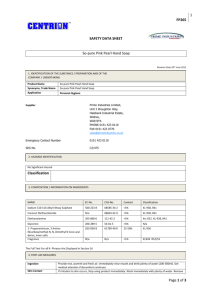
Wrightington, Wigan and Leigh NHS Trust
advertisement

St. Helens and Knowsley Hospitals NHS Trust Cancer & Palliative Care Service Directory Fourth Edition – April 2007 Produced by Cancer Services Version Four April 2007 NHS CONTENTS 1. INTRODUCTION .................................................................................... 4 2. CANCER MANAGEMENT TEAM .......................................................... 5 2.1 SUSPECTED CANCER REFERRALS .................................................... 6 2.2 MDT POLICY ........................................................................................... 7 2.2 MDT POLICY ........................................................................................... 8 2.3 SERIOUS DIAGNOSIS FAX .................................................................. 19 3 ONCOLOGY ........................................................................................ 21 3.1 LILAC CENTRE ..................................................................................... 21 3.2 CLINICAL TRIALS TEAM ...................................................................... 23 4. SITE SPECIFIC PATIENT SERVICES................................................. 24 4.1 CANCER SERVICE – Breast ................................................................ 24 4.2 CANCER SERVICE – Colorectal .......................................................... 26 4.3 CANCER SERVICE – Gynaecology ..................................................... 28 4.4 CANCER SERVICE – Haematology ..................................................... 30 4.5 CANCER SERVICE – Head & Neck...................................................... 31 4.6 CANCER SERVICE – Lung................................................................... 32 4.7 CANCER SERVICE – Skin .................................................................... 34 4.8 CANCER SERVICE – Upper Gastrointestinal ..................................... 35 4.9 CANCER SERVICE – Urology .............................................................. 37 5. PALLIATIVE CARE ............................................................................. 39 5.1 PALLIATIVE CARE - Hospital Specialist Palliative Care Team ......... 39 5.2 PALLIATIVE CARE - Willowbrook Hospice ........................................ 47 5.3 PALLIATIVE CARE - Macmillan Clinical Nurse Specialist Palliative Care - Community ......................................................................................... 51 Produced by Cancer Services - Version Four (April 2007) -2- 5.5 PALLIATIVE CARE - INTEGRATED PALLIATIVE HOME CARE TEAM – HENRIETTA PROJECT ............................................................................. 55 6.0 EXTENDED SERVICES ....................................................................... 57 6.1 EXTENDED SERVICES - HOSPITAL BASED PAIN TEAM ............... 57 6.2 EXTENDED SERVICES - Chaplain/Pastoral Care............................... 59 6.3 EXTENDED SERVICES - Department Of Nutrition and Dietetics ...... 61 6.4 EXTENDED SERVICES - The Speech & Language Therapy Service 68 6.5 EXTENDED SERVICES – SUPPORT Smoking Cessation ................. 69 6.6 EXTENDED SERVICES – ICCP (Integrated Cancer Care Programme) 72 7. SUPPORT GROUPS............................................................................ 74 7.1 SUPPORT GROUPS - Local Support Groups/Services ..................... 74 7.2 SUPPORT GROUPS - Local Bereavement Support ........................... 78 7.3 SUPPORT GROUPS - National Support - General ............................. 79 7.4 SUPPORT GROUP - National Support – Site-Specific....................... 84 8. AMENDMENT FORM........................................................................... 92 Produced by Cancer Services - Version Four (April 2007) -3- 1. INTRODUCTION Welcome to the fourth edition of St Helens & Knowsley Hospitals NHS Trust, Cancer & Palliative Care Service Directory. This Directory has been produced to build on existing communication links between primary and secondary care. The Directory contains vital information about the multidisciplinary teams responsible for cancer care at St Helens & Knowsley Hospitals. There are seven sections, with the first five giving details of cancer and palliative care services at St Helens & Knowsley Hospitals, Willowbrook Hospice and Primary Care. The sixth section covers a range of extended services, which may be accessed by cancer or palliative care patients. The last gives details of relevant local and national support groups. Inevitably teams change and Directory details become dated and inaccurate. To maintain what we believe is a crucial dialogue between health professionals, the directory will be subject to quarterly amendment to maintain its accuracy, future editions will be available electronically on our Intranet site: nww.sthkhealth.nhs.uk/cancer services. To ensure subsequent editions of the Directory are complete, please inform me of any additions or amendments directly. Your assistance is appreciated. Anita Corrigan Lead Nurse/Manager - Cancer Services 0151 430 1055 Anita.Corrigan@sthk.nhs.uk Produced by Cancer Services - Version Four (April 2007) -4- 2. CANCER MANAGEMENT TEAM There is a lead team within St Helens & Knowsley Hospitals, comprising of a lead clinician and lead nurse/manager, who work in close collaboration to deliver on the strategic and operational agenda for cancer services at a local level. Lead Clinician The lead clinician is responsible for the clinical organisation, development and delivery of cancer care across the cancer unit. The lead clinician is a representative voice for medical colleagues relating to all aspects of cancer service provision. Communication is a fundamental part of this role. Contact details: Dr Rani Thind Tel: 0151 430 1265 