a personal relationship dinner." was discussed at The 90. Dr Wade gave oral evidence to the following effect. 91. Dr Wade responded to questions concerning his late wife’s illness. He confirmed that his wife had died within a year of the initial diagnosis. He described both her diagnosis and death as being "traumatic". The date of his wife’s transplant operation had coincided with his mother’s funeral. Or Wade said that following the transplant the indications were very good. However, after two weeks complications arose between the graft and the host. As a consequence his wife was unable to eat and required nutrition through a central line. 92. Dr Wade was asked how he prioritised matters at that time. He described how his wife had suffered pain, insomnia and was very lonely. She had asked him to stay with her at the hospital which he did. Dr Wade recalled that there were often significant emergencies in the middle of the night such as haemorrhaging and he had assisted the nurses with his wife’s care. Dr Wade said that he did not consider his own needs. He said that his wife had also used him as an ’interpreter" to help her understand the advice being given by the haematologist. He had worked with the haematologist as an intern. Dr Wade said that he was trying to have some sense of hope in circumstances where his wife’s physical state was deteriorating. He described himself as being in "a state of holding an awful lot inside’ in his roles as a husband and father and in "keeping up appearances". 93. Dr Wade accepted that in October 2008 he had acted in a way in which he should not have acted in relation to Patient A. He was asked how he felt about his failure in relation to Patient A. Dr Wade responded "I was horrified really". He referred to the "bizarreness of it alt’, his disregard for Patient A’s welfare, that he was not thinking about Patient A and what his appropriate role 25 was. He said that he felt ’enormous shame" and described his conduct as "totally inappropriate". 94. Dr Wade confirmed that he knew about Patient A’s history of sexual abuse at the age of 3. He further confirmed that he knew because of the contents of what he had be told by Patient A and his experience as a psychiatrist that Patient A was vulnerable and fragile with regard to the issue of trust concerning men. Dr Wade described what he had done as "horrific" in failing to keep appropriate boundaries. He said that he was "exquisitely shameful" of his "wanton disregard and unawareness" of Patient A’s vulnerability. Dr Wade agreed that he had the knowledge and awareness of the ethical issues with regard to Patient A and had lapsed notwithstanding that knowledge. Dr Wade observed that his behaviour regarding Patient A "did not gel with who lam as a person or a psychiatrist" 95. Dr Wade was asked about his reflections in relation to his general standards and his behaviour concerning Patient A. He said that he had felt shame and guilt and had to try and live with himself. He said that he had failed Patient A and he was "trying to get a handle" on the perspective of how he behaved in an out of character way. 96. Dr Wade was asked to describe the kind of material posted on the RSVP website in addition to a photograph. He explained that the information generally included interests, hobbies, tastes in music, social life, sporting life and information about a persons background such as whether a person has children or is divorced. The system has a facility to enter a postcode and nominate a distance from that postcode. He had set his distance on the basis of convenience. 97. It was noted that Patient A had used the terms ’coincidental" and accidental" in referring to their contact. Dr Wade was asked how he made contact with Patient A. Dr Wade explained that Patient As photograph was not very revealing as she was wearing a long red coat with a high collar, long hair and large sunglasses. He said that he did not recognise Patient A in her photograph and had ’?io idea" that it was her. It became apparent that he knew Patient A from one of her email responses when she saw his photograph. The internal email system within RSVP does not use the parties’ private email addresses. 98. Dr Wade recalled that once Patient A realised who he was she was quite shocked that he was a widower. It was at this time that Patient A had sent him a private email and they exchanged emails. The major focus of this email correspondence was his late wife and what had happened to her. Patient A then sent him her phone number. 99. Dr Wade was asked, having regard to the treating relationship, how he perceived his professional relationship with Patient A at that time. Dr Wade responded that he considered any personal relationship inappropriate but considered the status of his treating relationship with Patient A was "on hold". He said that there was no formal arrangement after he ceased seeing Patient A on a regular basis she had "just left". However, he had been contacted subsequently in 2005 after Patient A had been hit by a car and he had received a request from an insurance company to write a report. 26 100. Dr Wade recalled that Patient A had given him her mobile phone number and he thought that he had given her his mobile phone number. He considered that it was highly unlikely’ that he had given Patient A his home phone number. 101. Dr Wade was asked about Patient A’s interest in him and whether there was any question of a relationship developing at that time. Dr Wade recalled that when he had explained what happened to his wife, Patient A had questioned whether their contact was accidental or whether he indentified her on RSVP and would be interested in a relationship as Patient A did not think that their contact was "happenstance " Dr Wade said that he had explained that a relationship was inappropriate having regard to the amount of privileged information he had and the imbalance of that and the issue of transference. He said that he had explained this in a "lay manner". 102. Dr Wade confirmed that Patient A did attempt to her friends but he had declined. 103. Dr Wade confirmed that he had no further personal contact with Patient A until she came to see him in May 2008. "match make" him with one of 104, Dr Wade was referred to Exhibit A tab 4. He confirmed that he was on notice that as at 22 April 2008 Patient A considered he was her treating doctor. 31 105. Dr Wade was referred to the transcript of his medical records for the consultations on 15 May 2008 and 1 June 2005.32 He confirmed that he had heard Patient As oral evidence regarding her concerns about taking Tramal and Aropax. Dr Wade reviewed the records and recalled that Patient A came to see him on 1 June 2005 to discuss her medications. He said that Tramal and Aropax are dangerous in combination and he had told Patient A to cease the medications if not required. He said that the principal purpose of the consultation on 15 May 2008 was about ongoing work problems related to her employer. He said that he was not aware of the paper work from her employer until the morning of the consultation and did not know that Patient A was coming to see him until that day. 106. In responding to questions concerning the consultation on 15 May 2008 Dr Wade explained that if Patient A had revealed that within the last calendar year she had been admitted to James Fletcher Hospital with a breakdown he would have "oriented" towards this and noted it in his records. He considered that he would have done so whether the consultation was for either psychiatric problems or medico-legal purposes. Dr Wade was asked what he would say in relation to the prospect of Patient A reporting a 2 week admission. He said that he would have remembered this and was unaware of Patient A’s breakdown or admission at the time. 107. If he had known about Patient A’s admission after his contact with her via RSVP and before October 2008 Dr Wade considered that he may have Exhibit A tab 4 page 2. A manuscript letter dated 22 April 2008 from Patient A notifying her employer at the time of a change in her treating medical practitioner and setting out Dr Wades name and address. The employer subsequently wrote to Dr Wade on 7 May 2008 see Exhibit A tab 4 page 32 Exhibit A tab 4 27 behaved differently as he had been characteristics. "imbuing" Patient A with a lot of 108. Or Wade was asked about Patient As presentation in 2005 and 2008 relative to the period of her intense treatment from 1999-2003. Or Wade said there was a mistake in 2005 in terms of the doctor putting her on a wrong medication" and he had seen Patient A "out of the blue" and he did not think that he had prescribed Aropax for Patient A. After referring to his medical records Dr Wade described Patient A in 2008 as being more aware and accepting of herself as compared to 2003. He said that one of Patient As big problems was people but she had shown more resilience in handling people and "there was no objective behavioural evidence that contradicted that". 109. Or Wade responded to various questions concerning the dinner with Patient A on 12 October 2008. He could not recall when he first made contact with Patient A prior to the dinner. He noted that "it all happened quite rapidly" and commented "I don’t know why it happened". He had phoned Patient A on her mobile phone having ascertained the number by looking up old emails from the 2007 period when Patient A had sent him her mobile phone number. 110. Or Wade was asked what was the purpose or what was he planning in contacting Patient A. He responded "to put the proposition of a secret relationship". Dr Wade recalled that there had been about 6 communications (emails or phone calls) before the dinner, 3 each from himself and Patient A. 111. Dr Wade agreed that Patient A’s acceptance of the invitation had no relevance to his lapse in judgment. 112. Or Wade was asked whether there was any discussion of personal matters when Patient A consulted him "on medico-legal matters" on 15 May 2008. He recalled that after he had examined Patient A and excluded treatment, Patient A had asked whether his identification of her on the RSVP website was accidental and she had talked about the possibility of a having a personal relationship. Dr Wade said that he had explained that it "was inappropriate because of ethical issues and power issues etc’. 113. Dr Wade was asked to describe his perception of Patient A’s attitude when he proposed further contact in October 2008. Dr Wade recalled that Patient A’s first words to him related to it being a surprise given the way the 2 previous contact sessions ended. He said that Patient A suggested that contact be by text instead of phone and Patient A seemed enthusiastic about the idea of a meeting and was excited. 114. Dr Wade recalled that it was agreed they would meet at a certain time in a street in Newcastle where there are number of restaurants and see what was available. He said that the dinner lasted from 11,4 -2 hours and they shared a bottle of wine, chatted and ate. 115. Dr Wade said that he had already had a phone conversation with Patient A about a possible relationship and he understood that this would be discussed at the dinner. He recalled that very little" was said about a proposed relationship at the dinner rather there was more "talking around the subject". He said that they had talked about "where they were at" with present and past 28 personal relationships. Or Wade acknowledged that he had spoken with Patient A about having a parallel" relationship with her. He said that Patient A did not express "verbally" that she wanted a more permanent relationship but had expressed this "by inference" several days later. 116. Dr Wade was asked when was the first time he had "heard alarm bells ringing" in relation to his behaviour with Patient A. He responded that to some extent even before the dinner he was suffering anxiety and adrenaline-like symptoms but he proceeded "over the top of that". 117. Or Wade was asked whether there were any worrying aspects or concerns in relation to the dinner. He responded that he was going through the motions; "/ wasn’t worrying and that is a worrying thing’ - ’there wasn’t enough thought going on". 118. Dr Wade recalled that after the dinner he had walked Patient A to her car which was parked near the restaurant, said goodbye and "gave her a cuddle and a peck on the cheek". He could not recall if he did kiss Patient A on the lips but agreed that he would be likely to remember this. Dr Wade denied that he had run his hand up the inside of Patient As leg. He observed that the car park was "quite a crowded public place and there were young people there". 