23. Comprehensive: Nursing Home, back pain
advertisement
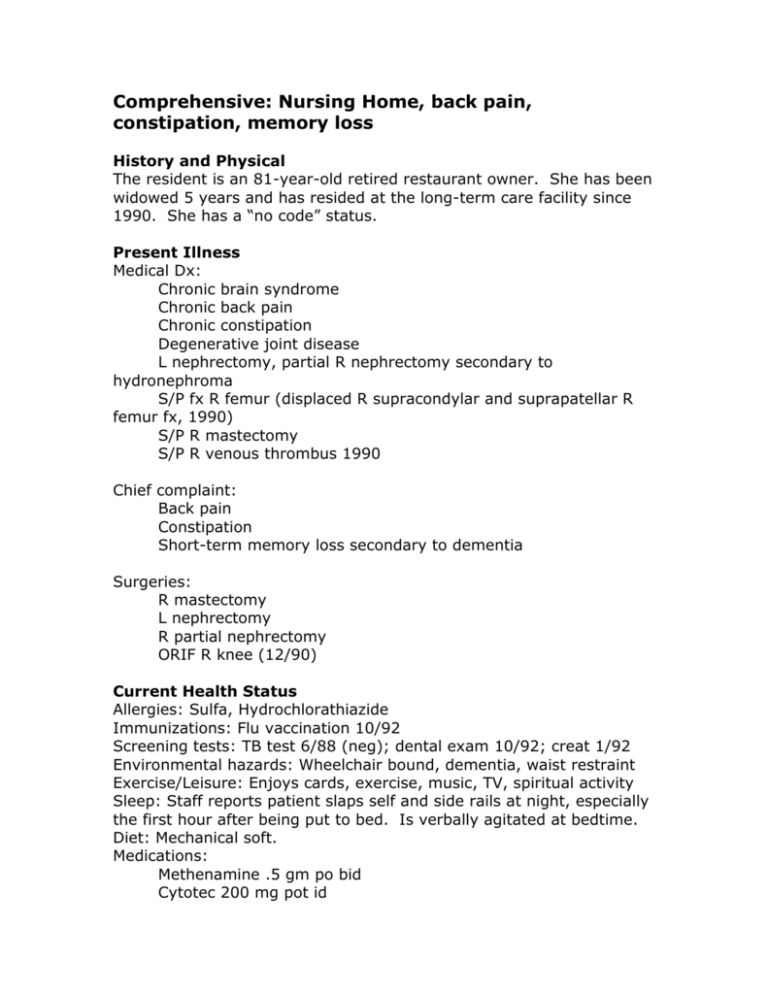
Comprehensive: Nursing Home, back pain, constipation, memory loss History and Physical The resident is an 81-year-old retired restaurant owner. She has been widowed 5 years and has resided at the long-term care facility since 1990. She has a “no code” status. Present Illness Medical Dx: Chronic brain syndrome Chronic back pain Chronic constipation Degenerative joint disease L nephrectomy, partial R nephrectomy secondary to hydronephroma S/P fx R femur (displaced R supracondylar and suprapatellar R femur fx, 1990) S/P R mastectomy S/P R venous thrombus 1990 Chief complaint: Back pain Constipation Short-term memory loss secondary to dementia Surgeries: R mastectomy L nephrectomy R partial nephrectomy ORIF R knee (12/90) Current Health Status Allergies: Sulfa, Hydrochlorathiazide Immunizations: Flu vaccination 10/92 Screening tests: TB test 6/88 (neg); dental exam 10/92; creat 1/92 Environmental hazards: Wheelchair bound, dementia, waist restraint Exercise/Leisure: Enjoys cards, exercise, music, TV, spiritual activity Sleep: Staff reports patient slaps self and side rails at night, especially the first hour after being put to bed. Is verbally agitated at bedtime. Diet: Mechanical soft. Medications: Methenamine .5 gm po bid Cytotec 200 mg pot id Feldene 20 mg po qd DSS w/CAS 1 cap po bid APAP 2 tab qid PRN: bisacoydal supp qd prn Alcohol and Tobacco Use: Current and past use unable to be determined at this time. Family History Had 3 children, one child died in infancy. Son lives in XXX. Daughter lives in XXX. Unable to determine medical family history, as patient believes parents are still alive. Psychosocial History Has daily contact with relatives or group activities. Son and granddaughter live close by. DJ and her husband owned and operated a restaurant and tavern in town. DJ’s son currently runs the tavern. At the time of this examination, DJ believes her husband and parents are still living and that she will be going home. She is active in the facility’s activities. Developmentally, she is age-appropriate with the exception of her confusion. Review of Systems Skin: Denies rashes, nodules or open sores. Head: Denies headache, head injuries. Eyes: Denies vision loss, glaucoma, diplopia. Wears glasses. Ears: Denies hearing loss, vertigo, tinnitus. Nose: Denies sneezing, nosebleed, hay fever. Mouth: Denies open sores, bleeding gums. Wears upper and lower dentures. Neck: Denies hoarseness, goiter, dysphagia. Lungs: Denies wheezing, productive cough, hemoptysis, pneumonia, asthma. Bronchitis documented 1990. Heart: Complains of shortness of breath. Denies orthopnea, chest