Rani.Thind@sthk.nhs.uk Lead Nurse The lead nurse is responsible for providing leadership and direction for all nurses involved in cancer care, to develop cancer-nursing practice in line with local, regional and national priorities. The aim is to facilitate a comprehensive and integrated approach to cancer service delivery and improve the patient’s experience throughout their cancer journey. Contact details: Anita Corrigan Tel: 0151 430 1055 Anita.Corrigan@sthk.nhs.uk Lead Manager The lead manager works closely with individual cancer teams and key stakeholders to develop cancer teams and services to meet national cancer standards and the targets set out in the National Cancer Plan. Contact details: Anita Corrigan Tel: 0151 430 1055 Anita.Corrigan@sthk.nhs.uk Produced by Cancer Services - Version Four (April 2007) -5- 2.1 SUSPECTED CANCER REFERRALS St Helens & Knowsley Hospitals NHS Trust Urgent Suspicious Cancer Referral Pro-forma Patient Details GP Practice Details (stamp) Surname: Practice Name: Address: First Name: Age/DOB: Postcode: Contact Number: Evening Telephone: Postcode: Telephone: Fax: Email: Referring GP: Mobile: New NHS number: Decision to refer date: Address: / / Hospital number (if known): First language: Interpreter required? Y / N Please tick the Speciality for which you are requesting a Two-week wait appointment: 1Gynaecology 2Lung 3Haematology (x-ray to be done prior to referral) 11Skin GI 8Breast 9Brain 10Lower GI 5Urology 6Testicular 7Upper 4Head & Neck 12Sarcoma State clinical reason for suspicion of cancer - See Referral Guidelines – Include any investigation results and any other relevant information. FAX THIS FORM WITHIN 24 HOURS OF YOUR DECISION TO REFER TO: UROLOGICAL 0151 430 1901 GYNAECOLOGICAL 0151 430 1043 ENDOSCOPY 0151 430 1892 ALL OTHER CANCER REFERRALS 0151 430 1629 Produced by Cancer Services - Version Four (April 2007) -6- 1GYNAECOLOGY-Urgent 5UROLOGICAL Referral Pelvic mass not obviously fibroids or pregnancy Post menopausal bleeding not on HRT Suspicious cervical lesion Persistent post-coital bleeding Smear suggesting malignancy 2LUNG-Urgent Referral to a Chest Physician: Chest x-ray suggestive or suspicious of lung cancer (including pleural effusion and slowly resolving consolidation) Persistent haemoptysis in smokers/ex-smokers over 40 years of age Sign of superior vena caval obstruction (swelling of face/neck with fixed elevation of jugular venous pressure) Stridor (consider emergency referral) 3HAEMATOLOGICAL – urgent referral Blood count/film reported as suggestive of acute leukaemia or chronic myeloid leukaemia. Lymphadenopathy (> 1cm) persisting for 6 weeks NB. Cervical lymphadenopathy/ unresolving neck masses persisting for > =3weeks, referral to the Head & Neck team is recommended Hepatosplenomegaly Bone pain associated with anaemia and a significantly raised ESR (or plasma viscosity) Bone x-rays reported as being suggestive of myeloma Constellations of 3 or more of the following symptoms (+/-fatigue) night sweats weight loss itching breathlessness bruising recurrent infections bone pain. 4Head & Neck – urgent referral >=6 weeks hoarseness any 1 of the following lasting >=3 weeks: ulceration of mucosa, oral swellings, dysphagia, unressolved neck mass uniltareal nasal obstruction with purulent discharge unexplained tooth mobility without peridontal disease cranial neuropathies orbital masses The level of suspicion is further increased if the patient is a heavy smoker or heavy alcohol drinker and is aged over 45years and male. Other forms of tobacco use (chewing Betel, Gutkha, Pan) should also arouse suspicion - Urgent Referral Macroscopic haematuria in adults Microscopic haematuria in adults over 50 yrs – excl UTI Swelling in the body of the testis – refer to consultant Solid renal masses found on imaging An elevated age specific PSA in men with a ten year life expectancy A high PSA (>20ng/ml) in men with a clinically malignant prostate or bone pain Any suspected penile cancer Recommended that PSA test, in aysmptomatic men should only be performed after full counselling and provision of written information. 6UPPER GI-Urgent Referral any age Dysphagia Dyspepsia with >=1 of the following alarm symptoms: Weight loss, proven anaemia vomiting >55 years Dyspepsia >=1 of the following "high risk" features: Onset of dyspepsia less than one year ago Continuous symptoms since onset Dyspepsia combined with >=1 of the following risk factors: Family history of upper GI cancer in more than 2 first degree relatives Barrett's oesophagus Pernicious anaemia Peptic ulcer surgery over 20 years ago Known dysplasia, atrophic gastritis, intestinal metaplasia Jaundice Upper abdominal mass tumours – urgent referral Subacute progressive neurological deficit developing over days to weeks eg weakness, sensory loss, dysphasia, ataxia. New onset seizures characterised by >=1 of the following: focal seizures, prolonged post ictal focal deficit (>1hr), status epilepticus, associated interictal focal deficit. Headache, vomiting & papilloedema Cranial nerve palsy eg diplopia, visual failure incl. Optician defined visual field loss, unilateral sensorineural deafness. Consider urgent referral for: recent onset non-migrainous headaches, present for >=1 month, accompanied by features of raised intra cranial pressure eg woken by headache; vomiting; drowsiness. (Exclude depression and somatisation disorder – brain tumour unlikely) 9LOWER GI - Signs & Symptoms of predictive value of bowel cancer • • • • • • • 7BREAST - Urgent Referrals Patients with a discrete lump in the appropriate age group (eg age > 30) Signs which are highly suggestive of cancer such as: ulceration, skin nodule, skin distortion, nipple eczema, recent nipple retraction or distortion (< 3 months 8Brain Produced by Cancer Services - Version Four (April 2007) -7- • Any age persistent increase in