outline21403
advertisement
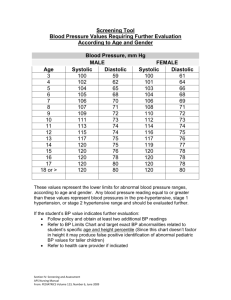
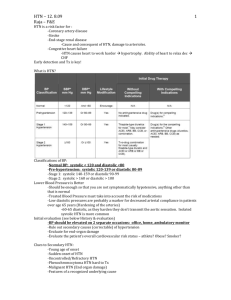
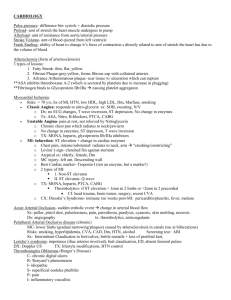
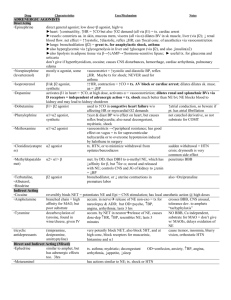
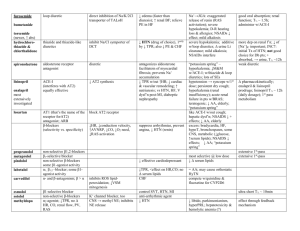
I. The "Top 300 Drugs" – ranked by number of Rxs written – from www.rxlist.com/top200 a. 5 of the top 50 drugs are antidepressants or antibiotics b. 4 of the top 50 drugs are pain killers (opiod combinations) c. 3 of the top 50 drugs are either beta blockers, benzodiazepines, proton pump inhibitors, asthma drugs, or NSAIDs d. 2 of the top 50 drugs are either statins, thyroid supplements, diuretics/HTN, allergy, neuropathy drugs, sleeping pills, or used for CVA prevention e. 1 of the top 50 drugs is either a hormone supplement, ACE inhibitor, diuretic/Lasix, CCB, steroid, diabetic, biphosphonate, K supplement, or muscle relaxant f. So, doctor – what do you make of these commonly prescribed drugs, and what do they imply about the conditions occurring in your patients? Should you be concerned about ocular manifestations? II. Depression a. Very common – 2nd only to HTN as the most commonly seen condition b. Major depression = depressed mood or anhedonia for 2+ weeks, plus 3+ of the following: insomnia, feeling worthless or guilty, fatigue, diminished concentration, change in appetite, psychomotor retardation, recurrent suicidal thoughts c. 50-6% respond to initial therapy (either meds or psychotherapy) d. Serotonin- and norepinephrine-reuptake inhibitors are i. tertiary amine tricyclics (Elavil, Sinequan, Tofranil) ii. secondary amine tricyclics (Norpramin, Pamelor) iii. bicyclic (Effexor) e. SSRIs are Celexa, Prozac, Paxil, Zoloft f. Serotonin antagonist is Remeron g. Norepinephrine- and dopamine-reuptake inhibitor is Wellbutrin III. Hypertension a. Present in 1 in 4 adults in the US; classic defn = systolic > 140, diastolic > 90 b. Risk factor for CVA, MI, renal failure, CHF, progressive atherosclerosis, and dementia; each 20 mm syst or 10 mm syst doubles the risk of CV disease c. The JNC 7 Report from 2003 d. NEW – normal is systolic < 120 and diastolic < 80 e. NEW – pre-hypertension is systolic 120-139 or diastolic 80-89 f. NEW – Stage I HTN is systolic 140-159 or diastolic 90-99 g. NEW – Stage II HTN is systolic ≥ 160 or diastolic ≥ 100 h. Lifestyle modification = diet (BMI 24.9 or less), reduced sodium, increased fruit/vegetable, reduced fat, 30 minutes/day aerobic exercise, ≤ 2 drinks/day i. Pre-HTN treatment: lifestyle modification j. Stage I HTN treatment: Diuretic (still preferred drug per ALLHAT), ACEI, ARB, k. CCB, or combinations (beta blockers less in favor now) l. Stage II HTN treatment: 2-drug combinations IV. Pain Control a. Drugs include NSAIDs, opioid combinations, and meds for neuropathy b. Neuropathic pain is quite common; related to diabetes, infection (herpes, HIV), nerve trauma, stroke, or occurring idiopathically c. Neuropathy: both "negative" and "positive" symptoms d. Pain control is both local (local analgesia, capsaicin) and CNS e. Blockade of calcium channels (gabapentin), sodium channels (amitriptyline) f. Both gabapentin and amitriptyline have many side effects V. Anxiety a. Generalized anxiety disorder is common: 6 months of symptom duration (prominent worrying and impairment) plus 3 or more of the following on most b. c. d. e. days: fatigue, restlessness, poor concentration, irritability, muscle tension, and unsatisfying sleep (but not anhedonia, which is seen in depression) Other anxiety disorders are panic disorder, obsessive compulsive disorder, social anxiety disorder, and PTSD. Symptoms are physical, cognitive, behavioral, affective, and uncontrollable worry Benzodiazepines are the cornerstone of therapy Physical dependence can occur with long-term therapy, but provide rapid relief V. Gastro-esophageal reflux disease (GERD) a. Classic