Lymph I: The Peripheral Lymph System
advertisement
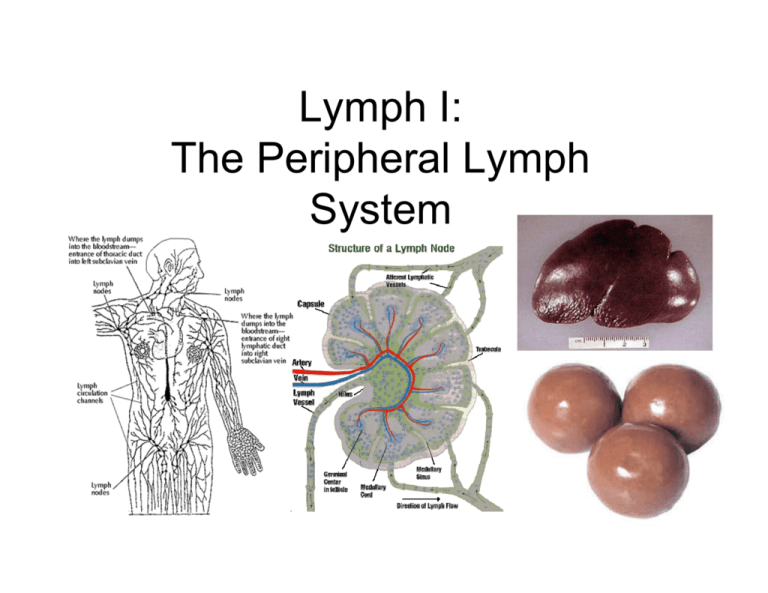
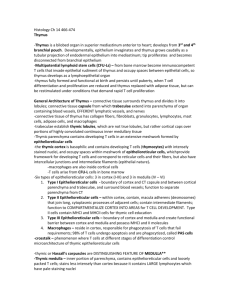
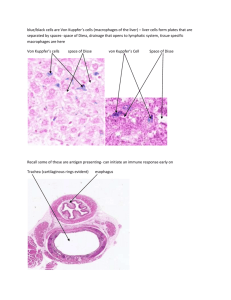
Lymph I: The Peripheral Lymph System Peripheral = Secondary • Primary Immune Organs = bone marrow, thymus – Site of maturation of cells of the immune system • Secondary Immune Organs = Nodes, MALT, spleen – Filter blood and lymph – Site of antigen, immune system interaction Lymph Vessels • Valves • Carries Lymph from tissue Æ lymph nodes Æblood via thoracic duct – – – – – Fluid Proteins Ingested fats Particulate matter Antigen Lab 11 Slide 7 Peripheral Lymph Organs • Diffuse – Eg. Peyer’s patches, tonsils, appendix – Non-encapsulated – In GI, respiratory, GU, and tracts, tonsils, appendix • Encapsulated – Spleen, lymph nodes The Follicle Primary - Lymphocytes Secondary - Germinal Center - Looks pale! - Antigen has been encountered Lab 11 Slide 9 Secondary Follicle Germinal Center • Pale staining center: Plasmablasts = B cells – Large, euchromatic nuclei – Prominent nucleoli – Mitotic activity • Dark periphery – T cells helping out Lab 11 Slide 15 Diffuse Lymphoid Tissue • At most likely site of infection • GALT = “Gut Associated Lymphatic Tissue” – Prototype for diffuse lymphatics: S/B/MALT Lab 11 Slide 4 GALT • “Peyer’s patches” • In lamina propria of GI • No afferent lymphatics! – Antigen enters via transcytosis across M cells Lab 11 Slide 4 Tonsils Diffuse Lymph organs! Not encapsulated! You may see stratified, squamous nonkeratinized epithelium. Lab 11 Slide 1 Encapsulated Lymphoid Tissue • Eg. Spleen, Lymph nodes • Both afferent and Efferent lymphatics Lab 11 Slide 5 Lymph Node Architecture • • • • • Capsule: DICT (collagen I is red/brown in silver stain) with trabeculae that extend into stroma of node (collagen III is black/brown) Subcapular space with macrophages (visualized with India ink) Cortex – Germinal centers w/ B cells – Paracortex around follicles – Deep cortex w/ high endothelial venules – Juxtamedullary cortex Medulla w/ Plasma cells and Macrophages – Cords – Sinuses Hilum – Efferent lymphatics – Afferent and efferent bvv Lab 11 Slide 14 Lymph Node Architecture • • • • • Capsule: DICT (collagen I is red/brown in silver stain) with trabeculae that extend into stroma of node (collagen III is black/brown) Subcapular space with macrophages (visualized with India ink) Cortex – Germinal centers w/ B cells – Paracortex around follicles – Deep cortex w/ high endothelial venules – Juxtamedullary cortex Medulla w/ Plasma cells and Macrophages – Cords – Sinuses Hilum – Efferent lymphatics – Afferent and efferent bvv Lab 11 Slide 6 Lymph Node Architecture • • • • • Capsule: DICT (collagen I is red/brown in silver stain) with trabeculae that extend into stroma of node (collagen III is black/brown) Subcapular space with macrophages (visualized with India ink) Cortex – Germinal centers w/ B cells – Paracortex around follicles – Deep cortex w/ high endothelial venules – Juxtamedullary cortex Medulla w/ Plasma cells and