119. Or Wade said that he thought any reference to breasts arose out of a reference to his late wife and an odd comment he made that one of her perceptions or beliefs was that "the health of the breasts related to the health of a woman’. Dr Wade did not recall saying "nice (its" and commented that this would be something he would be likely to remember. However, he did recall Patient A saying she had lost weight and her breasts were smaller. 120. Or Wade acknowledged that he was the author of the text messages reproduced in Patient A statement dated 9 February 2011. 121. Dr Wade was asked to comment on the text message he sent to Patient A on Monday 13 October 2008 at 858am which reads as follows: "HI ..., also enjoyed last night, much lust and desire, doubtful if you are cut out for the ambiguity of the role, main thing is for you to be selfish and decide what’s for you. Regards and Kisses Doug" He recalled that this was sent in reply to a text message from Patient A which had been "something to the effect that it was good to catch up". 122. Dr Wade was asked about a further text message on 13 October 2008 from Or Wade reads: "Hiya, sorry but lam in no position to vouch for you for anything with any third party. Regards Doug’ Dr Wade explained that the text related to him being a referee for a potential job a He said that he had realised that he was not able to be a referee Eecavuse of the contradiction of being in a secret relationship. 123. The next text message on 15 October at 1255pm reads: 29 "Hi .. thinking all a mistake taking you out of comfort zone, doubting own motivation. Sony but I think need to let go of fantasy of safe secret relationship. Regards Doug." Dr Wade said that he realised within himself that he had attributed unrealistic characteristics to Patient A related to being a saint, having wisdom and understanding; reality set in and that was not her. He concluded that what he was doing was "madness - it had to end - it was not right. 124. Dr Wade said that he did not initially think about Patient As vulnerabilities at the time but was more shocked about what he had done and about going against what was right and proper. 125. Dr Wade considered that he left the situation in a "shoddy state’ as he had treated Patient A "badly" and "behaved badly towards" her. When asked how he should have behaved Dr Wade responded that he should have been more forcefully apologetic in the genuineness of his remorse and grief. In his view a further personal meeting would not have helped but a sensitively worded letter of apology may have been appropriate. 126. In cross-examination Dr Wade described the nature of his communication with Patient A on the RSVP website. He said that the initial contract involved superficial niceties and when Patient A asked for his photo and she realised who he was she rapidly moved to sending personal emails outside the RSVP system and then contact was by phone. 127. Dr Wade estimated that he may have seen Patient A 30 times over a 5 year period. Dr Wade was taken to his report of 16 May 2000 in which he set out 13 dates on which he had seen Patient A in the period from 29 July 1999 to 10 Dr Wade continued to maintain his estimate of 30 times noting May 2000 He confirmed that consultations were for that the frequency "fell of’. approximately 1 hour. He said that he did not take notes at each consultation as he does not take notes unless there are significant changes in history, mental state or treatment. Dr Wade explained that he has now changed his practice had "got out of the dinosaur period" and currently it would be "exceptional" for him not to write something down. 128. Dr Wade confirmed that Patient A had been referred to him by her general practitioner in May 2008? It was noted that the referral from her general practitioner recorded that Patient A felt anxious and depressed and had difficulty sleeping. When it was put to Dr Wade that the referral was not solely about workers compensation matters he responded that it was "really about workers compensation problems" and a particular woman in the workplace who made Patient A feel uncomfortable. Dr Wade agreed that he did not expect Patient A to attend the consultation and tell him she was ’OK’. 129. Dr Wade did not recall having been informed by Patient A that she had been admitted to James Fletcher Hospital. He did not recall commenting at the consultation in May 2008 on Aropax being prescribed for Patient A. Dr Wade did not agree that Patient A requested medication at the consultation. The report was prepared for solicitors for the purposes of a workers compensation claim by Patient A, Exhibit A tab 4 at page 77. Exhibit A tab 4 at page 12. The referral is date 21 May 2008. 30 130. Or Wade was asked several questions about his medical notes for Patient A. 35 Or Wade considered that his notes for Patient A were accurate with regard to the history he took although he is now "more mindful" when taking notes. It was put to Dr Wade that the only times he took detailed notes was in July 1999 and May 2008. He said that he could not explain why he had taken more detailed notes at those consultations. 131. Or Wade was asked about 2 entries in his medical records for Patient: "26.09.01 Aropax, 30mg x 20 x 30 x 5..." and "19.03.02 Aropax 20 x 20 x 30 x 5"... Dr Wade said that the entries related to medications prescribed by other specialists or general practitioners. 132. Or Wade agreed that Patient A suffered from PTSD, had a problem with trust and was very distressed when she came to see him because of a breach of trust. Dr Wade noted that this was often work based. Dr Wade also acknowledged that he was in a position of trust in relation to Patient A especially with regard to her difficulties with men. Dr Wade could not recall whether Patient A had informed him it had been recommended that she should see a male therapist. 133. Dr Wade agreed that after the exchange of text messages with Patient A in 2008 that the next time he became aware of the mailer was on 15 October 2010 when he was contacted by the HCCC. 134. Or Wade was referred to paragraph 26 of his written statement and it was suggested that he did not give much thought to his conduct until he was contacted by the HCCC. Or Wade said that after he sent the final text to Patient A he still had an "odd feeling" and when he understood what he had done it became "encapsulated in shame". Or Wade explained that it was a mailer of ’shut the door or actively blocking off... of having done something shameful" and when he received the letter of complaint "the doors opened up on all this shame and after this time...! had the perspective of how awful and ghastly it was for [Patient A] having her trust betrayed.’ 135. Or Wade was taken to paragraph 20 of his written statement in which he referred to a "kind of insurance against more loss" and paragraph 21 where he also referred to "kind of secret insurance". He described his logic at the time as being ’bizarre"- 136. Or Wade agreed that he put his own needs before those of Patient A. Whilst Or Wade accepted he had offered a relationship to Patient A he also stated that Patient had made offers to him. 137. Or Wade agreed that he did not intend to tell his new partner about any affair with Patient A and as a consequence was contemplating deceiving her. 138. Dr Wade said that his decision not to follow through with a relationship with next couple of Patient A developed rapidly starting at the dinner and over the days". Dr Wade described the process as being ’driven by fear". He subsequently referred to a "growing realisation that it was a crazy proposition". Exhibit A tab 4. 31 139. Dr Wade agreed that it was possible that he kissed Patient A but did not recall doing so noting that he "doubts it very much". 140. Dr Wade was asked what he meant by "characteristics of maturity and self reliance" referred to in paragraph 23 of his written statement. He said that he was entrusting Patient A with characteristics that she did not have, such as maturity and self-reliance, of having some ’false sophistication". He described this as illogical at the time and devoid of reality. 141. It was noted that the dinner occurred approximately 2 1/2 years after Dr Wade’s wile had died. Dr Wade was asked how he was feeling at that time. Dr Wade said that he was about 80 per cent back to his normal self at the time of the dinner. He described himself as being "in a fairly good place"; he was recovering from his grief and his new relationship had grown in importance but had become a major threat because he was afraid of history repeating itself given that he had lost his wife and was afraid of entering into a new long term intimate relationship. 142. Dr Wade recalled that at the dinner he and Patient A had spoken about partners, children and holidays. He said that he was not sure there had been a second reference to the proposition that Patient A become his mistress as this was taken as a given but he had tried to "rationalise his logic" to her. 143. Dr Wade confirmed that his late wife had been discussed at the dinner, however, he had previously given Patient A a more detailed explanation and the discussion related to his fear of losing someone. 144. Dr Wade denied that he made any comment about Patient A’s breasts. He recalled that Patient A had made a comment that she had lost weight and her breasts had become smaller. 145. Dr Wade was asked whether he considered that Patient A was a patient when he contacted her about the dinner. He said that he did not consider that she was a current patient in terms of "my logic at the moment and somehow / had imbued her with characteristics which helped with the lies I was telling myself’. 146. It was noted that Dr Wade had seen Patient A for 5 years and subsequently at intervals of 2 years and he did not know when she may have returned for a further consultation. Dr Wade agreed with this proposition and confirmed that he had never officially concluded the therapeutic relationship with Patient A. 147. Dr Wade confirmed that he did not seek any help from psychiatrists or psychologists whilst grieving for the loss of his wife. He said that he had thought about some psychological assistance but had "rationalised" himself out of that and determined that he did not need such assistance because he had a peer group. He said that the peer group "do not pull punches" and if he needed outside help they would say so. 148. It was noted that Dr Chenoweth had given evidence about Dr Wade’s understanding of boundary violations. Dr Wade referred to the importance of boundaries and maintenance of safe boundaries even in non-therapeutic relationships. He said that it is fundamental to maintain respect for others’ 32 feelings, rights, intellectual property and within the psychiatric area it is "sacrosanct". 149. Dr Wade was asked whether he had done anything since to ensure that he does not make a similar mistake. He said that the main issue is ’connectiveness" and he had held a lot in" and become too isolated during his late wife’s illness. Dr Wade considers that he is now more "connected" and has "humility" in knowing his "vulnerabilities and potential vulnerabilities". 150. Dr Wade responded to questions from the Committee. 151. It was noted that Dr Wade had given evidence that he did not prescribe Aropax for Patient A yet in his medical records there were references to Dr Wade agreed that he probably prescribed Aropax in 2001 and 2002. Aropax on those occasions about 6 monthly. 152. Dr Wade was taken to the referral from Patient A’s general practitioner dated 21 May 2008_ 37 It was noted that the referral was a formal referral which indicated that Patient A was anxious/depressed and clearly had problems. Dr Wade was asked whether he wrote back to the referring general practitioner. Dr Wade responded "it would have been a normal practice but it doesn’t look as though I did". 153. Or Wade agreed that there was no conclusion or treatment plan in relation to the review recorded in his medical notes. His recollection of how the consultation ended was that Patient A had problems but was handling them well. This was not documented. 154. It was noted that Dr Wade had described a period of great distress during his ate wife’s illness. He was asked what impact this had on his practice. Dr Wade recalled that during his wife’s illness the practice "ground almost to a halt" and when it started to build up again ’the main problem was debts; the accountant’secretanj was robbing me and she disappeared". He said that he had been fairly dependent on being a psychiatrist; going to work and being in the work environment. He observed that in some ways the period made him a better psychiatrist in understanding other people with significant losses. Dr Wade explained that the practice slowly built up again from March/April 2008. 