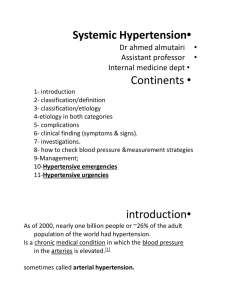
CARDIOLOGY Pulse pressure- difference btw systolc + diastolic
advertisement
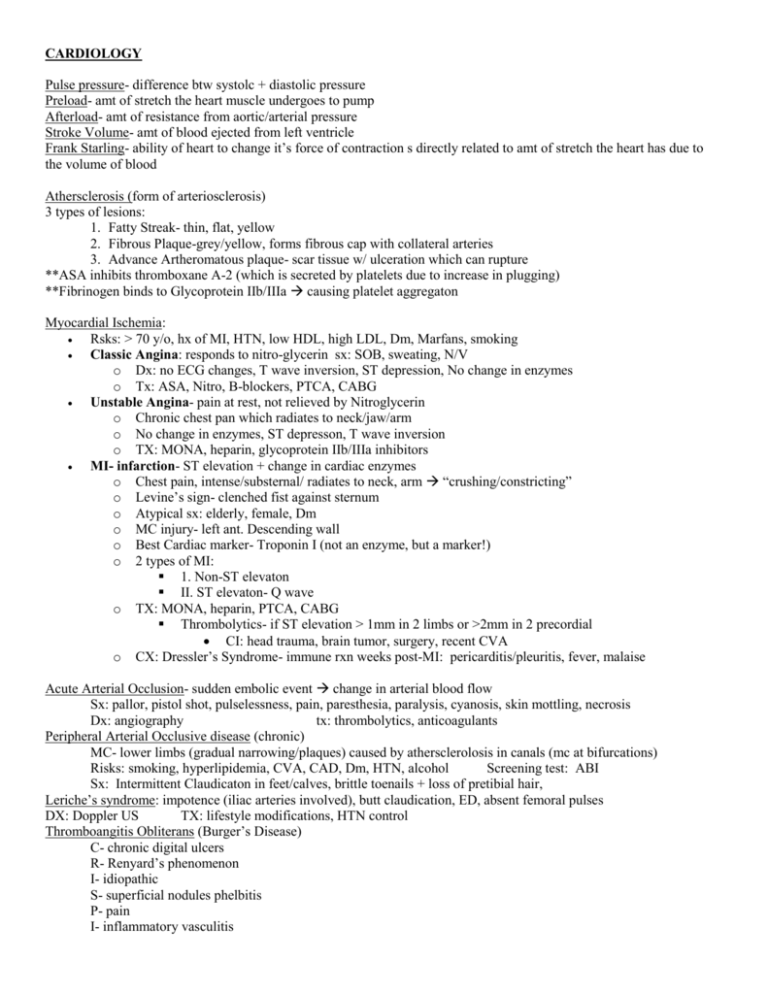
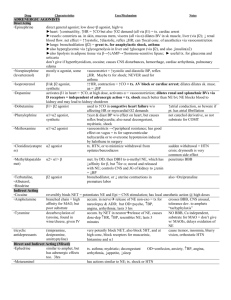
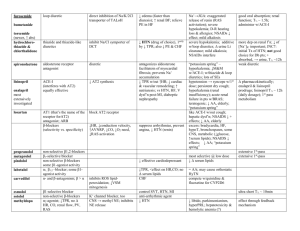
CARDIOLOGY Pulse pressure- difference btw systolc + diastolic pressure Preload- amt of stretch the heart muscle undergoes to pump Afterload- amt of resistance from aortic/arterial pressure Stroke Volume- amt of blood ejected from left ventricle Frank Starling- ability of heart to change it’s force of contraction s directly related to amt of stretch the heart has due to the volume of blood Athersclerosis (form of arteriosclerosis) 3 types of lesions: 1. Fatty Streak- thin, flat, yellow 2. Fibrous Plaque-grey/yellow, forms fibrous cap with collateral arteries 3. Advance Artheromatous plaque- scar tissue w/ ulceration which can rupture **ASA inhibits thromboxane A-2 (which is secreted by platelets due to increase in plugging) **Fibrinogen binds to Glycoprotein IIb/IIIa causing platelet aggregaton Myocardial Ischemia: Rsks: > 70 y/o, hx of MI, HTN, low HDL, high LDL, Dm, Marfans, smoking Classic Angina: responds to nitro-glycerin sx: SOB, sweating, N/V o Dx: no ECG changes, T wave inversion, ST depression, No change in enzymes o Tx: ASA, Nitro, B-blockers, PTCA, CABG Unstable Angina- pain at rest, not relieved by Nitroglycerin o Chronic chest pan which radiates to neck/jaw/arm o No change in enzymes, ST depresson, T wave inversion o TX: MONA, heparin, glycoprotein IIb/IIIa inhibitors MI- infarction- ST elevation + change in cardiac enzymes o Chest pain, intense/substernal/ radiates to neck, arm “crushing/constricting” o Levine’s sign- clenched fist against sternum o Atypical sx: elderly, female, Dm o MC injury- left ant. Descending wall o Best Cardiac marker- Troponin I (not an enzyme, but a marker!) o 2 types of MI: 1. Non-ST elevaton II. ST elevaton- Q wave o TX: MONA, heparin, PTCA, CABG Thrombolytics- if ST elevation > 1mm in 2 limbs or >2mm in 2 precordial CI: head trauma, brain tumor, surgery, recent CVA o CX: Dressler’s Syndrome- immune rxn weeks post-MI: pericarditis/pleuritis, fever, malaise Acute Arterial Occlusion- sudden embolic event change in arterial blood flow Sx: pallor, pistol shot, pulselessness, pain, paresthesia, paralysis, cyanosis, skin mottling, necrosis Dx: angiography tx: thrombolytics, anticoagulants Peripheral Arterial Occlusive disease (chronic) MC- lower limbs (gradual narrowing/plaques) caused by athersclerolosis in canals (mc at bifurcations) Risks: smoking, hyperlipidemia, CVA, CAD, Dm, HTN, alcohol Screening test: ABI Sx: Intermittent Claudicaton in feet/calves, brittle