frequency of bowel function or looseness of stools for 6 weeks definite palpable right sided iliac fossa mass definite palpable rectal tumour suspicious barium enema Aged 40> bleeding persistently without peri-anal symptoms (eg soreness, discomfort, itching, lumps, prolapse, pain) dark blood mixed with stools unexplained iron deficiency anaemia (Hb <11g/dl in men or <10g/dl in postmenopausal women) abdominal pain only if severe, colicky and in association with weight loss or decreased appetite 10SKIN -Urgent Referral Melanoma - Pigmented lesion which have >=1 of the following features: Growing in size Changing shape Irregular outline Change in colour Mixed colour Itch/ bleeding Inflammation NB Melanomas are usually 5mm or greater at the time of diagnosis, smaller lesions may appear in early melanoma. Squamous Cell Carcinoma (SCC) Slow growing, non-healing lesions with a significant induration on palpation with documented expansion over 1-2 months. Patients diagnosed SCC from a biopsy undertaken in general practice immuno suppressed patients following organ transplant have a high incidence of SCC which can be unusually aggressive and metastasize . Strongly recommend referring these patients via two week rule. Characteristics of SCC Evidence of chronic skin damage eg solar keratosis/old burn scar Crusting/non healing lesion Documented expansion Inflammatory response 11Sarcoma – urgent referral Soft tissue mass with >=1 of the following: Size > 5 cms, painful, increasing in size, deep to fascia, recurrence after previous excision. Radiological suspicion of a primary bone tumour based on evidence of bone destruction, new bone formation, soft tissue swelling and periosteal elevation. 2.2 MDT POLICY 1.0 Introduction 1.1 As a prerequisite for Cancer Peer Review, the Trust is required to have an agreed operational policy in place for each cancer multidisciplinary team (MDT). The policy aims to ensure that the MDT is an integral part of the cancer patient’s management. 1.2 Following consultation with all MDT Lead Clinicians (as documented below), the policy was approved on 14/03/05 at the Trust Cancer Committee Mr G. Cawdell Lead Clinician – Gynaecology Miss L. Chagla Lead Clinician – Breast Mr R. Green Lead Clinician – Skin Dr J. Hendry Lead Clinician – Lung Mr I. Khan Lead Clinician – Upper GI Mr R. Kiff Lead Clinician – Colorectal Dr C. Littlewood Lead Clinician – Palliative Care Mr A. Massey Lead Clinician – Urology Dr G. Satchi Lead Clinician – Haematology 2.0 Scope of Policy 2.1 To describe the process and requirements of an effective MDT, ensuring All patients with a new diagnosis of cancer have their treatment plan discussed by the appropriate MDT Prompt effective decision making, to prevent delays in the patients journey Teams comply with the site-specific quality measures identified within the Cancer Services Manual of Cancer Standards 2004. This is a generic document that applies to all cancer MDT’s in the Trust. It is intended for adjustment by the various MDT’s to reflect their local practices. 3.0 Terminology and definitions 3.1 The Cancer Multidisciplinary Team (MDT) is defined as a group of staff from different health care disciplines, who meet together at a given time (whether physically in one place, or by video/teleconferencing) to discuss a given patient and who are each able to contribute independently to the diagnostic and treatment decisions about the patient. Produced by Cancer Services - Version Four (April 2007) -8- 3.2 The (2004) Cancer Services Standards define the objectives of an MDT as follows: To ensure that designated specialists work effectively together in teams such that decisions regarding all aspects of diagnosis, treatment and care of individual patients and decisions regarding the team’s operational policies are multidisciplinary decisions. To ensure that care is given according to recognised guidelines (including guidelines for onward referrals) with appropriate information being collected to inform clinical decision making and to support clinical governance/audit. To ensure that mechanisms are in place to support entry of eligible patients into clinical trials, subject to patients giving fully informed consent. 4.0 MDT Constitution 4.1 There should be a single named lead clinician for the named MDT who should then be a core team member, agreed by the lead clinician of the Trust. 4.2 The lead clinician of the MDT should have agreed the responsibilities of the position with the lead clinician of the Trust. (Appendix 1) 4.3 The MDT should be listed as part of the services of a named locality of the network. 4.4 The core membership of an MDT will vary between teams and must be adjusted to reflect Cancer Services Standards, NICE guidance and local practice. Membership will generally include: 4.5 MDT Lead Clinician Consultant medically qualified core member(s) other than in imaging and histopathology. Oncologist(s). Clinical Nurse Specialist/nurse representative Radiologist Histopathologist Palliative Care representative MDT Co-ordinator Any additional members at the discretion of the MDT Lead. A core team member will be nominated as having specific responsibility for users' issues and information for patients and carers. The MDT should agree cover arrangements for each core member, agreed by the lead clinician of the MDT Produced by Cancer Services - Version Four (April 2007) -9- 4.6 The core imaging specialist member(s) of the MDT should regularly report on imaging of the primary cancer site or sites of the MDT. 4.7 The MDT should have at least one core nurse member who should have enrolled in, or be undertaking, or have successfully completed, a programme of study in their specialist area of nursing practice which has been accredited for at least 20 level III CAT points. 