Clinical Science 3
advertisement
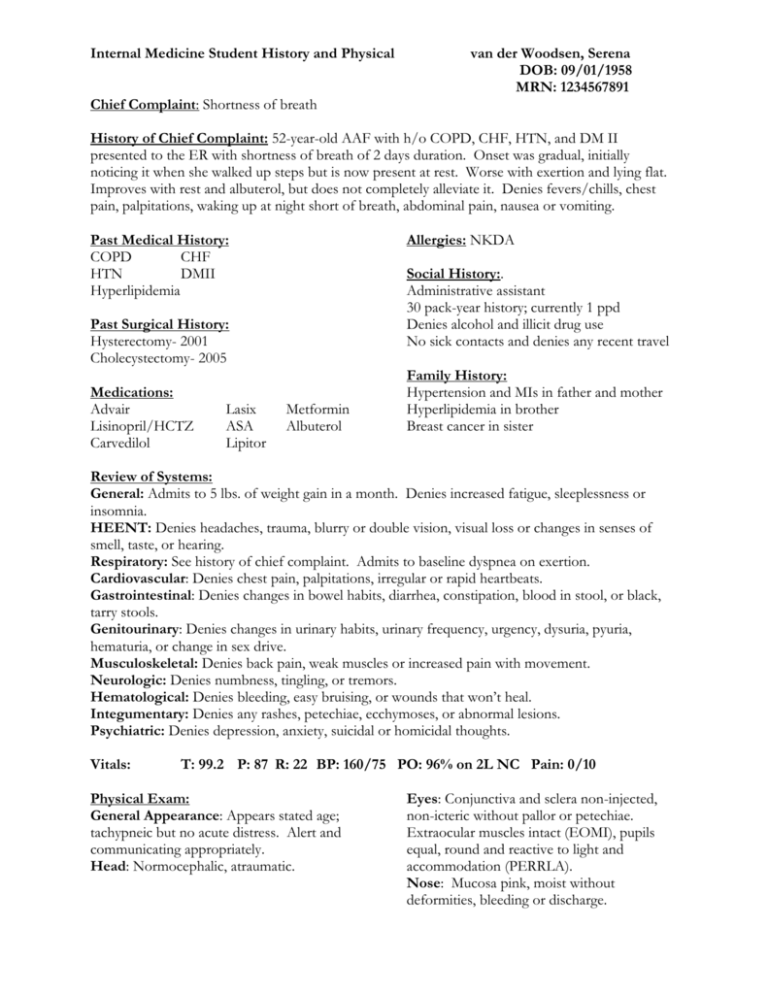
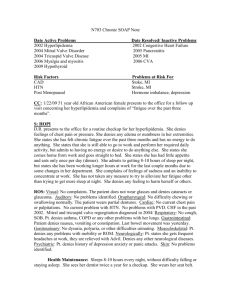
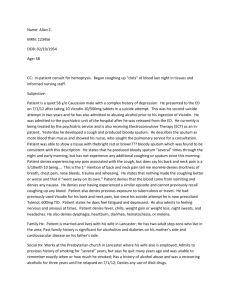
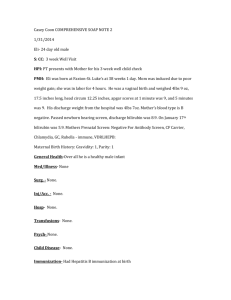
Internal Medicine Student History and Physical van der Woodsen, Serena DOB: 09/01/1958 MRN: 1234567891 Chief Complaint: Shortness of breath History of Chief Complaint: 52-year-old AAF with h/o COPD, CHF, HTN, and DM II presented to the ER with shortness of breath of 2 days duration. Onset was gradual, initially noticing it when she walked up steps but is now present at rest. Worse with exertion and lying flat. Improves with rest and albuterol, but does not completely alleviate it. Denies fevers/chills, chest pain, palpitations, waking up at night short of breath, abdominal pain, nausea or vomiting. Past Medical History: COPD CHF HTN DMII Hyperlipidemia Allergies: NKDA Social History:. Administrative assistant 30 pack-year history; currently 1 ppd Denies alcohol and illicit drug use No sick contacts and denies any recent travel Past Surgical History: Hysterectomy- 2001 Cholecystectomy- 2005 Medications: Advair Lisinopril/HCTZ Carvedilol Lasix ASA Lipitor Metformin Albuterol Family History: Hypertension and MIs in father and mother Hyperlipidemia in brother Breast cancer in sister Review of Systems: General: Admits to 5 lbs. of weight gain in a month. Denies increased fatigue, sleeplessness or insomnia. HEENT: Denies headaches, trauma, blurry or double vision, visual loss or changes in senses of smell, taste, or hearing. Respiratory: See history of chief complaint. Admits to baseline dyspnea on exertion. Cardiovascular: Denies chest pain, palpitations, irregular or rapid heartbeats. Gastrointestinal: Denies changes in bowel habits, diarrhea, constipation, blood in stool, or black, tarry stools. Genitourinary: Denies changes in urinary habits, urinary frequency, urgency, dysuria, pyuria, hematuria, or change in sex drive. Musculoskeletal: Denies back pain, weak muscles or increased pain with movement. Neurologic: Denies numbness, tingling, or tremors. Hematological: Denies bleeding, easy bruising, or wounds that won’t heal. Integumentary: Denies any rashes, petechiae, ecchymoses, or abnormal lesions. Psychiatric: Denies depression, anxiety, suicidal or homicidal thoughts. Vitals: T: 99.2 P: 87 R: 22 BP: 160/75 PO: 96% on 2L NC Pain: 0/10 Physical Exam: General Appearance: Appears stated age; tachypneic but no acute distress. Alert and communicating appropriately. Head: Normocephalic, atraumatic. Eyes: Conjunctiva and sclera non-injected, non-icteric without pallor or petechiae. Extraocular muscles intact (EOMI), pupils equal, round and reactive to light and accommodation (PERRLA). Nose: Mucosa pink, moist without deformities, bleeding or discharge. Throat/Mouth: Lips pink, tongue pink without atrophy, fissures or deviation from midline on extension. Buccal mucosa, palate, and