toenails + loss of pretibial hair, Leriche’s syndrome: impotence (iliac arteries involved), butt claudication, ED, absent femoral pulses DX: Doppler US TX: lifestyle modifications, HTN control Thromboangitis Obliterans (Burger’s Disease) C- chronic digital ulcers R- Renyard’s phenomenon I- idiopathic S- superficial nodules phelbitis P- pain I- inflammatory vasculitis G- gangrene **involves distal arteries (migratory red tender nodules) DVT Virchow’s triad- venous stasis, endothelial injury, and hypercoaguable state Sx: unilateral lower extremity edema/ palpable venous cord CX: PE Homan’s sign- pain on dorsiflexion dx: Duplex US Tx: compression devices, anticoagulants, Green Field Filter Varicose Veins (mc: saphenous veins) Primary varicose veins- weak valves Secondary varicose veins- due to DVT/ venous HTN MC in women b/c estrogen affects veins Sx: lower extremity edema, telangectasias, spider veins Dx: Dopler US TX: elastic stockings, leg elevaton, sclerotherapy; vein ligation (surgery) Superficial Thrombophelbitis Blood clot in superficial vein Trousseau’s syndrome: migratory venous thrombus sign of pancreatic cancer Sx: linear, tender, red induration within a warm vein, firm palpable cord Tx: NSAIDS, heat, elevation of limb Chronic Venous Insufficiency- blood pools in lower limb MC risk- DVT Causes: obstruction, DVT, valve destruction “Bilateral edema” causes stasis dermatitis (hyperpigmentation in ankles- hemosiderin) DX: US Heart Failure Right Sided Heart Failure: edema, hepatomegaly, JVD Left Sided Heart Failure: pulmonary edema, SOB, DOE, diaphoresis Hypotension (shock)- systolic BP < 90 (or drop of 30 systolic) Mcc- bleeding (hypovolemia) Sx: ↑HR, ↑PVR, ↑ catecholamines, ↑renin, ↑aldosterone, increase in blood volume 1. Hypovolemic Shock: GI bleed, internal bleed or loss of fluid, Mallory-Weiss tear, Borhaave’s Syndrome a. Sx: N, dizziness, weak pulse b. TX: vasopressin 2. Cardiogenic Shock a. Decrease in heart function; mcc- MI b. ↑ SNS vasoconstriction/increased afterload heart works harder c. Myocardial stunning- post ischemis (dysfunction- area will restore itself) d. Hibernating Myocardium- persistently impaired myocardium (decreased coronary blood flow) e. DX: ECHO, EKG, cardiac enzymes f. TX: MONA, heparin, glycoprotein IIb/IIIa inhibitors, vasopressors, PTCA, thrombolytics, CABG 3. Metabolic/Endocrine Shock a. Ass. with change in body chemistry or failure of adrenal/thyroid/pit. Gland 4. Obstructive Shock a. PERICARDIAL Tamponade- fluid in pericardial space i. BECK’s triad: JVD, hypotension, muffled heart sounds ii. DX: ECHO iii. TX: pericardial centesis b. Tension Pneumo c. PE d. Aortic Dissection- “ripping-tearing pain