- The 1st Kuwait
advertisement
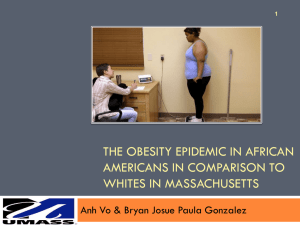
The 1st Kuwait-North American Update in Internal Medicine Cardiology: Challenging Cases Michael M. Givertz, M.D. Medical Director, Heart Transplant/Mechanical Circulatory Support Brigham and Women’s Hospital Associate Professor of Medicine Harvard Medical School Boston, MA Case Presentation: AK 74 yo Greek woman with new onset HF • Cardiac risk factors: + HTN, DM; - cigs, lipids, FHx • History of MI (inferior Q waves) • 2007: Acute onset chest and epigastric pain in Greece – US + gallbladder sludge, returned to U.S. for lap chole – In OR: pus in gallbladder, liver bx + cirrhosis – Pre-op echo: LVEF 60%, no WMAs, mild MR • 2011: Viral illness → progressive DOE and LE edema – – – – LVEDD 56, EF 40%, mod RV dysfxn, 3+ MR, 3+ TR Furosemide → 7-pound weight loss, marked ↓ symptoms Beta-blocker added to ACE inhibitor Transferred for cath and further management Case Presentation: AK • Cath: RA 14, PA 48/22/31, PCWP 26 (V 29), CO 6.5, insignificant CAD, EF 47% with global HK, 2+ MR • Palpitations lying in bed, no orthopnea/PND. Appetite “too good”, weight stable. Poor sleep 2° nocturia. • PMHx: osteoporosis, H. pylori gastritis, basal cell CA • Meds: lisinopril 10 mg qd, metoprolol 12.5 mg bid, furosemide mg 40 qd, glipizide 5 mg bid, lansoprazole mg 30 qd • Habits: no cigarettes, occasional glass of ouzo • FHx: no CAD, CMP or sudden death • SHx: married, retired from restaurant business Case Presentation: AK • Physical exam – – – – – Thin older woman, slightly anxious lying at 30°, malar flush BP 140/60, HR 104 and regular, T 99.6, Ht 5’4, Wt 48.2 JVP 12 cm, no HJR Lungs clear bilaterally Non-palpable PMI, parasternal lift, tachycardic RR, soft SEM at LSB, trace HSM at apex, +S3, no rub – Abdomen soft, NT, no HSM – Extremities warm, no edema • Na 141, K 4.4, BUN 25, Cr 0.8, glucose 224, TC 108, Hct 32 (MCV 90), WBC 12K, BNP 735, TnI < assay • CXR: mild cardiomegaly, “no heart failure” Electrocardiogram Cardiac MRI LVEDVI 159 (56-99), LVEF 36%, RVEF 47%, no scar, no edema Additional Labs • • • • • ANA and RF negative ESR 18, CRP 1.4 Iron and TIBC normal; ferritin 727 (20-400) RPR and HIV negative (ordered by the medical student) Carnitine and selenium levels normal (ordered by the resident) • TSH < assay (0.5-5.7) • T4 18.3 (4.6-10.7) • Free T4 8.6 (0.9-1.7) Dx: Thyrotoxicosis, high-output heart failure What Did We Miss? • • • • History: palpitations, appetite “too good” (no wt chg) Exam: 140/60, HR 104 (no ectopy), anxious, flushed Labs: glucose 224, TC 108, Hct 32 (MCV 90) Echo and MRI: mild-mod biventricular dysfxn, mod secondary MR/TR and secondary pulm HTN • Cath: CO 6.5, but at 5’4, 48.2 kg…BSA 1.46 → CI 4.5 • Repeat ECG during palpiations: Avoid Red Herrings • • • • • • Viral illness Greek ancestry Cryptogenic cirrhosis Overestimation of alcohol use Secondary (functional) valvular regurgitation Secondary (post-capillary) pulmonary hypertension Other Causes of High-Output HF • Systemic arteriovenous fistula – History of vascular surgery or trauma – Cardiac catheterization – ESRD • Other endocrinopathies – Carcinoid, pheochromocytoma • Thiamine (vitamin B1) deficiency – Alcoholic, fad diets • Skeletal disorders (e.g., Paget’s) • Dermatologic disorders (e.g., psoriasis) • Cirrhosis All are potentially treatable Treatment of Hyperthyroidism • Goal: return patient to euthyroid state – Leads to normalization of HR, pulse pressure, and CO – Reverse remodeling: ↓ EDD, ↑ EF • Anti-thyroid medication • Beta-blockers – Especially in patients with tachycardia, AF/flutter – BUT caution to avoid further ↓ contractility • Radioactive iodine, thryoidectomy • NB: amiodarone Case Presentation: AB 28 yo African American man with LE edema • Cardiac risk factors: + HTN, cigs; - DM, FHx; ? lipids • Grew up in