symptoms of heartburn and/or acid reflux b. Laxness of the esophageal sphincter c. Common in the US – 20% or more with symptomatology d. GERD = non-erosive reflux disease, erosive esophagitis, and Barrett's esophagus e. Barrett's demonstates cellular metaplasia; risk of adenocarcinoma f. Parietal cells produce acid in response to acetylcholine (d/t sight/taste/smell of food), gastrin, or histamine (both released by presence of food in stomach). g. Proton pump inhibitors bind within pumps in the secretory canaliculi of parietal cells, resulting in reduced acid production VI. Hyperlipidemia a. National Cholesterol Education Program (NCEP) released Adult Treatment Panels; latest (ATP III) was released in 2003. b. Optimal levels of LDL are now < 100 mg/dL, triglycerides < 150 mg/dL c. Patients are stratified into 3 risk groups, with varying levels of LDL d. Highest risk patient has: CHD/CAD or other atherosclerotic disease (PAD, abdominal aortic aneurysm, symptomatic carotid disease) or diabetes or > 20% risk of CHD within 10 years (per Framingham projection system); goal is LDL < 100 e. Middle risk patient does not have CHD/CAD or atherosclerotic disease, but has 2+ risk factors from among the following: cigarette smoking; HTN (> 140/90) or tx for HTN; low HDL (< 40 mg/dL); family h/o premature CHD (men < 55, women < 65); age (men over 45 years of age, women over 55 years of age); goal is LDL < 130. f. Low risk patient has 0 or 1 risk factors; goal is LDL < 160. g. Steps to reducing cholesterol are (1) dietary counseling and increased activity; (2) addition of high fiber diet; and (3) drug therapy VII. Anti-platelet and anticoagulant drugs a. Factors increasing stroke risk are (1) non-modifiable (age, male gender, nonwhite ethnicity, family history, and past CVA); and (2) modifiable (HTN, DM, a-fib, carotid artery disease, hyperlipidemia, cigarette smoking, obesity, and high alcohol use. b. Types of strokes are either (1) hemorrhagic strokes, caused by saccular aneurysm of large/medium intracranial arteries or hypertensive intracerebral hemorrhage; or (2) ischemic strokes, resulting from large vessels (atherosclerosis drives thrombus formation at carotids and aortic arch), small vessels (middle cerebral artery, circle of Willis, basilo-vertebral arteries), or cardioembolic phemonema (A-fib, mechanical valve, cardiomyopathy, or valvular or rheumatic heart disease). c. Prevention of strokes requires treating modifiable factors for atherosclerosis (HTN, systolic HTN in the elderly, hyhperlipidemia). d. Prevention of strokes also uses anti-platelet aggregation drugs (reduces thrombus formation by reducing aggregation of platelets on diseased arteries); strategy reduces risk by 25-30%; ASA, Plavix, or Aggrenox e. Anticoagulation with warfarin reduces risk of cardioembolic phenomena in patients with A-fib or mechanical heart valves VIII. Postmenopausal osteoporosis a. Bone mass or mineral density is reduced, causing "microarchitectural deterioration" and increased bone fragility with increased susceptibility to fractures. b. Women at age 50+ = lifetime risk of vertebral fracture is 1 in 3, and risk of hip fracture is 1 in 6. c. Osteoporosis is clinically silent until a fracture occurs d. Tested by DEXA (dual-energey X-ray absorptiometry e. Risk factors for osteoporosis are environmental (cigarette smoking, alcoholism, inactivity, thin or low body weight), drug therapy (steroids, antiepileptic drugs, anticoagulant drugs), endocrine disease (hyperparathyroidism, Cushing's disease), rheumatologic disease (RA, ank spondylitis), genetics f. Drug therapy works to reduce bone resorption g. Biphosphonates inhibit the normal function of osteoclasts (which is absorption and removal of bone); the result is increased bone mineral density h. Biphosphonates are associated with ocular inflammation. The worst offender (pamidronate/Aredia) is used for tumor-induced hypercalcemia or Paget's disease; alendronate/Fosamax and risedronate/Actonel are less toxic. IX. Allergy management a. Allergy, whether seasonal or perennial, is a very common condition in the US. b. Traditional strategies of oral antihistamines have been augmented markedly by other drug modalities, often with fewer side effects. c. First generation antihistamines remain effective, but their sedating and anticholinergic side effects are well known (Acrivastine/Semprex, brompheniramine OTC, carbinoxamine/Palgic, chlorpheniramine OTC, clemastine/Tavist, cyproheptadine, diphenhydramine, hydroxyzine/Atarax, triprolidine/Actifed) d. Second generation antihistamines cause less sedation (cetirizine/Zyrtec, desloratadine/Clarinex, fexofenadine/Allegra and generic, loratadine/Claritin OTC). e. Nasal steroids are increasingly popular (beclomethasone/Beconase, budesonide/Rhiocort, flunisolide/Nasarel, fluticasone/Flonase and generic, mometasone/Nasone/Nasacort. f. Mast cell stabilizer nasal spray (cromolyn/Nasalcrom) g. Antihistamine nasal spray (azelastine/Astelin – aka Optivar for eyes) h. Leukotriene antagonist (montelukast/Singulair) i. With such a profusion, plus crossover from asthma treatment, which is best? X. Erectile Dysfunction a. Erectile dysfunction (ED) due to many causes: major cause is aging, but risk factors include DM, HTN, hyperlipidemia, CAD, trauma, post-prostatectomy, cigarette smoking, depression, antidepressants (particularly SSRIs). b. ED is very common, increasing with age – 52% in men 40-70 years old, and 67% in men older than 70. c. Sexual stimulation involves release of nitric oxide (NO) in corpus cavernosum, with stimulation of cGMP synthesis, which relaxes smooth muscle in the corpus and penile arteries; end result is increased penile blood flow and an erection. d. Phosphodiesterase type 5 inhibitors (PDE5 inhibitors) enhance the effect of NO by inhibiting phosphodiesterase 5, which would otherwise degrade cGMP e. PDE5 inhibitors are sildenafil (Viagra), vardenafil (Levitra), and tadalafil (Cialis) f. All PDE5 inhibitors are contraindicated with nitrates (ie, NTG) due to exaggerated vasodilation; normal side effects include headaches, facial flushing, and nasal congestion from arterial vasodilation. g. Viagra side effects include blue color distortion and blurred vision. h. NAION has been tenuously associated with PDE5 use but most patients have had other risk factors (including DM, HTN, CAD, hyperlipidemia, nocturnal i. hypotension) or the "disc at risk." Many of the 25 reports of NAION did not have the episode occurring within the 4-hr plasma half-life of the drug. The only men who must avoid these drugs are those with a history of NAION in one eye already. XI. Conclusions - some of these very commonly managed conditions have little impact on eye health or the visual system, and the drugs used for their treatment have similarly little ocular impact. Other conditions (HTN, hyperlipidemia, stroke risk and prevention) have tremendous inter-relationships with the visual system. Finally, other conditions may have little direct impact but the medications used in management may have marked ocular toxicities associated with their use. The Top 50 of the Top 300 List Hydrocodone/APAP Lipitor Amoxicillin Lisinopril Hydrochlorothiazide Atenolol Zithromax Furosemide Alprazolam Toprol-XL Albuterol aerosol Norvasc Levothyroxine Synthroid Metformin Zoloft Lexapro Ibuprofen Cephalexin Ambien Prednisone Nexium Triamterene/HCTZ Propoxyphene-N/APAP Zocor Singulair Prevacid Metoprolol Fluoxetine Lorazepam Plavix Oxycodone/APAP Amoxicillin/Clavulanate Advair Diskus Fosamax Effexor XR Warfarin Paroxetine Clonazepam Zyrtec Protonix Potassium Chloride APAP/codeine Trimethoprim/SMZ Gabapentin Premarin Floanse Trazodone Cyclobenzaprine Amitriptyline