uvula pink and moist without lesion or masses. Edentulous. Neck: Supple without nuchal rigidity. Jugular venous pressure approximately 8 cm H20. Carotid pulses are equal bilaterally without bruits. Thyroid not enlarged, moves with swallowing. Trachea midline, moves freely with passive motion. Lymph nodes: No enlargement or tenderness of cervical, axillary, or inguinal lymph nodes. Lungs: Fine crackles in bases bilaterally, right worse than left. End-expiratory wheezes in upper lobes, but breath sounds present in all lung fields. Heart: Regular rate and rhythm (RRR) with S1 equal to S2. II/VI systolic ejection murmur present at right sternal border in 2nd intercostals space that radiates into carotids. No splitting, S3, S4. PMI laterally displaced. Abdomen: Abdomen soft, nontender, nondistended. Resonant to percussion, bowel sounds present in all four quadrants. Genitourinary: Perianal area intact without lesion, rashes, inflammation, scars. Anal Labs in ER: 12.9 137 surface intact without lesion, fissure, fistula, hemorrhoids. Good sphincter tone. Rectal walls smooth without nodules, masses, tenderness. Stool dark brown without visible blood. Guaiac negative. Extremities: Warm, pink, non-tender with peripheral pulses: radial, posterior tibial, and dorsalis pedis +2/4 equal bilaterally. No edema, varicosities, lesions, deformities. Capillary refill 2-3 seconds bilaterally. Muscle mass symmetrical bilaterally with full active, passive range of motion (ROM). Neurological: Oriented to person, place and time. Immediate, recent and remote memory intact; language appropriate and speech intelligible. Handgrip strength, internal and external rotation, symmetrical, strong. Reflexes are +2/4 and equal bilaterally for patellar, Achilles, biceps, triceps. Babinski reflex is down-going bilaterally. Structural Exam: Shoulders, iliac crest height are level. No apparent abnormality of kyphotic or lordotic curves. No scoliosis. Paravertebral musculature is symmetrical and non-tender with palpation. Skin: Pink, warm, dry with good texture and turgor. No rashes or lesions. 105 20 376 425 10.2 4.2 24 1.1 37.1 Chest x-ray (CXR): Stable cardiomegaly and pulmonary vascular congestion when compared to previous film from 1/10/2011. No focal infiltrates or acute process identified. Assessment and Plan: Your admission orders! Assignment: Write admission orders in the format presented in class (ADCA VAN DIMLS) Orders can be written on progress note paper or typed Focus on being complete, thorough, and following the proper format; don’t worry if you aren’t sure what the exact diagnosis or work up should be Don’t forget to put the date and time (military preferred) in the upper left corner, and sign and print your name at the bottom of your orders Turn in to G 227 by 5 pm 24 hours after your Documentation session Contact the fellows (fellowsd@oucom.ohiou.edu or stop by G333) with any questions!