It`s Time to Talk About Postpartum Depression
It’s time to talk about postpartum depression
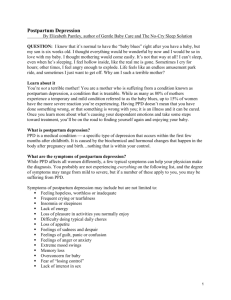
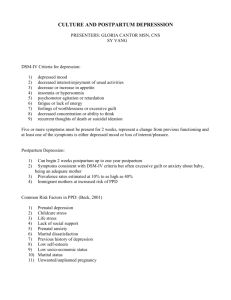
Having a baby rocks your world. Suddenly your priorities shift, your time vanishes and sleep becomes a rare and precious commodity. It’s a dramatic adjustment for anyone. But for some new mothers—about 1 in 5— the transition is even more difficult, because they’re suffering, usually unknowingly, from post-partum depression (PPD).
Ten years ago, PPD was buried in the medical books. These days, it’s increasingly in the news. Moms are coming forward with their stories. Doctors are discussing it. Even Marie Osmond wrote a best-selling book about her PPD experience. And this is good. Because the more people talk about post-partum depression, the more they’ll understand it. And the easier it will be for mothers who suffer to get the support and treatment they need.
So what is PPD and how can you tell if you or someone you know has it? In understanding PPD, it’s helpful to know what it is not. It is not the common “baby blues,” a brief and fleeting period of tearfulness caused by fluctuating hormones that strikes 50-80% of new moms in the first few weeks after delivery. PPD is also different from postpartum psychosis—a rare and extreme condition accompanied by hallucinations and delusions that can put the mother at risk of harming her baby or herself.
PPD is the gray area in-between. It is characterized by strong, lingering feelings of sadness, guilt, anxiety and worry. It can start anytime in the first year after birth and last up to a year. PPD is a not a sign of a weak person or a bad mother; it’s a real illness that can affect any new mom. The good news is, it is highly treatable.
People aren’t comfortable talking about PPD for a number of reasons. New mothers often don’t want to admit their fears and worries at what is supposed to be a joyful time. They may feel confused or ashamed. Spouses, friends and relatives may not recognize the depth of the problem or know what to say.
Even if the suffering mother does speak up, she may receive well-meaning but misguided advice: take a nap, get more exercise, hire a babysitter, go shopping. While these suggestions might help a mom who is simply tired and stressed out, they will do nothing to address or alleviate true postpartum depression.
If you’re concerned that you or someone you care about might be suffering from PPD, you need to speak up. And a call to the EAP is a great way to figure out what to say or do. They can guide you to information and resources that can help you identify the symptoms. And they can help you connect with others—doctors, counselors, local support groups—who can help.
Recovering from postpartum depression—even talking about it—requires a conscious effort. It may seem easier to mind your own business or hope it will pass. But that won’t get mom—and her baby—the help they need right now. If you’d like help talking about postpartum depression, call your Employee Assistance
Program at 1-8 **-***-**** .
It’s a free resource, available 24 hours a day, 7 days a week, offering counseling, information and referral services for all kinds of issues you face—from life-altering questions and events to day-to-day concerns. Start the conversation. Make the call today.