4.8 The MDT should have at least one core nurse member who should have enrolled in, be undertaking, or have successfully completed a course/module in communication skills, which is accredited for CAT points. This may be either standalone or as part of specialist programme. 4.9 The lead clinician and the core nurse member/s will have agreed a list of responsibilities. (Appendix 2) 4.10 If applicable, the MDT lead clinician will agree the names of members of the extended team for named roles in the team, if they are not already offered as core team members. 5.0 MDT Terms of Reference 5.1 Meetings should take place as directed by the Cancer Services Standards, or more frequently dependant on workload. As a minimum, fortnightly meetings should take place to ensure the patient’s journey is not adversely affected. A record of core members' attendance will be maintained. 5.2 Core members or their arranged "cover" should attend a minimum of 51% of the meetings. 5.3 The core MDT, at their regular meetings, should agree and record individual patient's treatment plans. A record should be made of the treatment plan. The record should include: The identity of patients discussed. The multidisciplinary treatment planning decision (i.e. to which modality(s) of treatment - surgery, radiotherapy, chemotherapy, hormone therapy or supportive care or combinations of the same, they are to be referred for consideration). 5.4 For patients requiring a treatment planning decision before the next scheduled meeting, the consultant lead will discuss the patient with the relevant core/extended team member (i.e. consultant colleague, oncologist , palliative care) and jointly agree a management plan. The agreed management plan will be documented in the case notes. All patients will be discussed retrospectively at the next scheduled meeting. 5.5 Besides the regular meetings to discuss individual patients, the team should meet at least annually to agree the following: Produced by Cancer Services - Version Four (April 2007) - 10 - Local protocols and guidelines for practice Adoption of national/network guidelines Review MDT compliance with Cancer Services Standards Agree and ensure representation on the relevant CNG, with regular feedback to the team. 6.0 MDT Co-ordination 6.1 The list of patients to be discussed at a forthcoming meeting is held by the MDT Co-ordinator. Any member of the core or extended MDT may add patients to the list, although this should be discussed with the sitespecific surgeon/physician beforehand to ensure responsibility for any clinical decision made by the MDT is agreed. 6.2 The MDT Co-ordinators frequently review all pathology reports to identify cancer patients. If a patient is identified via this route the MDT Co-ordinator has the authority to add these patients to MDT lists. 6.3 The cut-off time for adding patients to the list is as follows: For a morning meeting - cut-off midday previous working day For a lunchtime meeting – cut-off close of day previous working day This ensures the MDT Co-ordinators have time to find all notes and xray films before a meeting, and for these to be reviewed by MDT members. The Core Team Radiologist and Histopathologist will be informed of those patients on the list, in order to review films/slides in advance of the MDT meeting. 6.4 For patients added to the list after the cut-off time, notes and films must be provided by the ‘adding’ clinician. 6.5 The chair of the meeting will ensure discussions are focused, ensuring all core members of the MDT are able to contribute. 6.6 Following MDT discussion, a core team member will record the management decision be in the patient’s case notes. 7.0 Primary Care Feedback 7.1 The MDT will inform the patient's general practitioner (GP) after a patient is given a diagnosis of cancer. The agreed generic proforma will be completed and faxed to the practice by the end of the following working day. The MDT will audit this process on an annual basis. 7.2 The MDT will provide information to referring general practitioners on the appropriateness of urgent suspected cancer GP referrals. Produced by Cancer Services - Version Four (April 2007) - 11 - 8.0 Patient experience 8.1 Each MDT will identify a single named key worker for each individual patient receiving treatment/care directly from the team. The name of the current key worker will recorded in the patient's case notes. The responsibility for ensuring that the key worker is identified should be that of the nurse MDT member(s). (Appendix 2 & 3) 8.2 The key worker for each individual patient will ensure that the patients and/or carers receive written contact information to access the MDT to discuss problems or concerns. 8.3 The MDT will offer patients the opportunity of a permanent record or summary of at least a consultation between the patient and the doctor at which the treatment options of their diagnosis were discussed. 8.4 The MDT will undertake an annual survey of its patients' experience of the services offered by the team. The survey should at least ascertain whether patients were offered: A key worker. The MDT's information for patients (written or otherwise). The opportunity of a permanent record or summary of a consultation at which their treatment options were discussed. The survey results will be presented and discussed at an MDT meeting, with at least one action point arising from the survey agreed and implemented. 8.5 The MDT will provide written material for patients and carers which includes: Information specific to that MDT about local provision of the services offering the treatment for that cancer site. Information about patient self-help groups if available and complying with the network quality criteria. Information about the services offering psychological, social and spiritual/cultural support, if available. Information specific to the MDT's cancer site or group of cancers about the disease and its treatment options. 