155. Dr Wade confirmed that he had not raised the issue of Patient A’s complaint with Dr Chenoweth until after he was first contacted by the HCCC in 2010. He said that he subsequently discussed the matter with other members of the peer group within a "few weeks". There are 5 members of the peer group including Dr Wade. 156. Dr Wade outlined the nature of his current practice. He described his practice as being dominated" by patients suffering from PTSD; including war veterans, police officers, ambulance officers, emergency service workers, miners and workers in heavy industry. Many of these patients suffer from chronic PTSD. There is a significant workers compensation aspect to his practice. He works 4 days per week; consultations are usually for 1 hour and he usually sees 7 patients in a day. Referrals are mainly from general practitioners. He has an Exhibit A tab 4 at page 7, Exhibit A tab 4 at page 12. 33 interest in obsessive compulsive disorders; he has few psychotic patients and no admitting rights. Since 2006 the same person has performed the role of receptionist/secretary and office manager. Dr Wade shares his consulting rooms with a psychologist. When asked about his computer skills Dr Wade responded the he was ’a bit of a Iuddite’ Dr Wade said that he had become more aware that he needed to take more contemporaneous notes. 157. In re-examination Dr Wade indicated that he planned to reduce his workload in the future for health reasons which he outlined to the Committee. He said that he had no intention of seeking admitting rights. Dr Wade confirmed that when he experienced the period of shame and self-reflection in October 2008 he did not consult anyone and dealt with the matter himself. 158. Dr Wade considers that he had a good reputation amongst his colleagues for his reports and letters concerning patients. He said that generally he would see a patient a few times before reporting back to the referring doctor. Currently if he is confident with his diagnosis he will have "a 3 page response" back to the referring doctor within weeks. If the diagnosis is more ambiguous he will write something short and follow up when he is more confident of a diagnosis. REASONS FOR DECISION 159. The Committee has considered the evidence in the context of the legislative framework established by the National Law. The meaning of unsatisfactory professional conduct and the onus of proof have been previously noted. The Committee must be reasonably satisfied in relation to any findings that it makes. In reaching its conclusions the Committee has taken into account the seriousness of the mailers, the inherent likelihood of an occurrence of a given description and the gravity of the consequence flowing from a particular finding. 160. In its deliberations the Committee has also had regard to the Complainant’s written submissions, Dr Wades written submissions and the Complainant’s submissions in reply. 161. Whilst significant aspects of the evidence are not in dispute there are important factual divisions between Patient A’s evidence and Or Wade’s evidence. The submissions made on behalf of Dr Wade contend that Patient 38 A is an "unreliable witness and her evidence should be treated with caution" The submissions acknowledge that Dr Wade’s decision not to cross-examine Patient A left parts of her evidence unchallenged but purport to traverse those matters by referring to some aspects of her evidence which are allegedly "confused or conflated" and contend that little weight can be placed on much of Patient A’s evidence and any finding based on her evidence would not be consistent with the principles enunciated by Dixon J in Bdginshaw 39 Having considered Patient A’s evidence and presentation before the Inquiry the Committee is not persuaded by the submissions made on behalf of Dr Wade on this issue. It follows that the Committee must have regard to evidentiary Respondent’s Submissions at paragraph 21 op. cit 34 consequences which follow from Dr Wade’s failure to challenge key aspects of Patient A’s evidence by cross-examination. The Particulars 162. The Committee must determine whether the Particulars of the Amended Complaint have been proven to the requisite standard. Relevantly, Dr Wade has admitted to a number of the Particulars. The Committee notes that findings to the effect that one or more of the Particulars have been proven may not necessarily support a finding of unsatisfactory professional conduct in terms of section 139B (1) of the National Law. 163. For convenience the following commentary also includes some aspects of the written submissions which deal with the possible consequential findings by the Committee in the event that the Particulars are found proven. The Preamble 164. The facts set out by way of background in the Preamble to the Particulars are not in dispute. Particular I 165. Particular 1 describes the substance of the Amended Complaint and alleges in general terms that Dr Wade failed to observe proper professional boundaries. The alleged factual circumstances which purport to support the allegation are then set out in various sub-paragraphs. The Committee proposes to deal with these seriatim. Paragraph 1.1 1.1 In 2007 the practitioner: 1.1.1 exchanged messages of a personal nature with Patient A on the RSVP website; 166. Dr Wade does not admit Particular 1.1.1. 40 The Complainant contends that in cross-examination Dr Wade admitted to an exchange of superficial niceties" between himself and Patient A on the RSVP website and these were "of a personal nature and not in relation to his professional relationship" with Patient A’ 1 167. Dr Wades written submissions contend that the contact was inadvertent. It is submitted that it is not a significant failing of any professional standard, or or improper conduct to communicate with a person on a dating unethical website. The only personal information that was exchanged was their respective identities and some innocuous further contact. For this Particular to be used as a basis for a finding against Dr Wade, there must be something more than mere contact occurring. There was no pursuit of any kind of [Patient 40 Exhibit I tab 5. Complainant’s submissions at paragraph B. 35 ate in the A] via the RSVP website, there was nothing im 2pro per or inappropri contact or the limited exchange of information". 4 Finding 166. The Committee is reasonably satisfied that Particular 1.1.1 is proven to the requisite standard. 1.1.2 after contact with Patient A on the RSVP website, spoke with Patient A by telephone and/or exchanged emails with Patient A and discussed personal mailers. 169. Although Dr Wade admits to the facts in Particular 1.1.2 his written submissions endeavour to address any potential adverse implications arising from his admission by contending, for example, that there was nothing sexual in the emails’43. It is further submitted: 28. It is not a breach of professional boundaries to exchange personal information with a patient It is a question of how often, how much, the content and extent of the personal information and the context of the exchange9 On Dr Wade’s evidence there was not a lot of contact, and it was [Patient A] who initiated the discussion that roamed into the area of personal, as in romantic, relationships. . 29. She had assumed, quite understandably, having encountered him on the RSVP website, that Dr Wade was seeking companionship. [Patient A] had therefore, come into know/edge of Dr Wades personal life without any action on his part and decided to act on it. Or Wade cannot be held responsible for this. 30. It is not the case that the practitioner contacted a patient, in an unsolicited way, to discuss personal mailers of an inappropriate nature. Apart from a somewhat desultory exchange of information, which, in our submission is not sufficient to establish any allegation of unprofessional conduct there was further personal discussion, which was not initiated by Or Wade. 31.1n support of this Particular, the Complainant relies on the evidence of [Patient A] however on this issue [Patient A] is supportive of Dr Wades account that he rejected her proposals that included social contact (the proposed barbeque) and ’matchmaking’ of Dr Wade with her fiiend.fs. There was no pursuit of [Patient A] (one may have expected him to accept the invitation if he had harboured an intention to maintain contact) and no relationship. 32. Neither limb of this Particular is made out as a failure to observe professional boundaries, or as evidence of a failure in terms of the d2 Respondent’s submissions at paragraph 25. Respondent’s submissions paragraph 26. 36 exercise of care, skill and judgment on the part of Dr Wade’s clinical practice. Nor, in our submission, does it support a finding of other improper conduct in the practice of medicine. [9. See Re Dr C op cit. at [97] conversations regarding a practitioner’s and patient’s respective personal life and respective marriages, during a consultation with the patient may have been imprudent and want judgment but did not amount to a breach of standards or improper conduct.] Re Dr C [2010] NSWFC 17 Finding 170. The Committee is reasonably satisfied that Particular 1.1.2 is proven to the requisite standard. 1.2 Between about 1 and 12 October 2008 the practitioner made telephone calls and sent text messages to Patient A in which the practitioner: 1.2.1 suggested that the practitioner and Patient A have a personal and/or sexual relationship; 171. Whilst Dr Wade admits to the facts in this Particular the written submissions made on his behalf endeavour to limit any consequences which might flow from this admission. The relevant submissions are as follows: 33i Dr Wade has admitted the facts of this Particular He agrees that he invited [Patient A] to meet with him, and to discuss the offer she had made earlier to him to embark on a personal relationship, although the exact content of the discussion is not clearly recollected. He does recall that [Patient A] was surprised because he had told her in 2007 and again in 2008, that it was inappropriate. [Patient A’s] evidence about her reaction to the contact in late 2008 in fact supports Dr Wade’s account on this issue34. Dr Wade has explained that when she came to see him in May 2008, [Patient A] repeated her suggestion that the two of them could have a relationship. Dr Wade said that [Patient A] brought up the subject of the RSVP coincidence. [Patient A] in evidence and her statement of 9 February 2011 states that Dr Wade brought up the subject of the RSVP connection. In our submission that is inconsistent with the notes of the consultation, indicating a reasonably lengthy discussion during an hour-long interview, about [Patient A’s] current work situation, and current state of mental health, which he said seemed to be good. Dr Wades’s [sic] notes support this account. The reason for the visit, according to Dr Wade was in relation to a Work Cover claim at her employers, ... This is also reflected in the Medical Record. Notwithstanding the referral, the Committee will see correspondence both to the Dr’s rooms by [Patient A’s] then employer, ..., and by email from [Patient A] to the CTT Tribunal consistent with the purpose of the 2008 consultation being largely concerned with her employment dispute and need to provide medical support for it Those materials and most of the consultation notes in no way align with the extended 37 account given by [Patient A] to the Committee of the consultation. 35. [Patient A’s] evidence was that the principal reason for the consultation was for medication. This is not the mason given in the referral, and is inconsistent with the notes taken at the time. Indeed it also inconsistent with the outcome, which was that no medication was prescribed. 36. Dr Wade denies he made any advances, sexual or otherwise, to [Patient A] during the consultation, as he denies the alleged pursuit of [Patient A] from the first contact in 2007, until October 2008, which is the thrust of her written statement. We submit that Dr Wade’s evidence should be accepted on this point and we refer to the matters put generally as to credibility earlier in this submission. 