CULTURE AND POSTPARTUM DEPRESSSION
advertisement

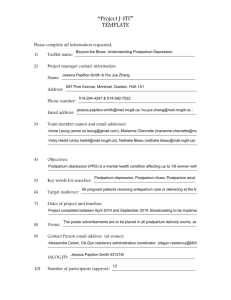
CULTURE AND POSTPARTUM DEPRESSSION PRESENTERS: GLORIA CANTOR MSN, CNS SY VANG DSM-IV Criteria for depression: 1) 2) 3) 4) 5) 6) 7) 8) 9) depressed mood decreased interest/enjoyment of usual activities decrease or increase in appetite insomnia or hypersomnia psychomotor agitation or retardation fatigue or lack of energy feelings of worthlessness or excessive guilt decreased concentration or ability to think recurrent thoughts of death or suicidal ideation Five or more symptoms must be present for 2 weeks, represent a change from previous functioning and at least one of the symptoms is either depressed mood or loss of interest/pleasure. Postpartum Depression: 1) 2) Can begin 2 weeks postpartum up to one year postpartum Symptoms consistent with DSM-IV criteria but often excessive guilt or anxiety about baby, being an adequate mother 3) Prevalence rates estimated at 10% to as high as 40% 4) Immigrant mothers at increased risk of PPD Common Risk Factors in PPD: (Beck, 2001) 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) Prenatal depression Childcare stress Life stress Lack of social support Prenatal anxiety Marital dissatisfaction Previous history of depression Low self-esteem Low socio-economic status Marital status Unwanted/unplanned pregnancy Cultural risk factors: 1) 2) Loneliness 3) Fear of failure 4) Helplessness to fulfill traditional role 5) Lack of knowledge 6) Pre-migration trauma 7) Immigration stress 8) Inability to carry out cultural rituals 9) High expectations for new mothers 10) Having a female infant Cultural factors possibly mitigating development of PPD: 1) Distinct postpartum period for mothers 2) Extended family providing help and care for the new mother 3) Special personal attention to the mother 4) Social seclusion 5) Mentoring of the new mother by older women Cultural differences in explaining PPD 1) Typically non-biological 2) Role conflicts 3) Advice conflicts 4) Lack of support Barriers to seeking treatment: 1) Somatization of emotional problems 2) Cultural norms 3) Lack of knowledge 4) Language barriers 5) Fear of being labeled “mentally ill” 6) Family disapproval 7) Religious beliefs Health Professional Barriers: 1) Lack of knowledge about PPD and its cultural presentations 2) Failure to ask 3) Failure to refer 4) Language barriers 5) Cultural biases 6) Lack of time BIBLIOGRAPHY Nahas, V and Amasheh, N. (1999). Culture Care Meanings and Experiences of Postpartum Depression among Jordanian Australian Women: A Transcultural Study. Journal of Transcultural Nursing 10, 3745. Fonte, J. and Horton-Deutsch, S. (2005). Treating Postpartum Depression in Immigrant Muslim Women. Journal of the American Psychiatric Nurses Association 11 (1), 39-44. Beck, C. (2001). Predictors of Postpartum Depression: An Update. Nursing Research, 50, 275-285. Goyal, D., Murphy, S. , and Cohen, J. (2006). Journal of Obstetric, Gynecologic, and Neonatal Nursing, 35, 98-104. Nahas, V. and Amasheh N. (1999). Postpartum Depression: The lived experiences of Middle Eastern Migrant Women in Australia. 44(1), 65-74. Dindar, I. And Erdogan, S. (2007) Screening of Turkish Women for Postpartum Depression Within the First Postpartum Year: The Risk Profile of a Community Sample. Public Health Nursing 24(2) 176183. Maternidad Latina (2007) Postpartum Latinas Cry for Mental Health Services. North Carolina Healthy Start Foundation Newsletter, November-December 2007. Stuchbery, M, Matthey, S, and Barnett, B. (1998) Postnatal Depression and Social Supports in Vietnamese, Arabic and Anglo-Celtic Mothers. Social Psychiatry and Psychiatric Epidemiology, 33(10) 483-490. Wisner, K, et al. (2002) Postpartum Depression. New England Journal of Medicine, 347 (3) 194-199. Kendall-Tackett, K. (1994) Postpartum Rituals and The Prevention of Postpartum Depression: A Cross-Cultural Perspective. Newsletter of the Boston Institute for the Development of Infants and Parents, 13 (1) 3-6.