8.6 There should be a checklist in each patient's case notes addressing whether the patient has been offered: A key worker. The MDT's information for patients (written or other formats). The opportunity of a permanent record or summary of a consultation at which their treatment options were discussed. 9.0 Network requirements 9.1 The MDT should send a team member as a representative to at least two thirds of the site-specific clinical network group (CNG) meetings. Produced by Cancer Services - Version Four (April 2007) - 12 - The representative should feedback CNG discussions to the MDT on a regular basis. 9.2 The MDT should abide by the agreed specified network-wide clinical guidelines for the cancer site. 9.3 The MDT should abide by the agreed network-wide referral guidelines 9.4 The MDT should abide by the agreed imaging guidelines for the diagnosis and assessment of that cancer site. The guidelines should address: Imaging modalities. Their specific indications. 9.5 The MDT should abide by the agreed pathology guidelines for the diagnosis and assessment of that cancer site. The guidelines should address: Laboratory and histopathology/histochemical investigations. Their specific indications. 9.6 The MDT should collect the minimum dataset (MDS), as agreed by the site-specific clinical network group (CNG). 9.7 The MDT should participate in at least one network-wide audit project. The MDT should present the results of a completed network-wide audit project to the site-specific clinical network group (CNG) 9.8 The MDT should abide by the agreed network approved list of clinical trials. 10.0 Data Collection 10.1 The MDT should have started to record the MDS in an electronically retrievable form. 10.2 Measured over the complete calendar year prior to the peer review visit, the MDT should ensure that the hospital's number of separate patient returns to the cancer registry for the MDT's cancer site(s) should be at least 95% of the hospital's 'average' return. 10.3 Measured over the complete calendar year prior to the peer review visit, the MDT should ensure that the hospital's number of separate patient returns to the cancer registry for the cancer site(s) of the team should be at least 95% of the new cancer patients discussed by the team in the same period. 10.4 The Cancer Support Team will provide each MDT with a monthly report identifying pre-defined data items including Cancer Waiting Times Performance. Produced by Cancer Services - Version Four (April 2007) - 13 - 11.0 Service Improvement 11.1 The lead clinician of the MDT should nominate one of the members of the core or extended team as the person responsible for ensuring that service improvement is integrated into the functions of the MDT. 11.2 The MDT should carry out process mapping covering the key stages of their patients' journey i.e.: a) From the receipt of the referral of a new patient to their point of referral on for each of the possible options for first definitive treatment; and: b) In the case of a surgical, first definitive treatment, to the point of admission for surgery. From the completed process mapping the MDT should produce a report containing an action plan (AP) for service improvement, which addresses patient waiting times. The report including the AP should be agreed by the MDT lead clinician, the service improvement lead of the CNG and the network service improvement lead. From the AP, at least one action point for service improvement addressing patient waiting times should have been agreed with the service improvement lead for the CNG and the network service improvement lead, as being of first priority for implementation, and should then have been implemented. Data, addressing patient waiting times, from the relevant part of the patient journey should have been collected before and after implementation, and compared. Following receipt of the MDT's process mapping report, the network service improvement lead should decide whether capacity/demand study is required for any part of the patient journey. If this is required, the MDT should have completed the required study and the results used as a basis for part of the service improvement AP. 11.4 The MDT will offer patients ‘booking’ at three key stages of their cancer journey: Booking Two-week wait referrals should be able to choose to prebook their appointment. New patients who are suspected of having cancer should be able to choose and pre-book the date of their first diagnostic test. Patients who require an elective admission/outpatient treatment for first treatment should be able to choose and pre-book their admission date. 12.0 Clinical Governance 12.1 It is a national requirement that an MDT discusses all patients with a new diagnosis of a cancer. Each MDT must therefore ensure the team discusses all patients within their remit at least once, and that treatment decisions are clearly recorded in the patients notes. Produced by Cancer Services - Version Four (April 2007) - 14 - Appendix 1 – Role and Responsibilities of MDT Lead Clinician Role: Ensure that all objectives of MDT working (as laid out in Manual of Cancer Service Standards, 2004) are met Ensure that MDT members work effectively together, such that decisions regarding all aspects of treatment/care of individual patients and decisions regarding the team's operational policies are multidisciplinary decisions Ensure that care is given according to recognised guidelines (including guidelines for onward referrals) with appropriate information being collected to inform clinical decision-making and to support clinical governance/audit. Ensure mechanisms are in place to support entry if eligible patients into clinical trials, subject to patients giving fully informed consent. Responsibilities: Overall responsibility for ensuring that MDT meeting and team