37. Dr Wade concedes that he contacted [Patient A] in early October 2006, however it was out of the blue’ which is again, in our submission more likely to be because he had not made any other attempt to pursue a personal relationship until this point He rang [Patient A’s] phone on a number (likely a mobile service) that she had provided to him at the time of the RSVP contact The Complainant did not put this issue in contest He said [Patient A] preferred to use text messages so they did. 38. [Patient A] broadly supports the account of Dr Wade on this part of the chronology, and has provided one of the text message sent by Dr Wade. There are no messages sent from [Patient A] in evidence. Dr Wade says that there was contact between them consisting of a number of calls and texts, including his proposition of an intimate relationship in a telephone call. The two accounts coincide as to the details of meeting in Newcastle and selecting a cafe once they had met 3 Dr Wade does not deny that by initiating contact in October 2008 of this kind, he blurred the professional boundaries between a psychiatrist and his former patient He has never resiled from the concession he made in his first response to the HCCC (Tab 8) that he should not have contacted [Patient A] and should not have invited her to dinner because, although they had no current treating relationship, in his view, he had been her treating psychiatrist in the past 40. In our submission, this conduct, whilst ill considered, does not constitute unsatisfactory professional conduct. It is sufficiently removed, in our view from clinical practice to not involve a significant falling in clinical judgment, and is not illustrative of a significant lack of care, skill or treatment 41. The Committee must consider whether, given the nature of the doctorpatient relationship, making contact at this point with [Patient A] is either a significant failing in an identified standard (i. a the deficiency expected to be identified by Childs v Walton) pursuant to s139(B)(1)(a) ora breach of 139(B)(1)(1) (e.g. by committing a clear breach of the sexual misconduct guidelines, however no evidence 11 was put before the Committee as to whether or not the guidelines were breached, and if they were, the extent to which they were). In our respectful submission the Committee, considering all the evidence and applying the proper tests, will not be comfortably satisfied of unsatisfactory professional conduct on either of the limbs conjunctively relied on by the Complainant 42. The suggestion of a personal relationship must be examined in context in the following terms: whether or not a doctor-patient relationship existed If it did, whether the professional boundaries of such a relationship were breached. If they were, whether the breach was serious enough to constitute unsatisfactory professional conduct 43. In October 2008, Dr Wade had seen [Patient A’s] once, 5 months earlier. Prior to that, he had seen her in the middle of 2005, and only once at that time. On both these occasions she saw him for reports for an insurance claim. She was not consulting him for any ongoing treatment for psychiatric problems, disturbances, episodes of depression, or illness. He did not consider that he was her treating psychiatrist and [Patient A’s] acknowledges that there was no existing therapeutic relationship, indeed she said that he had not been her psychiatrist for some time. In oral evidence before the Committee, however, [Patient A] attempted to change her position to the extent of saying that she considered he was still her doctor. 44. There is no argument that a therapeutic relationship of some significance had existed between 1999 and 2002 and then again for a period in 2003, so that it could be properly characterised as a doctorpatient relationship of some four or five years duration, and that during that time, [Patient A] was entitled to place her trust in Or Wade as her treating psychiatrist The establishment of that relationship is the basis upon which Dr Klug opined that it still pertained in 2008- In short his evidence seemed to be that once it existed it remained in existence. In our submission, it is not possible to accept that proposition. 45 In October 2008, it is debatable that the former relationship still existed. Dr Klug ’s opinion was that it did. Dr Wade and [Patient A] seemed to think it did not although both moved from that position in oral evidence, particularly [Patient A]. In our view, it is appropriate to proceed on the basis that [Patient A] was a former patient, and that no therapeutic relationship was in place at that time. It is then appropriate to scrutinise the conduct of the practitioner and the effect of it on his former patient to determine whether or not the Complaint is made out 46. There was no evidence from [Patient A] that she felt at all imposed upon by the invitation to meet with Dr Wade, and from her oral evidence she did not appear to find the invitation to entertain the possibility of a personal relationship, such as a mistress, out of all consideration. [Patient A] did seem to take affront, however her evidence was unclear as to the reason for this but she seemed to say 39 either that she thought it was odd because he was moving in with his girlfriend and was not the ’man in terrible grief she expected to find. It is submitted that she was not overborne into accepting the invitation, or the victim of predation. [Patient A] was adamant that she had significant strength not to go down the path of being a mistress, in fact, calling such a thing ’masochism’. 47. Notwithstanding [Patient A’s] own view of her strength of mind and character, she was a former psychiatric patient whom Dr Wade had treated for some time, for PTSD in particular. Her background included claims of child sexual assault, and issues of trust, particularly regarding those with whom she worked and by whom she felt let down. [Patient A] also attested to the difficulties she had in trusting men. [Patient A] was, certainly on a prima facie view of her history, likely to be a vulnerable person for whom Dr Wade was a person of superiority in terms of the balance in the doctor/patient relationship that existed, and he would likely to continue to be seen in that light once that doctor/patient relationship ceased. The possibility of emotional vulnerability was a matter that should have been considered by Dr Wade, regardless of the effiuxion of time. However, our submissions, which are supported by Dr KIug’s opinion, is that Dr Wade was not cynically exploiting [Patient A’s] emotional vulnerability, but had permitted hirnself, as Dr KIug says, to introduce personal issues into the doctor/patient relationship 48. There is no denying that a degree of dependence would have developed during the time [Patient A] saw Or Wade regularly, however by 2008 it is unlikely, on any view, that [Patient A] was dependent on Dr Wade for psychiatric, or medical support, except so far as the compensation claim is concerned. The evidence does not support the proposition that Dr Wade exploited any dependency on him as a medical practitioner. Any such dependency that had existed during the time he treated [Patient A], had long since past 49. Our submissions are not an attempt to detract from Or Wade’s own consideration of his conduct, but it is important, in our view, that the Committee consider the matter from both [Patient A] perspective and from Dr Wade’s - and with due acknowledgment that Dr Wade was probably wrong in his assessment of the situation when he imbued her with characteristics’ of sophistication, maturity and self reliance. As far as he was aware, at that time, in Ocotber [sic] 2008, [Patient A] was not in need of psychiatric therapy, and had not been for some years, she was not considered by him to be suffering from any particular disability and was not then on regular medication". His impression, having seen her in May 2008 was that she was well and doing well. He had no know/edge of anything to the contrary. He had no knowledge of her breakdown in, apparently, mid 2007- It had not been mentioned either in conversations they had in 2007 (the timing of which is unclear) or at the consultation in 2008, on his evidence. Dr Wade said he would consider it (i.e. a two week admission) a significant matter and it would have not only appeared in his notes but affected the orientation of the 2008 consultation (and subsequent considerations). 40 f’ ln contrast with (Patient A’s) evidence on this point, the referral fetter to be found in the Medical Records asserts that the patient had not been on Aropax for some time.) 50. It is accepted that there is an absolute prohibition on sexual relationships with patients and that may extend to former patients. It is accepted that having a very close social relationship with a patient may breach the professional boundaries between a practitioner and his patient, but whether it is as serious an issue with former patients will depend on the particular circumstances. The Commission’s submissions, and indeed the questions put to witnesses on this point, tend to focus on the fact of a relationship and the prohibition of entering into a sexual relationship. No physical, sexual relationship was ever entered into. A meeting over dinner is not, in our submission, a relationship. 51. The mere contemplation of entering into a social relationship, or even a sexual relationship, in the absence of any other relationship developing, with a former- patient is not, in our submission, enough to constitute unsatisfactory professional conduct It might be a step along a process towards such conduct, and it may be an indication of a willingness to transgress boundaries at some point in the future, but in our submission, given the length of time since [Patient A] had been a psychiatric patient under Or Wade, this Particular does not establish unsatisfactory’ professional conduct under either sub paragraph (a) or (1). We submit that the Commission should not be accepted when it submits (HCCC submissions, paragraph 38) that Dr Wade contemplated a sexual relationship with [Patient A] prior to October 2008. He acknowledges that he had in mind, in a somewhat abstract way, a sexual relationship when he spoke to her in early October, and that this notion had dissipated, and then disappeared entirely, by 15 October This is what the evidence supports and this is the highest that the case against Or Wade can by [sic] put 52. It is not argued that this actions in contacting [Patient A], represents sensible, or even responsible, behaviour on the part of a practitioner. It is argued that it is not sufficiently serious to constitute unsatisfactory professional conduct, and because it has not been Particularised as a deficit of practice, as required by Childs v Walton, and is not sufficiently close in temporal terms to the doctor patient relationship, and did not arise out of clinical practice, for example, an invitation made in the course of a consultation or ongoing treating relationship, or otherwise in the practice of medicine. 53. Dr (<lug’s opinion that Dr Wade’s conduct is significantly below standard is an opinion wedded to the definition of unsatisfactory professional conduct in s39(B)(1)(a). His opinion was predicated on the existence - which still pertained in his opinion - of the doctor patient relationship, and applying the test of s39(B)(1)(a). In our submission, the Commission has misdirected Dr kiug when seeking his opinion. He has been asked to direct his attention to the wrong 41 questions, and has given no opinion on a possible breach of s39(1)(1). 54. This evidential difficulty for the Committee is further compounded by Dr KIug’s statement that the conduct in question attracts only his mild criticism, which although confusing gives support to our submission that the conduct Particularised here is not sufficiently serious to amount to unsatisfactory professional conduct deserving of the consequences that such a finding would invite. Finding 172. The Committee is reasonably satisfied that Particular requisite standard. 1.2.1 is proven to the 1.2.2 suggested that the practitioner and Patient A meet for coffee or have dinner together. 