that radiates to back” 5. Distributive shock- decrease in vasomotor tone a. SEPSIS- mcc (risk: cath, surgery, hx of infection) i. TX: ICU, antibiotics + vasopressors b. Anaphylaxis- allergic rxn Tx: EPI pen c. Neurogenic- failure of nervous system to control blood vessels i. Mcc- brain/spinal injury ii. Sx: syncopy, hypotension, bradycardia, hypothermia Myocarditis- inflammation of myocardium (infection, drugs, radiation) MCC: cocksackie B virus Increase in all cardiac enzymes CXR: pulmonary venous markings TX: digitalis, diuretics, vasodialators DX: Bx, US, Echo Cardiomyopathy- primary heart disease 1. Dialated Cardiomyopathy- mc cardiomyopathy a. Systolic dysfunction Thin walls, abnormal systolic pump function b. Causes: alcoholic, severe hypophosphatemis, cocaine c. SX: SOB, DOE, orthopnea, pulmonary edema, JVD, hepatomegaly, PMI is displaced d. DX: CXR; ECG-sinus tachycardia with enlargement; reduced ejection fraction e. Common sx: mitral + tricuspid regurg f. Angiography- dx of ejection fraction g. TX: vasodilator decreases preload/afterload; digitalis, diuretics, catecholamines, B-blockers 2. Hypertrophic Cardiomyopathy- IHSS a. Mcc of sudden cardiac death in young adults who exercise b. Diastolic dysfunction; asymmetric septal hypertrophy c. Decrease blood into ventricle increased obstruction of blood outflow (↓preload, ↓ afterload) d. SX: Mitral Regurg; SOB, DOE, murmurs increase with Valsalva e. DX: ECG, CXR, enlarged heart, ECHO f. TX: b-blockers, surgery 3. Restrictive Cardiomyopathy a. Diastolic dysfunction b. Etiology: fibrosis of myocardium (sarcoidosis, amyloidosis) c. Endocardium may be scarred/ thickened; valves are not involved d. Sx: congestion edema, SOB, hepatomegaly, DOE e. DX: Bx is definitive i. CXR: atrial enlargement with pulmonary venous congestion, edema ii. EKG- sinus tachycardia f. TX: no vasodialators, No digitalis, do not remove pericardium; only tx is transplant g. NOTE: in pericarditis- you can remove the pericardium Heart Murmurs + Valve Disease DX: ECHO, EKG, CXR TX: diuretics, digoxin, B-blocker 1. Mitral Stenosis- diastolic; “Opening Snap” at API; cause: Rheumatic Fever 2. Mitral Regurg- systolic; soft murmur at apex; causes: Marfan’s, mitral calcification 3. MVP- mc valve disorder; “MID-SYSTOLIC Click” 4. Aortic Stenosis- SAD: syncope, angina, DOE (radiates to neck) 5. IHSS- subaortic stenosis increases with Valsalva 6. Aortic Regurg- best heard along left sternal border a. Diastolic produces LV hypertrophy b. Causes: congenital, rheumatic fever 7. Graham Steel Murmur0 at 2nd ICS (pulmonic valve regurg) 8. Pericardial Friction Rub- grating noise from inflammation, heard best with experiation and PT