compliance meet Peer Review Quality Measures. Ensure attendance levels of core team members are maintained, in line with Quality Measures. Ensure the target of 100% of cancer patients discussed at MDT is met. Provide link to Network Site Specific Group (NSSG), either by attendance at meetings or by nominating another team member to attend. Engage in the work of the NSSG in developing cancer services, policies and standards Lead on, or nominate radiology lead for service improvement. Organise and chair MDT annual team meeting examining functioning of team and reviewing operational policies, and collate any activities that are requires to ensure optimal functioning of the team (e.g. training for team members). Ensure MDT’s activities are audited and results documented.. Ensure that the outcomes of the meeting are clearly recorded and clinically validated and that appropriate data collection is supported. Ensure target for communicating MDT outcomes to primary care is met. Meet regularly with Cancer Management Team, colleagues from Trust and locality, participating in discussion on trust-wide Cancer Services and Strategy. Signed ……… Date ………….. MDT Lead Clinician Clinician Signed ……...………………….. Date ………………. Dr Thind, Cancer Services Lead Produced by Cancer Services - Version Four (April 2007) - 15 - Appendix 2 – Role and Responsibilities of MDT Core Nurse Member/s Role: Contribute to the MDT’s compliance with the quality measures for site-specific teams (as laid out in Manual of Cancer Service Standards, 2004) are met. Contribute to effective MDT working, such that decisions regarding all aspects of diagnosis, treatment and care of individual patients and decisions regarding the team's operational policies are multidisciplinary decisions. Ensure that care is given according to recognised guidelines (including guidelines for onward referrals) with appropriate information being collected to inform clinical decision-making and to support clinical governance/audit. Responsibilities Contributing to the MDT discussion and patient assessment/care planning decision of the team at their regular meeting. Ensuring the at MDT meeting and team meet Peer Review Quality Measures. Providing expert nursing advice and support to other health professionals in the nurse’s specialist area of practice Utilising research in the nurse’s specialist area of practice. Involvement in clinical audit Contributing to the management of the service Specific responsibility for user issues and information for patient and carers Lead on patient communication issues and co-ordination of the patients pathway for patients referred to the team – acting as a key worker or responsible for nominating the key worker for the patient’s dealings with the team. Key Worker Role: To promote clinical continuity for patients Key Worker Responsibilities - To orchestrate assessments to ensure patients’ needs are elicited - Ensuring care plans have been agreed with the patient Ensuring findings from assessments and care plans are communicated to others involved in a patient’s care - Ensuring patients know who to contact when help or advice is needed, whether the ‘key worker’ or other appropriate personnel - Act as an administrative contact (during normal working hours i.e. 09.00-17.00, Monday-Friday) for patients and professionals. The key worker will ensure that patient’s and those providing care are given contact information in writing (i.e. name and telephone number). - Managing transitions of care In circumstances where the Palliative Care Team (HPCT) are involved, there has to be an agreement made between the Site-Specific Clinical Nurse Specialist (SSCNS) and the HPCT member negotiating the' key worker' for that specific episode of care. The individual patient’s current issues and specific problems or concerns need to be taken into account. This will take the form of: Produced by Cancer Services - Version Four (April 2007) - 16 - - Advice from HPCT to SS-CNS on a particular situation, e.g. on symptom control, where the SS-CNS remains the key worker. Joint consultation by HPCT and SS-CNS where, on patient's agreement, SS-CNS continues to be the key worker. Joint consultation by HPCT and SS-CNS where, on patient's agreement, HPCT becomes the key worker. Signed ……………..…………… MDT Lead Clinician Date ………….. Signed ……...………………….. Date ………………. Site Specific – Clinical Nurse Specialist Produced by Cancer Services - Version Four (April 2007) - 17 - Appendix 3 - Clinical Nurse Specialist Protocol Initial contact with a newly diagnosed cancer patient Introduction As a prerequisite for Cancer Peer Review, the Trust is required to have an agreed operational policy in place for each cancer multidisciplinary team (MDT), ensuring each MDT identifies a single named key worker for each individual patient receiving treatment/care directly from the team. The responsibility for ensuring that the key worker is identified should be that of the nurse MDT member(s). Scope of Protocol To describe the role of the site-specific nurse specialist on Initial contact with a newly diagnosed cancer patient Terminology and Definitions For St Helens & Knowsley Hospitals, the site-specific clinical nurse specialist will perform the role of the ‘key worker’. The Clinical Nurse Specialist title will be used rather than ‘key worker’. Protocol Initial contact will be made at time of diagnosis in clinic/ward setting or by the end of the next working day by telephone. In the absence of the Nurse Specialist, it is the responsibility of the clinician informing the patient of the diagnosis to provide the Nurse Specialist and patient with contact details. On contact the patient and/or carer will receive the Nurse Specialist’s name, contact details and hours of work. The patient and/or carer will receive written/verbal information regarding the role of the