173. Dr Wade admits to the facts in Particular Finding 174. The Committee is reasonably satisfied that Particular requisite standard 1.2.2 is proven to the 1.3 On or about 12 October 2008 the practitioner met Patient A for dinner; 175. Or Wade admits to the facts in Particular submissions: 13 and makes the following 55.Dr Wade admits that he and [Patient A] met, at his invitation. His initial suggestion had been for coffee that can be seen from a text exhibited by the Complainant and the evidence remains unclear about how that invitation converted to a meeting, and then a dinner 56-Had [Patient A] been a current patient undertaking therapy, this would be an invitation that had the potential of bluffing of professional boundaries, and depending on the circumstances, could be likely to lead to confusion for the patient It is not so clear, in the case of a former patient, whether the same thing can be said. Such conduct may attract the censure of the Medical Council in the form of counselling, on referral from a complaint It would not automatically amount to unsatisfactory professional conduct of itself. This Particular, in our submission does not establish unsatisfactory professional conduct Exhibit 1 tab 5. ibid 42 Finding 176. The Committee is reasonably satisfied that Particular 1.3 is proven to the requisite standard. 1.4 On or about 12 October 2008, at or after having dinner with Patient A, the practitioner: 1.4.1 kissed and/or hugged Patient A; 177. Dr Wade admits that he hugged Patient A. 46 The Complainants submissions refer to Patient As evidence that Or Wade kissed her on the lips albeit not in a passionate manner. It is contended that the events had a strong impact on Patient A "which led to them being impressed upon her memory" and as a consequence Patient A’s "memory concerning these events would be clearer that Dr Wade ’s". 47 The Complaint’s submissions continue: 19Jn Dr Wade’s first response letter dated 21 October 2010, he does not strongly deny the kiss and instead suggests he cannot recall exactly what happened after the dinner. He admits there may have been a kiss on the cheek He stated ’[t]he physical contact I had with [Patient A] was very minimal and /think constituted a cuddle or a hug and maybe a kiss on the cheek when we said goodbye. In Dr Wades letter to the Commission dated 1 February 2011, Dr Wade admits his recollection of what was exchanged between himself and [Patient A] was not clear: ’I cannot recall what it was [the physical contact], but it was in a public place ... and would have been in the nature of a brief hug when we said goodbye.’ There is no mention of any kiss. In Dr Wade’s statement dated early April 2012 he stated ’I do not recall kissing [Patient A] (emphasis added). In examination- in-chief, Dr Wade stated there may have been a ’peck on the cheek’. Under cross- examination, Dr Wade said he ’doubted’ them was a kiss on the lips between himself and [Patient A]. 20. Dr Wade’s evidence was that he does not think he kissed [Patient A] or he cannot recall doing so and was somewhat inconsistent regarding whether there had been a kiss on the cheek or no kiss at all. Dr Wade elected not to cross-examine [Patient A] and challenge her account For the reasons outlined above, it is submitted that [Patient A’s] memory should be preferred to Dr Wade’s. Further, Dr Wade’s conduct in arranging the dinner, proposing that [Patient Al be his mistress and his text message the following day stating ’much lust and desire... all suggest that contextually, [Patient A’s] version of events is much more plausible. It is submitted that the Committee ought to be satisfied that this particular is proven to the requisite standard. 178. Dr Wade’s submissions on this matter are as follows: 57. Dr Wade’s evidence is that in saying farewell to [Patient A] he gave her a hug. He did not strenuously deny any kind of kiss as 46 Ibid. Complainants submissions at paragraph IS, 43 he has no clear recollection of kissing her or not kissing her, however he doubts he did so as he would remember that If there was a kiss, it was of a friendly, not sexual kind, and [Patient A] does not characteflse it as at all a big’ or pashy kiss. Both he and [Patient A] agree that he walked her to her car, and it is undisputed that it was in a public parking lot Dr Wade says them were people about He denies doing more than giving [Patient A] a hug, and he denies a kiss of any kind other than a peck on the cheek In our submission it should be accepted that it is unlikely that Dr Wade would have engaged in a public display of affection such as kissing [Patient A], molesting her by running his hand up the inside of her thigh (which would, in our submission, require a considerable amount of contact over and above the hug which Dr Wade says he gave [Patient A] and which evidence was not challenged) and commenting on her breasts in the manner alleged, whilst in full view and hearing of fellow Novacastrians. 179. The Complainant’s submissions contend that Patient A is a credible witness and her evidence should be accepted. The submissions made on behalf of Dr Wade respond as follows: 58. ... The Commission submits that [Patient A] was in fact experiencing shock at the conduct of Dr Wade, but that her ability to recall detail is unaffected In our submission, [Patient A’s] evidence in many respects is not reliable as she has confused and con fiated various matters throughout her written statement and oral evidence. The Commission acknowledges that her recollection is not perfect. In our submission, [Patient A’s] recollection is faulty. Both she and Dr Wade are attempting to recall an incident which occurred almost four years ago. [Patient A] did not make a complaint in relation to this for many months thereafter. The Commission submits that in the interim she reflected on this matter and for that reason her account should be given credence. There is no evidence as to the extent to which [Patient A] reflected on the events of that evening insofar as ensuring that her recollection was accurate. There is no contemporaneous statement in evidence and no corroboration. [Patient A] said that she was driven to making the complaint because she had been reflecting on all the negative things that had happened to her. She did not indicate that she had reflected particularly on the interaction in the parking lot and we submit it would be erroneous to take the accounts that she provided some years later, as the truth of the matter. 59. Dr Wade’s recollection is similarly imperfect, but, in our submission it is to be preferred. His evidence has been provided in a full and frank manner in both his written and oral evidence. He has freely admitted those matters which he accepts occurred, has provided explanations in an open way, made appropriate concessions where he cannot recall and is entitled to the benefit of the doubt in those matters where there is a conflict in recollections. 60. When considering this Particular, we submit that it is inconsistent, 44 for [Patient Alto initiate contact with Dr Wade via a text message (which has not be produced) the next morning, if she was experiencing the kind of shock distrust and disbelief that the Commission submits her evidence indicates. [Patient A] not only initiated contact with Dr Wade, she asked him for a reference. 180. Dr Wade admits that he hugged Patient A. The evidence with regard to whether he kissed Patient A involves quite specific recollections on the part of Patient A contrasted with uncertain and inconsistent recollections but not a strenuous denial on the part of Dr Wade. Moreover Patient As evidence has not been tested by cross-examination. On balance the Committee accepts Patient As recollection of the facts but notes that Patient A described the kiss as not being passionate. Finding 181. The Committee is reasonably satisfied that Particular 1.4.1 is proven to the requisite standard. 1.4.2 touched Patient A on the inner thigh; 182. Dr Wade denied this Particular. The Complaints submissions contend: 21. _[Patient A] gave both whiten and oral evidence stating that following the dinner in the catpark, Dr Wade ran his hand up her inner thigh after kissing her. In Dr Wades statement, he said he could not recall touching [Patient A] inappropriately: Under cross-examination Dr Wade said he ’doubted’ he had touched [Patient A’s] thigh Dr Wade did not cross-examine [Patient A] on this point The Commission again submits that [Patient A] was a credible witness, whose memory was superior to Dr Wade’s regarding these events. Finally, given the contextual background of the dinner date, it is submitted that [Patient A’s] version of event should be accepted. 183. The submissions made on behalf Or Wade question the reliability of Patient A’s evidence by referring to the submissions previously made in relation to Particular 1.4.2. Finding 184. On balance the Committee is reasonably satisfied that Particular proven to the requisite standard. 1.4.2 is 1.4.3 commented on Patient A’s physical appearance including, in particular, her breasts; 185. Dr Wade denies this Particular. The Complainant makes the following submissions: .[Patient As]evidence was that Dr Wade commented on her breasts 22 _[Patient saying ’great tits’ or’nice (usc following the kiss and touch of her inner thigh in the carpath, [Patient A’s] written evidence was consistent with her oral evidence. As [Patient A] was not cross-examined, her 45 evidence remains unchallenged. 23. In Dr Wades letter to the Commission dated 21 October2010 1 he stated; ’I do not recall commenting on her breasts but! do recall her mentioning that her loss of weight had reduced her breasts. If / made a comment that has offended her I apologise. Again Or Wades evidence is that he cannot recall and does not strongly deny the conduct Dr Wade seems to accept the possibility that he may have made a comment by his words if I made a comment..’ 24. In Dr Wades statement dated ean’yApdl 2012, he admits that [Patient A’s] breasts were mentioned in a ’conversational context’ In examination/n-chief, Dr Wade was asked to comment on the discussion regarding [Patient A’s] breasts. Dr Wade stated the conversation had arisen with a reference to his late wife who had believed that the health of a woman is reflected by the health of her breasts. Dr Wade acknowledged it was an ’odd comment’. Dr Wade only raised this conversation for the first time at the hearing. He was then asked ’was that part of the discussion regarding [Patient A] saying that she’d lost weight from her breasts?’ He then said yes that’s right’. He was then asked whether he said ’great tits’ to [Patient A] and he replied ’I don’t remember that happening.’ 25. The Commission submits, as was put to Or Wade in cross-examination, that it is likely that he made a complimentary comment regarding [Patient A’s] breasts. As discussed above, [Patient A] presented as a credible witness. Dr Wade ’s denials were weak, saying he ’doesn’t recall’ making the comment In his letter of 21 October 2010, he seems to accept the possibility that he may have made a comment that offended [Patient A]. Further, Dr Wade raised new evidence regarding the ’conversational context’ in which [Patient A’s] breasts were discussed on the day of the hearing. It is submitted that [Patient A’s] evidence should be preferred over Dr Wade’s and again that the conduct is likely given the kind of relationship that Or Wade was proposing to [Patient A]. 26. Finally, [Patient A] gave evidence that Dr Wade did not discuss his late wife at the dinner at all. She expected to see a ’grieving man’ and was shocked to hear about his new partner, the holiday they had just taken to Europe and their children. She was further shocked to receive the proposition from Dr Wade regarding a ’safe secret relationship’. Dr Wade admitted discussing all issues outlined above but maintained That he had spoken of his wife at the dinner Once again, Dr Wade elected not to cross-examine [Patient A] and challenge her account in this respect It is submitted that Dr Wade’s account of how [Patient A’s] breasts came to be the subject of comment should not be accepted 186. The submissions made on behalf of Dr Wade concerning this Particular are as follows: 62. There is no evidence in relation to Dr Wade commenting on [Patient A’s] appearance. Patient A’s evidence was that Dr Wade 46 commented on her breasts saying great tits’ or ’nice tits’, following the kiss and touch of her inner thigh in the carpas*. The Amended Complaint does not assist in evaluating [Patient A’s] evidence. Dr Wade has always agreed that there was mention of [Patient A’s] breasts that evening. He says that [Patient A] spoke of a reduction in her breasts as she had lost weight Dr Wade said that in conversation over dinner, in the context of speaking of his wife and how she saw her own physical deterioration, womanly breasts were mentioned In our submission, Dr Wade has been frank as to this conversational subject He does not deny outright that there was any mention of breasts, he merely puts the comments, whatever they were, into the context in which he says breasts were mentioned. If it is accepted that at the dinner both parties spoke about matters and relationships personal to them - and the evidence from both Dr Wade and [Patient A] is that both of them discussed matters personal to them, [Patient A], for example, spoke in her evidence about her relationship (arrangement) with a person called John; Dr Wade spoke about his children, and his new relationship as well as about his late wife - it is in our submission more likely than not that the comment, whatever it may have been in which [Patient As] breasts were mentioned occurred within a discussion. We submit it is open to the Committee to infer from Dr Wade’s open and expansive manner that a discussion of personal matters may have taken place in a restaurant, but that a rather more pointed and somewhat vulgar comment such as ’nice tits’ or similar, is unlikely to have been made by him in a cafØ or an even more exposed public place. 