COMPARATIVE ANALYSIS OF HYPERTENSION AND ITS CAUSES
advertisement
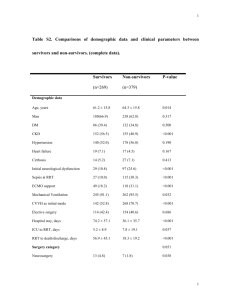
COMPARATIVE ANALYSIS OF HYPERTENSION AND ITS CAUSES AMONG RENAL REPLACEMENT THERAPY PATIENTS Summary Background Life prolongation of patients with chronic kidney disease (CKD) treated conservatively or after renal replacement therapy (RRT) increases the time of exposure to harmful factors related to lifestyle, environment and treatments leading to the prevalence of cardiovascular diseases (CVD. In renal replacement therapy (RRT) patients, the target values of blood pressure (BP) are being continuously modified and excessive fat tissue may even have a protective impact on the risk of mortality due to cardiovascular causes – the “obesity paradox”. Automatic 24-h ambulatory blood pressure monitoring (ABPM) enables credible and precise comparison of BP values and 24-h BP circadian rhythm between patients undergoing hemodialysis (HD), peritoneal dialysis (PD) and post- kidney transplant (KTx). The measurement enables 24-h recording of BP values during taking of the patient’s daily vital functions. The health-related quality of life (HRQoL) may determine the efficacy of RRT. Purpose The purpose of this study was to compare the occurrence of arterial hypertension (HTN) and its underlying causes in patients in the first year after KTx, and in HD or PD patients. Material and Methods A group of 120 RRT patients (PD, n=30; HD, n=40; KTx, n=50) was analyzed. The following research tools were used: (1) 24- or 44-h ambulatory blood pressure monitoring (ABPM); (2) bioelectrical impedance analysis (BIA); (3) traditional method – office BP; (4) Morisky-Green test; and (5) disease history; (6) Medical Outcomes Study 36 - the Short Form 1 (SF-36v.1); (7) Kidney Disease Quality of Life Short Form (KDQOL-SF™ v1.3). The significance level was p<0.05. Results The results demonstrate that the HTN prevalence in patients in the 3rd month after KTx stands at 85% did not change over the follow-up period of 12 months. The efficacy of anti-hypertensive pharmacotherapy had changed slightly – 38% in the 12th month after KTx vs. 33% in the 3rd month after KTx. In patients in the 12th month after KTx, as opposed to patients in the 3rd month after KTx, BP values went up along with increased creatinine concentration (r=0.38; p<0.05). The correlation between urine protein presence and BP was similar (r=0.38; p<0.05). In patients in the 12 month after KTx, a positive correlation of hemoglobin concentration with BP (r=0.31; p<0.05) was shown. Comparing dipping in the 3rd and 12th month after KTx, we found a rise in the frequency of at least 10% of the drop of night-time BP in favor of patients in the 12th month after KTx (16% vs. 40%; p< 0.05). HD patients showed the statistically significant impact of fat tissue growth on reducing BP. The cardioprotective nature of the fat tissue concerned both the whole body fat (r=–0.34; p<0.05) and abdominal fat (r=–0.44; p<0.05). Fat-free body mass corresponding to the skeletal muscle protein mass expressed as FFMI demonstrated a negative correlation with BP (r=–0.35; p<0.05), which proves the cardioprotective role of muscle mass in HTN development. A clinically significant correlation revealed that the increase in the pre-dialysis creatinine concentration reduced BP (r=–0.22; NS). This also indirectly endorses the protective role of muscle mass in HTN pathogenesis. Our study revealed HTN (on a basis of ABPM values and anti-hypertensive treatment) in 90% of PD patients, in 83% of HD patients in the first 24 h after hemodialysis, and in 95% of HD patients in the second 24 h after hemodialysis. In own study, no impact of Kt/V and URR on BP of HD patients has been shown. Among HD patients, the following conversion was demonstrated: from non-dipping in the first 24 h to inverse-dipping in the second 24 h of the interdialytic period (45% vs. 64%; p<0.05). Among PD patients, along with increasing differences between measured TBW and iTBW, BP was increasing (r=0.40; p<0.05). We showed the cardioprotective nature of the acid-base balance. Along with the balancing of chronic metabolic acidosis (increased stHCO3), BP decreased (r=–0.41, p<0.05) 2 An analysis of correlation in RRT groups demonstrated that Physical Component Summary (PCS) was significantly statistically correlated with the following: SBP (r=–0.54; p<0.05), DBP (r=–0.58; p<0.05) and creatinine concentration (r=–0.46; p<0.05) in the 12th month after KTx; hematocrit (r=0.40; p<0.05), hemoglobin concentration (r=0.24; p<0.05) among HD patients; SBP (r=–0.70; p<0.05), DBP (r=–0.40; p<0.05), age (r=0.68; p<0.05), BMI (r=–0.74; p<0.05), creatinine concentration (r=0.41; p<0.05), total cholesterol concentration (r=0.57; p<0.05), and LDL concentration (r=0.54; p<0.05) among PD patients. Conclusions 1. The results of the study show insufficient monitoring of arterial hypertension in RTRs. 2. Fat tissue plays a cardioprotective role in the development of hypertension in HD patients. 3. The transplanted kidney function parameters (creatinine, urine protein presence) demonstrate positive correlation with ABPM in the 12th month after KTx. This shows the possibility of early identification of patients exposed to development of chronic allograft nephropathy. 4. HRQOL of ESRD patients differed depending on the RRT method used: highest values were shown by post-KTx patients, lower values by PD patients, and the lowest ones by HD patients. 5. Along with patient age, increased BP, and BMI, a drop in value of HRQOL in post-Tx or PD patients was observed. 3