Nurse Specialist i.e. - To orchestrate assessments to ensure patients’ needs are elicited - Ensuring care plans have been agreed with the patient - Ensuring findings from assessments and care plans are communicated to others involved in a patient’s care - Ensuring patients know who to contact when help or advice is needed, whether the ‘key worker’ or other appropriate personnel* - Act as an administrative contact (during normal working hours i.e. 09.0017.00, Monday-Friday) for patients and professionals. The key worker will ensure that patient’s and those providing care are given contact information in writing (i.e. name and telephone number). - Managing transitions of care The Nurse Specialist will provide written material for patients and carers which includes: - Information specific to that MDT about local provision of the services offering the treatment for that cancer site. - Information about patient self-help groups if available and complying with the network quality criteria. - Information about the services offering psychological, social and spiritual/cultural support, if available. - Information specific to the MDT's cancer site or group of cancers about the disease and its treatment options. Produced by Cancer Services - Version Four (April 2007) - 18 - 2.3 SERIOUS DIAGNOSIS FAX PRACTICE PROTOCOL SERIOUS DIAGNOSIS FAX BACK Introduction During the baseline assessment of cancer services in primary care throughout St Helens PCT, it was highlighted that patients were attending surgery following a cancer diagnosis before the GP has been informed of that diagnosis. Developments are being progressed in secondary care to provide GPs with this communication within 24 hours of diagnosis. PROTOCOL This protocol is to be used when a serious diagnosis fax is received within the practice. A named member of the reception staff for each practice should be responsible for dealing with the serious diagnosis fax. A second named member of the Primary Health Care Trust should be identified to cover for holidays and sickness absence etc. The named member of staff should inform the relevant GPs of the diagnosis and treatment plan (registered GP and/or the GP the patient normally sees). Either by showing them the serious diagnosis fax. By informing the GP by telephone. If the GP is unavailable due to sickness absence or holiday then the Locum and/or principle GP of the practice should be informed of the diagnosis and treatment plan. The serious diagnosis fax (or copy) should be placed within the patient’s record/notes. The patient’s record/notes should be Read coded with the appropriate diagnosis (Read codes to be provided). Produced by Cancer Services - Version Four (April 2007) - 19 - NHS St. Helens and Knowsley Hospitals NHS Trust Cancer Diagnosis – 24 hour communication Speciality Dear Doctor ………………………………………… RE: Date …………………… Addressograph Your patient was seen in clinic today by:………………………………………………………. Diagnosis …………………………………………………………………………………………. The patient has been told:……………….……………………………………………………… ………………..…………………………………………………………………………………….. The plan of treatment is as follows: ……………………………………………………………. ……………………………………………………………………………………………………… New medication commenced: ………………………………………………………………….. Investigation / procedures planned ……………………………………………………………. ……………………………………………………………………………………………………… ……………………………………………………………………………………………………… Additional information (ie referred to palliative care …………………………………………………………………………………………………………………… Appointment details ……………………………………………………………………………… A detailed letter will be sent to you in the near future. However, if you have any queries in the meantime please do not hesitate to contact me. You will need to update your cancer register with this information. Yours Sincerely, (Name Telephone Number Bleep Number) Whiston Hospital, Warrington Road, Prescot, Merseyside, L35 5DR Produced by Cancer Services - Version Four (April 2007) - 20 - 3 ONCOLOGY 3.1 LILAC CENTRE St Helens & Knowsley Hospitals provides a local outpatient chemotherapy service for haematology and oncology patients. In addition to elective chemotherapy the Unit operates an open door access policy for known haematology/oncology patients, with emergency assessment, telephone advice and triage. The Unit also facilitates out-patients procedures including: Bone marrow biopsy Hickman/PICC line placement and care Pleural/ascitic tap Whole unit venesection Intravenous infusions including: - iron - immunoglobulin - bisphosphonates - monoclonal antibody - blood and platelet transfusions. The Lilac Nurses are qualified and trained to care for patients with cancer. They aim to make treatment as tolerable as possible and to minimise side effects associated with chemotherapy treatment. They work closely with all team members, to help provide continuity of care. Based within the Lilac Centre is a counselling and complimentary therapy service. This service is open to patients and carers during and post treatment. Both staff and patients can make referrals to the service and all therapies are conducted in a safe and confidential environment. Produced by Cancer Services - Version Four (April 2007) - 21 - Team Members Role Barbara Jost Ruth Jackson Karen Pocock Holly Donaghy Philip Walker Maureen Scotton Janet Davies Deborah Kilshaw Janice Ashton Gill Levey Shirlie Deveney Dawn Porter Unit Manager Chemotherapy Sister Chemotherapy Nurse Chemotherapy Nurse Chemotherapy Nurse Chemotherapy Nurse Receptionist Receptionist Health Care Assistant Counselling Manager Assistant Counselling Manager Research Practitioner Jeanette Ribton Oncology Nurse Specialist Raphael Kawonga Haematology Staff Grade Dr M Abbas Oncology Staff Grade Peter Smith Laura Evans Oncology/Haematology Pharmacist Oncology Dietician Elaine Smith Denise Ambage Lisa Ryan Sandra Clegg Haematology Secretary Haematology Secretary