63. Dr Wade is criticised by the Complainant for making weak denials. In our submission, Dr Wade has been scrupulous in not saying something did or did not happen unless he is sure or had a good recall of it. That is not to say it is not denied. He has not changed his position on these matters since his first response. He has not made a veiled admission by apologising to [Patient A] for offending her, as the Commission appears to submit (HCCC paragraph 23). 64. The Complainant places some importance on the fact that Dr Wade had not mentioned the conversation previously. We submit that this is a non-sequitur He gave the evidence that he did and it was not inconsistent with his previous responses, merely an elaboration on the comment when asked about it. 65. It is our submission that there is a conflict in the evidence that must be resolved by the Committee, to the requisite level of comfortable satisfaction, if it is to be relied on as a basis for finding unsatisfactory professional conduct [Patient A’s] evidence is that Dr Wade said ’nice tits’ to her in the car park in the context of an incident involving close physical contact Dr Wade’s evidence is that he did not make the comment as alleged but that [Patient A’s] breasts were mentioned by her and possibly also by him, during a conversation at an earlier time, in another place. It is our submission that a careful examination and weighing of the evidence does not support the allegation as contained in the 47 Particular. It must fall and the allegation of unsatisfactory professional conduct must fall with it Finding 187. on balance the Committee is reasonably satisfied that Particular 1.4.3 is proven to the requisite standard. 1.4.4 suggested that the practitioner and Patient A have a personal and/or sexual relationship. 188. Dr Wade denies that this conversation occurred at this time 48 Complainants submissions contend as follows: The 27.1t is unclear whether this particular is admitted, in particular. whether Dr Wade suggested a personal or sexual relationship either at or after the dinner It seemed to be admitted in Dr Wade’s statement However during examination-in-chief, Dr Wade claimed that he had already had that conversation with [Patient A] on the telephone. It was put to Dr Wade under crossexamination that ’at the dinner, you suggested to [Patient A] that she be your mistress’ Dr Wade responded It was not so much a proposition but an explanation.’ Again it is clear from Dr Wades changed stance on this point, his recollection of the dinner is not very clear. [Patient A] gave evidence at the hearing that she was certain the proposition was made again face-to-face because she recalls squaring her shoulders and directly looking at Dr Wade and asking him in a neutral tone, ’and how long do you intend for this to go on for (referring to the secret affair)?’ [Patient As] evidence was not challenged under cross-examination and Dr Wade’s evidence was confused. In any event ) Dr Wade concedes that his suggested proposal was current and discussed at the dinner. It is submitted that this particular ought to be found proven to the requisite standard. 189. The submissions made on behalf of Dr Wade areas follows: 66. Dr Wade agrees that made a suggestion to [Patient A] that they consider a personal relationship, which he described at some point as a ’safe secret relationship’. It is not clear that this description arose prior to its use in the text message sent later. In any event, Dr Wade agrees he made some kind of proposition involving a relationship to [Patient A]. His evidence is that he did this during the telephone conversations he had prior to the dinner. There are no records of the text messages exchanged at that time. He said that at the dinner, the conversation was not concerned with the proposition but rather an explanation of it This is not inconsistent with [Patient As] evidence regarding her reaction. However that is not what the Particular alleges. 67. There is no evidence that a suggestion was made after the dinner, as particularised. The Commission asserts that [Patient Exhibit 1 tab S M AJ is certain the suggestion was made at the dinner However at its highest, the evidence is that [Patient A] was ’pretty sure that it was at the dinner that the ’mistress thing came up’. This is somewhat inconsistent with her evidence regarding her acceptance of the invitation to dinner. Her oral evidence was that, at the time of the phone ca/Is she went to dinner because she cared about Dr Wade, wanted to find out what he was doing, and she did not think he was ready to move in with a new girlfriend if ’he was shopping for a mistress’. Her evidence was that he rang her with a proposition, which she says she thought was odd, and inferred she accepted the invitation to dinner to find out what he proposed - the proposition having already been made. This is what Dr Wade says occurred and the dinner in fact revolved around a generalised talk of relationships, and, in his words some kind of explanation. The proposal, in fact, went nowhere with Dr Wade taking steps to distance himself from it the next day. 68. It is our submission that the evidence does not support this particular. The suggestion referred to occurred prior to the time particularised Dr Wade’s evidence is that it did not happen at this time, and [Patient A] was ambivalent as to when the suggestion was actually made, therefore we do not think the Committee can be comfortably satisfied that this Particular is made out 190. The extent of any discussion at or after the dinner with regard to the suggested relationship is unclear from the evidence. Nevertheless, it is clear from the evidence and Dr Wade’s admission in relation to Particular 1.2.1 that a sexual relationship had been suggested by Dr Wade prior to the dinner. Finding 191. On balance the Committee is not reasonably satisfied that Particular 1.4.4 is proven to the requisite standard. FINDINGS - Section 139B (1) (a) and Section 139B (1) (I) of the National Law49 192. As the Committee has found that all of the Particulars, with the exception of Particular 1.4.4, have been proven to the requisite standard the next issue for 139B Meaning of (unsatisfactory professional conduct" of registered health practitioner generally [NSW] (I) Unsatisfactory professional conduct of a registered health practitioner includes each of the following (a) Conduct significantly below reasonable standard Conduct that demonstrates the knowledge, skill orjudgment possessed, or care exercised, by the practitioner in the practice of the practitioner’s profession is significantly below the standard reasonably expected of a practitioner of an equivalent level of training or experience. (I) Other improper or unethical conduct Any other improper or unethical conduct relating to (he practice or purported practice of the practitioner’s profession 49 determination by the Committee is whether Dr Wade is guilty of unsatisfactory professional conduct 5 within the meaning of section 139B (1) (a) and/or section 139B (1) (I) of the National Law (NSW) as alleged in the Amended Complaint. Section 139B (1) (a) 193. The submissions made on behalf of Dr Wade dealing with section 139B (1) (a) raise three key issues. First, the existence of a doctor-patient relationship, secondly the connection of Dr Wades conduct with the practice of medicine and thirdly the adequacy of the Particulars of the Amended Complaint. 194. The Complainant contends that the evidence strongly supports a finding that there was a current treating relationship in 2007 and 2008. The Complainant submits: 31. Both Dr Wade and [Patient A] gave evidence that there was no formal termination of the doctor-patient relationship. From [Patient A’s] perspective it is clear that she considered Dr Wade to be her treating psychiatrist in both 2007 and 2008. In her statement she said this consideration was based on the fact that ’he knew all my past trauma.’ At the hearing, [ Patient A] stated that irrespective of how many years had lapsed, in 2007 or 2008, she still would not hesitate in returning to see Dr Wade if she needed to. [Patient A] explained that this was particularly common attitude in a smaller city environment. 32. Under cross-examination, Dr Wade admitted that he could not be sure when [ Patient A] may seek to consult with him. In examination-in-chief, Dr Wade admitted that at least prior to the May 2008 appointment, he was on notice that he was [Patient A’s] treating doctor due to the referral from [Patient As] general practitioner, _ -. ’ 33. The question of whether there was a doctor-patient relationship must be assessed on the evidence and it is submitted is a question for the Committee. 34. Dr Klug expressed the view that at all times in 2007 and 2008 there was a doctor-patient relationship subsisting due to the nature of the therapeutic relationship. Dr Kiug gave evidence that the conduct fell significantly below the standard irrespective of whether [Patient A] and Dr Wade were in a doctor-patient relationship, although he did state that this would change the fabric’ of what occurred. Dr KIugs opinion stemmed from the inappropriateness of the personal contact given the therapeutic relationship. 195. The submissions made on behalf of Dr Wade contend: 7. It is not clear to us that the conduct in the Complaint falls to be 5 Pursuant to section 138 of the National Law conduct means any actor ornission 50 considered in s139(B)(’l)(a) as that section assumes a reasonably close connection with the clinical practice of medicine, and the exercise of knowledge, care, skill, and judgment by the practitioner in that pursuit No case was put before the Committee as to the exercise of Dr Wade’s knowledge, care or skill or judgment in the medical treatment of [Patient A] as a basis for a finding of unsatisfactory professional conduct As the Court of Appeal, per Samuels JA observed in Childs V Walton, it is ’desirable for a complainant to particular/se the complaints made by specifying the acts or omissions upon which the complainant relies, and then indicating which of the professional defects in s 27(1)(a)’ each is said to constitute.’ The Complainant has not done this, but relies on a generic proposition that Dr Wade’s conduct is in breach of s1398(1)(a) by virtue of the continued existence of the doctorpatient relationship, relying on Childs v Walton. It is our submission that if the relationship is not current, therefore there is no direct link in temporal terms with the practice of medicine, it is essential that the Complaint identify the conduct in terms which are. . capable of satisfying the prescription [of medical practice]. ’The conduct must be such as to demonstrate the lack of a quality (eg adequate knowledge) necessary in the practice of medicine’. It is our submission that the Commission has failed to establish these fundamental matter [sic]: the existence of a doctor-patient i.e. treating relationship, or the specific deficiencies demonstrated in conduct that is sufficiently connected to the practise of medicine to be relevant to s1398(1)(a). 8. [Patient A] was not a current patient at the relevant times, and there is no allegation that improper conduct occurred during consultations, or whilst the complainant was under continuing treatment. We submit that the Committee would be asking itself the wrong questions when considering whether the conduct alleged, breached s139(B)(1)(a). 