Lymph II Thymus
advertisement

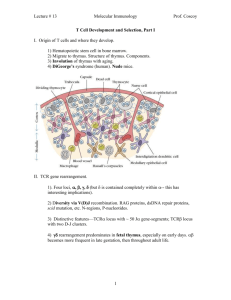
Vinny - vbv2101@columbia.edu Anand - apd2104@columbia.edu Lymph II: THYMUS FUNCTION: “Educate T cells”: Thymocytes (immature T lymphocytes) mature and proliferate in the thymus. T cells undergo positive and negative selection in the thymus. Positive Selection: T cells that react weakly with self MHC and self antigens presented by epithelioreticular cells survive. Negative Selection: T cells that react strongly are eliminated. Result of Selection Processes: Only 5% of thymocytes survive to leave the thymus as T cells. THREE CELL TYPES: 1) Epithelioreticular cells: Derived from endodermal epithelium. There are NO reticular fibers in the thymus. Involved in the selection, proliferation and/or death of thymocytes. These cells are large, pale and stellate. The chromatin is loose and prominent nucleoli can be seen. Large nuclei, acidophilic cytoplasm. 2) Thymocytes: Derived from stem cells produced by the bone marrow. Will differentiate into T cells. Thymocytes undergo selection by interactions with epithelioreticular cells. They stain strongly basophilic from their round nuclei and very condensed chromatin. 3) Macrophages: Found in the cortex and near the cortico-medullary junction. Phagocytose T cells that react too strongly with self-antigens. Also present antigens to lymphocytes. TWO LOBES: Not always clearly defined. CAPSULE: Dense, fibrous, irregularly-arranged connective tissue. Trabeculae from the capsule divide the lobes into many incomplete lobules with a peripheral dark cortex and central paler medulla. Septae NEVER penetrate the medulla. Blood vessels and efferent lymphatics travel along the trabeculae. There is NO subcapsular space (unlike lymph node). CORTEX: Stains strongly basophilic due to numerous closely packed small lymphoctes with intensely staining nuclei. Thymocytes predominate. Epithelioreticular cells are obscured by the thymocytes. The cortex stains more blue than the medulla, because of the thymocytes. Can also see some macrophages, sometimes with phagocytosed thymocyte nuclei in the cytoplasm. BLOOD-THYMIC BARRIER: Arterioles that branch into the cortex are surrounded by a perivascular connective tissue sheath containing macrophages, a basal lamina, and an epithelioreticular cell sheath. This forms a highly impermeable barrier to macromolecules and is called the blood-thymic barrier. The blood-thymic barrier allows thymocytes to mature and undergo selection in an environment protected from contact with foreign antigens. MEDULLA: Stains lightly because there are less lymphocytes with relatively more cytoplasm. After selection, T cells leave the thymus. They migrate between the cells of the low cuboidal epithelium of postcapillary venules in the medulla and at the cortico-medullary junction. There are fewer thymocytes in the medulla, which means that the epithelioreticular cells are more visible than in the cortex Hassall’s corpuscles are concentrically arranged keratinizing and degenerating epithelioreticular cells and macrophages found in the medulla of the thymus. They are highly eosinophilic from the keratin. The presence of Hassall’s corpuscles instantly signifies Thymus. APPEARANCE IN ADULTHOOD: The thymus is critical for establishing the immune system during childhood, but begins to shrink just before puberty. In adults, thymic tissue is replaced by adipose tissue (age involution), however thymocytes are continually produced into old age. In adults, it is difficult to distinguish between the cortex and medulla by the concentration of thymocytes, however Hassall’s corpuscles can still be identified in the medulla. Notes: The thymus does NOT have lymphatic nodules (but can appear as if it does)! The thymus does NOT have afferent lymphatic vessels!