Boston, struggled with obesity (109 kg entering high school) • SOB during gym class attributed to asthma • 2009: First noted to be hypertensive (150/100) – Started on HCTZ 12.5 mg daily – Told to exercise and lose weight (did neither) • 2011: Presented to PCP with increased SOB, fatigue and new LE edema Case Presentation: AB • • • • ROS: shoulder and back pain on ambulation PMHx: asthma, bilateral hernia repair Meds: HCTZ 25 mg daily, albuterol inhaler prn Habits: cigarettes 1 ppd since age 14, occasional marijuana; no alcohol, cocaine or IVDU; 1 tattoo • FHx: M and F with HTN, DM and obesity; sister with hypothyroidism; half-brother with hepatitis C • SHx: engaged, studied computers in community college, currently working nights in security Case Presentation: AB • Physical exam – – – – – – – Obese young man, appears tired with dull affect BP 160/100, HR 51 and regular, Ht 5’6, Wt 147.3, BMI 52.3 JVP difficult to assess due to body habitus Decreased BS at bases, no wheeze Slow RR, distant S1 and S2, no murmur heard Abdomen obese, NT Extremities warm, 2-3+ edema (R>L) to below knees • Na 141, K 4.0, BUN 11, Cr 1.3, LFTs normal, BNP 21, Hct 50.6, plt 254K, A1c 6.4 • CXR: top normal heart size, clear lungs, no effusions Electrocardiogram Echocardiogram LVEDD 50, mod LVH (15 mm), LVEF 50%, impaired relaxation, mild RV enlargement and dysfunction, mild TR, estimated PASP 54 Diagnostic Considerations • Is this HF with preserved EF (HFPEF)? • What about the RV dysfunction and pulmonary HTN? – – – – – HIV negative No history of diet pills Echocontrast study negative for shunt CT scan negative for PE PFTs: moderate restrictive defect, normal DLCO • Role of RHC? – RA 16, PA 54/27/36, PCWP 18, CO 4.8, PVR 310 – Saturation run: no step up • What about morbid obesity? Prevalence of Obesity (BMI > 30) Among US Adults: NHANES 2007-2008 Men Women 60 Prevalence, % 50 40 30 20 10 0 All White Black Hispanic Mex-Am Flegal et al., JAMA 2010;303:235 Obesity is an Independent Risk Factor for Heart Failure 6 5 Adjsuted HR • Framingham Heart Study • 5881 patients followed for 1st episode HF over 14 yr • Increased prevalence of DM and HTN with ↑ BMI • Overall, 2-fold increase risk of HF associated with BMI > 30 kg/m2 Men Women 4 3 2 1 0 25-29.9 30-34.9 35-39.9 > 40 BMI, kg/m2 Kenchaiah et al, N Engl J Med 2002;347:305 Pathophysiology of HF in Obesity Hemodynamic Factors Vascular Injury Neurohormonal Factors Heart Failure in Obesity SleepDisordered Breathing Rheologic Factors Systemic and Pulmonary Hypertension Polysomnogram Severe OSA (AHI 46/h, oxygen saturation ↓ 81%) Pulmonary Hypertension is Common in Patients with HFPEF • N = 244 HFPEF • Age 76, 45% male vs. • N = 719 HTN w/o HF • Age 66, 44% male In both groups, patients with PH were older, had higher systolic BP, higher PCWP and larger LA Lam et al., J Am Coll Cardiol 2009;53:1119 Bariatric Surgery and Reverse LV Remodeling • N = 423 morbidly obese patients vs. 733 non-surgical controls • At 2-years: BMI 15.4 kg/m2 with bariatric surgery (vs. 0.03) • Significant reductions in BP, HR and lipids Owan et al., J Am Coll Cardiol 2011:57:732 CPAP and Reverse RV Remodeling N = 47, BMI 38 ± 9, OSA with mean AHI 63 60 p < 0.05 RVSP, mmHg 50 40 30 20 10 0 0 Cardiac MRI 3 6 12 Months Colish et al., Chest 2012;141:674 PDE-5 Inhibition in HFPEF and Pulmonary Hypertension N = 44, chronic HTN, LVEF ≥ 50%, PASP > 40 mmHg Sildenafil also MPAP 42%, ↑ RVEF and improved QOL Guazzi et al., Circulation 2011;124:164 Back to Our Patient • HCTZ changed to furosemide with good diuretic response • ACE inhibitor added with good BP response • Started on CPAP (but did not tolerate it) • Referred to nutritionist (but did not go) • Prescribed sildenafil (but could not afford it) • Follows up intermittently in HF clinic last admit Dec. 2013 Thank you for your attention