196. On balance the Committee considers that the doctor-patient relationship pertained during the relevant period in October 2008. In reaching this conclusion the Committee has had regard, amongst other matters, to the logic of Dr KIug’s characterisation of the relationship between Dr Wade and Patient A and the absence of any termination of the doctor-patient relationship. The Committee has also had regard to the intense nature of Patient A’s treatment in the period from 1999 - 2003 and the complexity of Patient As ongoing psychological presentation. The Committee also notes Patient As evidence that she continued to consider that Or Wade was her psychiatrist. 197. The Complainant contends that even if the doctor-patient relationshl? had ? been terminated the conduct still occurred "in the practice of medicine" Complainant refers the judgment of Samuels JA in the NSW Court of Appeal in Childs v Walton NSWCA (unreported 13 November 1990). When SI 52 The Medical Practitioners Act 1938 Section 139B (1) (a) "...in the practice of the practitioner’s profession’ 51 considering the phrase in the context of the Samuels JA concluded: Medical Practice Act 1938 The phrase in the practice of medicine’ does not have a temporal meaning, but rather a qualitative or descriptive character. It does not circumscribe the period during which the conduct impugned must occur if it is to be capable of satisfying the prescription.. Hence the act or omission constituting the conduct.. need not occur while the relationship of doctor and patient exists between a complainant and the practitioner... The only requirement is that it must demonstrate one of the specified deficits. conduct by a practitioner that demonstrates his or her lack of one or more qualities indispensable to the practice of medicine or, in the case of lack of adequate experience, to the particular procedure undertaken-" 198. For the purposes of section 139B (1) (a) the Committee considers that the conduct occurred in the practice of medicine. 199. The submissions made on behalf of Dr Wade concerning section 139B (1) (a) challenge the adequacy of the Particulars of the Amended Complaint due to a lack of specificity. The submissions contend: 72.No case has been put which identifies with any specificity the deficit in knowledge, care, skill or judgment is relied upon by the Commission to the Complaint of a breach of s39(B)(1)(a). The Commission relies on Dr KIugs evidence that because in his view a doctor/patient relationship existed in 2007 and 2008, the conduct breached the section (presumably in terms of a failing in judgment). In our submission it is not that simple. In our submission, Dr kIug was asked to apply the wrong analysis to the facts of the complaint, and in focusing his evidence on only one aspect, that is (a), the Committee is left with an ambivalent conclusion by the expert peer in relation to (a) and no guidance as to whether or not the conduct in question breached s39(1) [sic] In these circumstances we do not consider that the Committee could comfortably reach a decision that unsatisfactory professional conduct has been proved. 200. It is contended on behalf of Dr Wade that the Complainant has relied on a generic proposition and failed to particularise the professional defects by reference to knowledge or skill or judgment possessed or care exercised by Dr Wade. The Complainant’s submissions do not address this issue. Although there is a need for clarity with regard to Particulars the National Law provides that the Committee may conduct proceedings on the inquiry as it thinks fit. At page 9 Priestly JA and Meagher JA agreeing Section 171A (1) and Schedule 5D of the National Law. The observations of Freeman DCJ i n/n Re A Medical Pi’actitioner and the Medical Practice Act Mare relevant in this regard: 16. ... The PSC is not and should not be cast as a cowl of strict pleading. Under s176 and Schedule 2 of the Medical Practice Act it is empowered to conduct its proceedings as it sees fit, not being bound by the rules of law governing the 52 The Committee considers that Dr Wade had not been denied procedural fairness by the general nature of the Particulars. 201. For the purposes of section 139B (1) (a) of the National Law it is necessary for the Committee to have regard to the relevant "equivalent level of training and experience in order to determine the standard expected of a practitioner. The Committee considers that Dr Wades conduct should be assessed in accordance with the standards expected of an experienced consultant psychiatrist. 202. The Complainant contends that Dr Wade’s conduct fell below the relevant standard and submits as follows: 28. The Commission expert, Dr klug, found Dr Wade’s conduct fell significantly below the standard reasonably expected of a practitioner of an equivalent level of training or experience at the time of his conduct. Dr Kiug isolated two key reasons as to why Dr Wades behaviour was inappropriate. The first was the initiation of the contact: ’[t]he main issue was his response to [Patient A] once he had identified her as a former patient.’ Dr KIug opines that the personal correspondence between Dr Wade and [Patient A] via the internet and by mobile telephone was inappropriate. The second reason is the nature of the therapeutic relationship, that is, the period of regular treatment and the reason for the treating relationship. Dr Klug makes specific note that Dr Wade was aware that [Patient A) suffered chronic post traumatic stress disorder, chronic depression, mood instability indicating a possible diagnosis of bipolar If disorder, borderline personality disorder, somatisation and was a victim of childhood sexual assault.’ 29.Dr KIug was not strongly critical of Dr Wade’s conduct. At the hearing Or K/ug explained that Dr Wade’s conduct did not invite his strong criticism partially because the relationship was not pursued by Dr Wade and partially because Or Wade did not appear to be predatory in his pursuit of [Patient A]. It is submitted that it is the aggregation of the respondent’s conduct starting from the RSVP interaction and ending with the October 2008 dinner should persuade the Committee that his conduct did fall significantly below the acceptable level and was not just a single isolated act of poor judgment 30. The Commission notes Dr Kiug’s opinion as provided at the hearing, that is, that Dr Wade’s conduct still fell significantly below the relevant standard even if there was no kiss, no touching of her thigh and no comment on her breasts. Dr KIug explained that in his opinion, it was the initiation of the personal admission of evidence. It is constituted deliberately as an expert body dealing in a practical manner with problems faced in the practice of medicThe. That does not mean, of course, that it is entitled to deal unfairly with a practitioner and deny the rules of natural justice or procedural fairness. A practitioner is entitled to know the allegation made against him or her’ 53 contact that led to the conduct falling significantly below the relevant standard, irrespective of any subsequent inappropriate physical contact or comments. [References omitted] 203. The submissions made on behalf of Dr Wade contend that there was no evidence that Patient A felt imposed upon by the invitation to meet with Dr Wade and she did not seem to take affront at the possibility of a personal relationship such as a mistress. The Complainants submissions in reply submit that "even if [Patient A] had expressed interest in the relationship or even made the first offer, that in no way diminishes the inappropriateness of Dr Wade’s conduct This is because there is an inherent inequality in a doctorpatient relationship and accordingly it is the doctor’s professional and ethical duty to avoid any personal relationships". The Complainant refers to the decision of HCCC v Dr Vipal Kumar Mehta (2002) NSWMT55 in support of this proposition: "It is of course not the point that he perceived her to be a willing party. Mutuality’ in the relationship can never truly exist. The position of power occupied by a treating doctor is such that a relationship with a patient can never truly be ’equal’- The doctor and not the patient has the ethical and professional obligation to avoid such relationships. As Denning LJ observed in De Gregory v General Medical Council [1961] AC 957 at 966 ’even if she sets her cap at him, he must in no way respond or encourage her.’ 204. Relevantly in his oral evidence Dr Wade described his conduct as ’horrific" and he referred to his "wanton disregard for Patient A’s vulnerability". In contradistinction to Dr KIug the Committee considers Dr Wade’s departure from the expected standard warrants strong criticism. Having assessed the evidence the Committee considers that Dr Wade’s conduct fell significantly below the standard expected of a senior consultant psychiatrist. Accordingly the Committee finds that the provisions of section 139B (1) (a) of the National Law are engaged and Dr Wade is guilty of unsatisfactory professional conduct. Section 139B (1) (I) 205. The Committee notes that the Amended Complaint is framed in terms of section 139B (1) (a) "and/or" section 139B (1) (I) which indicates that the Complainant alleges that either or both statutory provisions apply. However, the Complainant’s submissions in reply purport to clarify the Complainant’s position by indicating that a finding should be made under section 139B (1) (I) in the alternative, in the event that a finding is not made pursuant to section 139B (1) (a). 56 As the Committee has found that Dr Wade is guilty of page 13 The Complainant’s submissions in reply at paragraph 3: a/n response to the respondents submissions on unethical or improper conduct at [9][16], the Commission clarifies its position that in the event that a finding is made that the conduct was not significantly below the relevant standard or not in the practice of medicine under section 1398(1)(a), then alternatively, a finding should be made that the conduct is improper or unethical relating to the practice of medicine under section 1398(1)(1) (see [38] of May submissions). 54 unsatisfactory professional conduct in terms of section 139B (1) (a) it is not necessary for the Committee to address section 139B (1) (I). Summary 206. In summary the Committee is reasonably satisfied that Dr Wade is guilty of unsatisfactory professional conduct in terms of section 139B (1) (a) of the National Law. The Appropriate Orders - Submissions 207. The protective orders proposed by the Complainant traverse 3 issues. FhsL, submissions that Dr Wade be reprimanded. 57 Secondly, a recommendation that Dr Wade should be required to attend the Medical Ethics Course conducted by Monash University. 58 Thirdly, a submission that Dr Wade "enter into a mentoring relationship with a more senior psychiatrist for a period of time. ’ 208. The Complainant submits that Dr Wade’s conduct was of a serious nature given the following factors: (a) [Patient A’s] particular difficulty with trust in men; (14 the range and severity problems/conditions; of [Patient A’s] psychiatric (c) the intensity and duration of the treating relationship, i.e. five years on a regular basis (1999-2003); (d) the initiation and continuation of personal contact over a period of months which started with emails, texts and phone calls and culminated in a dinner; (e) the active steps taken towards entering into a sexual affair with [Patient A] including initiating the dinner, participation in various personal communications via email and telephone, physically touching [Patient A] inappropriately and asking [Patient A] on more than one occasion to be his mistress. (t) unconvincing explanation for his conduct in October 2008; and (g) Dr Wades less than fulsome admissions. 209. The submissions made on behalf of Dr Wade with respect to Orders are as follows: 2. If the Committee does conclude that the Complainant has established that Dr Wade’s conduct constituted unsatisfactory professional conduct, we submit there is very limited material to suggest protective orders beyond a caution pursuant to s146B (1) (a) is in Complainants submissions paragraph 65 -66 ibid at paragraph 68. ibid at paragraph 69 55 any way indicated 3. There is no evidence that would support additional orders for the protection and safety of the public. A caution is sufficient notice to the public and the profession for the purposes of maintaining appropriate standards and its good name. 4. The Complainant submits that there are aggravating factors that support its application for protective orders. We submit there are no aggravating factors because Dr Wade has shown he is unlikely to conduct himself this way again, and there is no evidence to sugg he is practising in a manner that is unsafe or unsatisfactory. 