leaning forward Primary HTN: “essential HTN”- idiopathic Syndrome X- HTN, Dm, hyperlipidemia, obesity Mc presentation of HTN: asymptomatic MC sx: HA- suboccipital early in morning Cx: LV hypertrophy, MI, CHF, aortic aneursyms, S4 gallop, TIA, CVA, renal proteinuria, retinopathy Pre-HTN: 120-139/80-89 STAGE 1: 140-159/90-99 STAGE II: > 160/100 Start drugs after 3 months of lifestyle modifications or immediately if they have: o Dm, CAD, Renal Disease o Initial tx: HCTZ HTN Emergency: DBP > 120-130 + end organ damage Dx: Ct, EKG, UA (microalbumnuria Dm nephropathy) TX: IV nitroprusside HTN Medications: 1. Diuretics: CHF, edema (CI: Dm, Gout, hyperlipidemia) a. HCTZ: decrease Na/K/ Mg (increase glucose/ LDL/ Calcium) good for osteoporosis b. Loop: decrease Na/K/Ca (increase glucose/uric acid) c. K-sparing (decrease Na + increase K) 2. B-Blockers- MI, ischemia, migrane (CI: AV block, asthma, CHF, Dm) 3. Ace-Inhibitors- Dm nephropathy, CHF, MI (CI: bilateral renal artery stenosis + pregnancy) a. Side effects- hyperkalemia, bronchospasm 4. ARBS (“sartan”) 5. CCBS (“dipine”)- CI: CHF, AV block (mc side effect: constipation) 6. alpha-blockers- for HTN + BPH a. side effects: OH, bradycardia, dizziness Secondary HTN: 1. Renal Parenchymal disease a. Mcc- glomerulonephritis; also: Dm, chronic pyelonephritis, renal failure b. Kidney can’t excrete NA water retention c. Tx: ACE inhibitor 2. Renal Artery Stenosis- due to athersclerosis, fibromusclar dysplasia in young women a. Excessive rennin increases angiotensin (↑ high rennin) b. PE: epigastric/ renal artery bruits c. DX: US, angiography TX: stent, surgery 3. Primary Hyperaldosteronism (Conn’s disease) a. Unilateral adrenal adenoma b. Low rennin levels ; High aldosterone levels increase in blood pressure c. Sx: hyperkalemia (↑ K in urine and low rennin levels) d. Dx: elevated adolesterone in urine/blood e. Tx: K sparing diuretics 4. Pheochromocytoma episodic HTN a. Tachycardia, sweating, palps, feeling of impending doom b. Dx: urinary vanillymandelic/ catecholamines c. TX: alpha blockers, B-blockers, surgery 5. Cushing’s disease (because increase in ACTH) a. HTN, truncal obesity, buffalo hump, moon face (facial plethora) b. Dx: dexamethasone suppression test tx: surgery 6. Coarctation of Aorta a. HTN is greater in Upper Extremities CHD risk factors: HTN, low HDL, high LDL, family hx CAD equivalents: Dm, HTN, AAA Hyperlipidemia Tx: 1. HMG-CoA Reductase (Statins) most powerful 2. Bile Acid sequestants (nyasin) decreases LDL 3. Fibric Acid Derivatives decreases TB 4. Ezetimbie (blocks absorption in intestine) 5. Probucol decrease both LDL + HDL 6. Niacin inhibits VLDL + LDL a. Adr: pruritis, flushing, gout