pain, edema, heart attack, palpitations, hypertension. Breasts: Denies lumps or discharge. States both breasts are present (has had R mastectomy). GI: Denies anorexia, vomiting, diarrhea, bleeding, nausea, constipation, pain, jaundice (patient record indicates frequent constipation). GU: Denies frequency, nocturia, hematuria, polyuria, dysuria, incontinence, infections or hernias. GYN: Gravida 3, para 3. Postmenopausal. Peripheral Vascular: States varicose veins. Denies leg cramps, phlebitis. MS: Denies pain, joint swelling, arthritis. States occasional back pain. Neurological: Denies seizures, paralysis, numbness, tingling. Blood: Denies transfusion history. Endocrine: States thyroid difficulty, denies diabetes. Physical Exam General: Wt. 146 lb (6/93). Ht: 5’3”. BP 108/80. Requires total assist in transfer to and from bed. Does not bear weight. At time of exam, pt incontinent of urine. Skin: Hair white, thin. Skin color pink, no rashes or lesions. Eyes: Reads large print easily, able to read some small print. Sl ptsosis L eye. Unable to elicit EOM. PERRLA. Opthalmic exam WNL. Ears: R ear partially blocked with cerumen, L3/4 occluded. R TM WNL. Hears whispered tones bilaterally. Nose: Septum midline, no sinus tenderness. Mouth: Lips moist, gums pink, non-edematous, tongue midline, pharynx WNL. Upper and lower dentures intact. Neck: Thyroid palpable, non-enlarged, trachea midline, no nodes palpable. Lungs: Respirations non-labored, lungs clear, good aeration, chest shape normal. CV: Sl. Systolic murmur auscultated, HS regular, no JVD, no bruits auscultated. Ankle edema present bilaterally, L > R. Feet cool to touch. Unable to palpate pedal or posterior tibial pulses. Breasts: Left breast full, non-tender, soft, no masses palpated. R mastectomy incision. Abdomen: Large, soft, non-tender. Upper left incision extending to back, 2” incision below umbilicus, midline pubic incision. Yellow/brown skin tag present LLQ. Genitalia: Labia and vulva normal for age. Pelvic exam deferred at patient request. Urinary incontinence. Rectum: Anal area reddened, no open areas. Rectal exam: Smooth rectal wall, no masses. MS: No deformities. Finger joints slightly enlarged but no deformity. Unable to bear weight. Knees flexed during transfers. Unable to adduct L leg. Able to raise L leg 90 degrees. R leg normal ROM. Resistance to plantar flexion bilaterally. Neuro: CN II-XII intact. Negative Romberg. Upper arm strength strong and equal bilaterally. Lower extremities previously described. Mental: Scored 11 of 30 on Mini-Mental exam. Uses waist restraint while in wheelchair. Asks same question or made same comment frequently during examination. Short-term and long-term memory impaired.