Macrophages – Cords – Sinuses Hilum – Efferent lymphatics – Afferent and efferent bvv Lab 11 Slide 12 Lymph Node Flow Afferent Lymphatics Æ Subcapsular sinus Æ trabecular sinuses Æ medullary sinus Æ efferent lymphatics Lab 11 Slide 5 Lab 11 Slide 14 Thymus and Spleen Are you getting immune to exam blocks yet?? Thymus=“Education of T cells” • Thymocytes mature and proliferate in the thymus • Thymocytes undergo positive and negative selection • Only T cells that react weakly with self proteins survive Thymus has 3 cell types • Epithelioreticular cells are large, pale, and stellate (they are not reticular fibers!) • Thymocytes are immature T cells • Macrophages phagocytose T cells that react too strongly with self Thymocytes Epithelioreticular cells The Cortex and Medulla • The cortex stains darkly basophilic because there lots of small lymphocytes with intensely stained nuclei • The medulla stains light because it has less lymphocytes with more cytoplasm Medulla Cortex Blood-Thymic Barrier • Separates developing T cells from blood (prevents T cells from recognizing foreign proteins as “self”) • Components (from outside) – Capillary endothelium – Endothelial basal lamina – Perivascular connective tissue sheath – Basal lamina of epithelioreticular cell – Epithelioreticular sheath Hassall’s corpuscles • Hassall’s Corpuscles instantly signify the thymus!! • They are concentrically arranged keratinizing and degenerating epitelioreticular cells and macrophages • They are found in the medulla The Adult Thymus • Adult thymus shrinks • Adipose tissue replaces thymic tissue • Medulla and cortex are harder to differentiate because there are less lymphocytes The Spleen: What is it good for? 1. Filters blood 2. Iron Retrieval 3. RBC reserve 4. Immune Response* 5. Fetal Hematopoiesis The ‘White’ Pulp • Appears basophilic on H&E and red on silver stain • Site where immune response is mounted; formation of germinal centers • Germinal centers with B cells and B cell derivatives push the ‘central artery’ off to the side White Pulp Vasculature • The central artery is found in the white pulp • The central artery is surrounded by the PALS, which is T cells • Penicilli branch from the central artery into the red pulp Red Pulp Vasculature: • Penicilli give rise to ellipsoids • Ellipsoids are capillaries ensheathed by reticular cells and macrophages; their lumens are often occluded in histo sections • Blood is filtered by macrophages through fenestrations in the sinusoids Sinusoids See how the basal lamina is interrupted; evident with both stains The Red Pulp • Appears Red on H&E • Composed of sinusoids and Cords of Billroth • The cords are the parenchyma of the red pulp; they are composed of reticular tissue w/ macrophages, red blood cells, and lymphocytes Silver Stain *Notice how reticular fibers are evident with silver stain and not H&E *Notice the difference in appearance with the two different stains That’s all folks • We hope you got a good education (THYMUS) & that you filtered out what was important (SPLEEN)