5. He concedes that a psychiatrist has a duty to his patient to always act with the highest level of propriety and circumspection. Given the exposure to a patient’s mental and emotional history, a former patient must also be treated with care, and a proper distance maintained for the sake of the patient’s trust in the doctor and in the profession generally. The Committee is able to consider Dr Wade’s ability to recognise and appreciate his patient’s fights and potential vulnerabilities, and the extent to which he took advantage of [Patient A’s] vulnerability and dependence, or exploited these for his own purposes and whether, given the effluxion of time, his own capacity for insight and reflection, and the circumstances prevailing at the time, the Committee should have any concerns that such conduct would be repeated. Only if there is such a risk, in our submission, would the Committee be justified in imposing conditions. Prior to October, there is no evidence of any exploitation on the part of Dr Wade. On the evidence, what exploitation occurred was limited to [Patient A’s] role as a dinner companion and potential sympathiser. Dr Wade, thereafter, made attempts to stop any further contact and to disabuse [Patient A] of any idea that he intended to pursue a relationship. He thought [Patient A] had accepted his apology and was not unduly upset by this. 7. Some support for Dr Wade’s perception that his conduct had not adversely affected [Patient A] can be found in the extended period of years before any complaint was forthcoming, during which period it is understandable that, after anguishing about his conduct, Dr Wade put it out of his mind as over, both for [Patient A] as well as for himself. 8. Nevertheless, upon becoming aware of it, Dr Wade accepted that [Patient A] did feel she was exploited by his actions, and that he had erred in not considering this property. He accepts that he did not recognise, and he should have, that she was not as capable as she thought Using the clarity of mind that he should have employed at the time, Dr Wade realised that what he had done was potentially damaging. He confided to members of his peer group and received support from them. ITA 9. Dr Wade was without doubt, in our submission, still suffering from the significant issues that surrounded the death of his wife, as well as other deeply affecting personal and family problems, such as the death of his mother and family discord, responsibility for his children, the ability to continue to work and earn a living and some issues with staff and finances. These external factors were very significant forces pertaining at the time that impacted on his decision making. As Dr Klug said in re-establishing his life, and another relationship at this time, Dr Wade blurred his professional and personal relationship with [Patient A] for reasons that were unclear even to Dr Wade but which related to those stresses. 10. We submit that the Committee can accept Dr Chenoweth’s evidence that Dr Wade suffered considerably for a great length of time, over the tragic and shocking illness and demise of Mrs Wade in 2006. The effect of this on his ability to rationalize his intentions towards [Patient A] is not something that can be measured simply by looking at the time that had elapsed since the death of Mrs Wade, and reach a conclusion, in the manner of Dr kIug, that grief should not excuse his conduct, two and a half years on. This is the position taken by the Complainant in its written submissions and is not supported on all the evidence particularly that of Dr Wade and Dr Chenoweth. II, The Commission’s written submission (paragraph 64) invite the Committee to discount the effect of "issues surrounding his wife’s passing" on his conduct. The submission is that Dr Wade denies the real reason for his conduct i.e. that he saw an opportunity with [Patient A] and decided to pursue it This misunderstands Dr Wade’s evidence. He accepts that he decided to pursue an opportunity (he does not accept he had expressed previous interest as alleged). The issue for Dr Wade and the Committee is trying to understand the context in which this decision making took place. 12. We submit that Dr Wade receives considerable support and understanding from his peers and that this is sufficient to assist him in maintaining appropriate boundaries, as he has done prior to and since this particular episode. We submit that Dr Chenoweth and Dr KIug both agreed that the length of time that has elapsed, the lack of other boundary issues, and the practitioner’s own comprehension of appropriate boundaries lessened the risk of such conduct occurring again In our submission, the Committee would be satisfied on the basis of the reports from Drs Chenoweth and Dr Corrigan, and the mild criticism of Dr Kiug that Dr Wade is not in need of further admonition, or further monitoring by the Medical Council as a means of ensuring compliance with the high expectations of his profession. 13. We submit no further protective orders are necessary’. Factors that the Committee ought reasonably take into account in arriving at that view include the following. 57 14. Dr Wade, whilst opposing a legal characterisation of his behaviour as unsatisfactory professional conduct, has nonetheless frankly agreed that his behaviour, in paraphrase, was wrong, regrettable and likely to have caused anguish to [Patient A]. 15. Dr Wade demonstrated significant remorse and insight in terms of his evidence and his conduct before the Committee. 16. Dr Kiug found the conduct did not invite his strong criticism. 17. Dr KIug considered Dr Wade did not have a predatory motivation. 18. Dr KIug agreed that the circumstances of the conduct, peer group support and self reflection and the fact of the isolated nature of the offending conduct ameloriated [sic] risk. 19. Doctors Chenoweth and Corrigan provided references that were consistent with Dr Wade’s showing genuine insight, and receiving support which almost entirely diminished risk 20. Dr Wade receives ongoing professional support through his peer group. 21. The time period before and since the formal complaint without any hint of similar behaviour strongly indicates no ongoing need for protective orders. 22. The Committee can safely move on the basis that the Complaint and the proceedings have had a significantly salutary effect on Dr Wade. The Appropriate Orders - Conclusions 210. 60 The Disciplinary Powers of Professional Standards Committees are set out in Part 8 Division 3 Subdivision 3 of the National Law (NSW). The Committee 360 The Committee may exercise any powers conferred on it by Subdivision has been mindful that the jurisdiction of the Committee in disciplinary matters of the present nature involves protection of the public and the maintenance of the highest possible ethical and clinical standards of the medical profession. Protection of the public includes consideration of the likelihood of the relevant Section 146 B (1) provides a Committee may do one or more of the following: (a) caution or reprimand the practitioner; (b) direct that the conditions, relating 10 the practitioners practising of the practitioner’s profession, it considers appropriate be imposed on the practitioner’s registration; (c) order that the practitioner seek and undergo medical or psychiatric treatment or counselling; (d) order that the practitioner complete an educational course specified by the Committee; (e) order that the practitioner report on the practitioner’s practice at the times, in the way and to the persons specified by the committee; (I) order that the practitioner seek and take advice, in relation to the management of the practitioners practice, from the persons specified by the Committee. Section 146 C provides that the Committee has the power to fine in certain cases 58 conduct being repeated and the necessity of deterring both the practitioner and others from failing to adhere to the standards expected of them . 61 211. The Committee has found that Dr Wade is guilty of unsatisfactory professional conduct. Dr Wades role as Patient As treating psychiatrist placed him in a singular position of trust in relation to a particularly vulnerable and fragile patient with a complex psychiatric history. Whilst Dr Wades personal circumstances may have been distressing it is unfortunate that notwithstanding his training and experience Dr Wade did not have sufficient insight to seek appropriate professional support in the period following his bereavement. 212. The rationale for Dr Wades conduct remains problematic. The evidence indicates that he sought no advice about his conduct until after he was contacted by the HCCC in October 2010. Dr Wade’s decision not to pursue any relationship with Patient A following the dinner on 12 October 2008 indicates he eventually did achieve some perspective regarding the inappropriate nature of his conduct. In addition Dr Wade expressed remorse for his conduct. Nonetheless Or Wade’s unsatisfactory professional conduct warrants strong reprobation. To that end the Committee considers that Dr Wade should be reprimanded for his unsatisfactory professional conduct. 213. There was no evidence before the Inquiry suggesting similar conduct on Dr Wade’s part in the past or that Dr Wade would be likely to engage in such conduct in the future. Dr KIug opined that Dr Wade’s involvement with a supportive peer group would be relevant to the protective aspect of the Committee’s jurisdiction. Both Dr Wade and Dr Chenoweth have attached considerable significance to the role of Dr Wade’s peer group in assisting Dr Wade to maintain appropriate professional boundaries in keeping with the high standards of the medical profession. On balance the Committee considers that no further protective orders are necessary. ORDERS 214. The Committee exercises its powers in accordance with section 146B (1) (a) of the National Law (NSW) to reprimand Dr Wade. PUBLICATION OF DECISION 215. Pursuant to section 171E (1)ofthe National Law the Committee provides copy of this written statement of decision to the Dr William Douglas Wade, the Health Care Complaints Commission and the Medical Council of New South Wales. 216. Pursuant to section 171E (3) of the National Law the Committee provides a copy of this written statement of decision to Patient A, the Medical Board of Australia, Dr Peter KIug and Ms Francesca Davis, Senior Solicitor from Avant Law Pty Ltd. Health Care Complaints Commission v Litchfield (1997)41 NSWLR 630 at 637, See also Prakash v Health Care Complaints Commission [NSWCA] 153 at paragraph 91 Basten JA ... There is also an element of deterrence or, to put it more positively, encouragement to other practitioners to recognise the importance of complying with professional standards and the risks of failing to do so...’ 61 59 NON-PUBLICATION DIRECTION 217. Clause 7 of Schedule 5D of the National Law (NSW) provides that the person presiding at proceedings before the Committee may make directions in relation to the release of information if that person thinks it appropriate in the particular circumstances of the case (and whether or not on the request of the complainant, the registered practitioner or any other person) 218. The Chairman considers that in the circumstances of this case there are no reasons relating to the public interest which warrant the publication of Patient As name or any evidence which might lead to the identification of Patient A. 219. The interim non-publication direction issued on 8 May 2012 is varied and the following direction applies from the date of this Decision: 1. The following matters are not to be published by any person: a. The name and address of Patient A; b. Any evidence relating to the subject matter of the complaint which may identify Patient A. 2. This direction does not operate to exclude any provision of the National Law (NSW) and does not preclude the Medical Council of New South Wales from undertaking its statutory functions. 3. Publication may include communicating either in writing or verbally to any person. APPEAL and REVIEW 220. An appeal to the Medical Tribunal against this Decision is available under section 158 of the National Law or section 158A of the National Law if the appeal is with respect to a point of law. Such an appeal is to be made within 28 days of handing down of the decision (or such longer period as the Executive Officer of the Medical Council may allow in any particular case). Mr Robed Kelly Chairperson 19 September 2012 [1
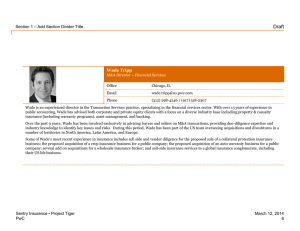
![Arrival of Wade Keiffer[1]](http://s3.studylib.net/store/data/008164778_1-51788b3e4d580af943e609fb94f63938-300x300.png)