Haematology Secretary Oncology Secretary Contact Details Monday to Friday 9–5 0151 430 1687 0151 430 1687 0151 430 1687 0151 430 1687 0151 430 1687 0151 430 1687 0151 430 1614 0151 430 1614 0151 430 1687 0151 430 1687 0151 430 1687 0151 430 1147 Bleep 1148 0151 430 2269 Bleep 0014 0151 430 1825 Bleep 1826 0151 430 1995 Bleep 0227 0151 430 1514 Bleep 1514 0151 430 1201 Bleep 0208 0151 430 1825 0151 430 1825 0151 430 1825 0151 430 1910 OUT OF HOURS CONTACT INFORMATION Out-patient Advice Ward G5 – 0151 430 1560 In-patient Advice Surgical/ Medical On Call Team. Produced by Cancer Services - Version Four (April 2007) - 22 - 3.2 CLINICAL TRIALS TEAM Team Members Role Dr E Marshall Jenny Almond Dawn Porter Consultant Oncologist Merseyside & Cheshire Cancer Research Network Manager Research Practitioner Sarah Simpkin Clinical Trials Nurse Michelle Harvey Jeanette Ribton Clinical Trials Data Clerk Oncology Nurse Specialist Produced by Cancer Services - Version Four (April 2007) - 23 - Contact Details Monday to Friday 9–5 0151 430 1910 0151 482 7804 0151 430 1147 Bleep 1148 0151 430 1147 Bleep 1147 0151 430 1147 0151 430 2269 Bleep 0014 4. SITE SPECIFIC PATIENT SERVICES 4.1 CANCER SERVICE – Breast Core Multidisciplinary Team Members Role Miss L. Chagla Mr R. Audiso Lead Consultant Consultant Breast Surgeon Consultant Radiologist Dr S. Desmond Dr O. Harris Dr E. Gradwell Dr S. Kelly Dr H Innes Dr R Sripadam Consultant Radiologist Consultant Pathologist Consultant Pathologist Clinical Oncologist Sue McNicholas Breast Care Specialist Nurse Breast Care Specialist Nurse Breast Care Nurse MDT Co-ordinator Chris Bebb Louisa Mahon Jill Atherton Extended Multidisciplinary Team Member Colette Murray Chris Jonkers Rob Rosser Mr K. Graham Mr R. Alvi Dr Lynn Greenhough (Alder Hey Hospital) Marie Curie centre Mr A. Ray Dr R. Thind Dr M. Pinto Dr N. Hasan Sarah Simpkin Nina Agnew Contact Details Monday to Friday 9-5 0151 430 1607 0151 430 1079 0151 426 1600 Ex2491 0151 430 1185 0151 430 1827 0151 430 1839 Clatterbridge Centre for Oncology 0151 334 4000 0151 430 1908 0151 430 1908 0151 430 1908 0151 430 1061 Role Contact Details Monday to Friday 9-5 Palliative Care Cancer Nurse Specialist Breast radiographer Clinical Psychologist Consultant Plastic Surgeon Consultant Plastic Surgeon Clinical genetic/genetics counsellor 0151 430 1953 Physiotherapist/ Lymphoedema Associate Specialist Consultant Radiologist Consultant Pathologist Consultant Pathologist Trials Nurse Warrington Screening Produced by Cancer Services - Version Four (April 2007) - 24 - 0151 430 1185 0151 430 1654 0151 430 1262 0151 430 1401 0151 430 1528 0151 430 1265 0151 430 1731 0151 430 1190 0151 430 1147 01925 230923 OUT OF HOURS CONTACT INFORMATION Out-patient Advice Via GP/NHS Direct. If urgent local A&E Department. G5 Ward if Chemotherapy related. In-patient Advice Ward H4 or via Surgical On Call Team. G5 Ward if Chemotherapy related. Non-urgent Advice Breast Care Nurses Answer Phone Service. OUTPATIENT CLINICS Consultant Clinic Type Day Site Miss Chagla Breast New patients Wednesday AM Burney Breast Unit Miss Chagla Breast Revisits Wednesday PM Burney Breast Unit Mr Audisio Breast New patients Tuesday PM Burney Breast Unit Mr Audisio Breast Revisits & Thursday PM Burney Breast new non-urgent Unit Mr Audisio Breast Revisits Friday AM Stephenson House Mr Ray Breast New patients Monday AM Burney Breast Unit Mr Ray Breast Revisits Friday PM Burney Breast Unit Dr Innes Breast New patients Friday AM Stephenson and Revisits. Wednesday PM House Alternate Monday AM Dr Innes Breast New patients Tuesday PM St Helens and Revisits. OUTPATIENT CLINICS Nurse Clinic Type Specialist Sue McNicholas Breast Prosthetic Or Chris Bebb Clinic BREAST SCREENING/RECALL Dr R. Thind Breast Screening Assessment Dr O. Harris Breast Screening Assessment Dr S. Breast Screening Desmond Assessment Day Site Tuesday PM Whiston Monday AM Whiston Monday AM Whiston Monday AM Whiston Multidisciplinary Team Meeting held, every Friday at 13.00 Venue: Post Graduate Centre Produced by Cancer Services - Version Four (April 2007) - 25 - 4.2 CANCER SERVICE – Colorectal Multidisciplinary Team Members Role Mr R. Kiff Mr D. Maitra Lead Clinician Colorectal Surgeon Mr M. Scott Dr J McLindon Colorectal Surgeon Physician Gastroenterologist Medical Oncologist Clinical Oncologist Dr E Marshall Dr Whitmarsh Dr A. Evans Dr. S. Kelly Helen Carroll Angela Fitzgerald-Smith Paul Ratcliffe Extended Multidisciplinary Team Carolyn Swash Debbie Maddox Laura Evans Tony Ellis Consultant Radiologist Consultant Pathologist Colorectal Nurse Specialist Colorectal Nurse Specialist MDT Co-ordinator Role Stoma Nurse Specialist Specialist Palliative Care CNS Dietitian /nutritionist Clinical geneticist / genetics counsellor Social Worker Contact Details Monday to Friday 9-5 0151 430 1529 0151 426 1600 Ext. 2339 0151 430 1911 0151 430 1281 0151 430 1910 Clatterbridge Centre for Oncology 0151 334 4000 0151 430 1265 0151 430 1839 0151 430 1078 0151 430 1685 0151 430 1061 Contact Details Monday to Friday 9-5 0151 430 1221 0151 430 1274 0151 430 1201 0151 430 1201 OUT OF HOURS CONTACT INFORMATION Out-patient Advice Via GP/NHS Direct. If urgent local A&E Department. G5 Ward if Chemotherapy related. In-patient Advice D2 Ward or Via Surgical On Call Team. G5 Ward if Chemotherapy related. Non-urgent Advice Colorectal Nurse Specialists’ Answer Phone Service. Produced by Cancer Services - Version Four (April 2007) - 26 - OUTPATIENT CLINICS Consultant Clinic Type Mr Kiff Colorectal Cancer/General Mr Kiff Colorectal Cancer/General Mr Maitra Colorectal Cancer/General Mr Maitra Colorectal Cancer/General Mr Scott Colorectal Cancer/General Mr Scott Colorectal Cancer/General Dr Marshall Oncology (Chemotherapy) Dr Marshall Oncology (Chemotherapy) Dr Whitmarsh Oncology (Radiology) ENDOSCOPY SESSIONS Mr Kiff Wednesday PM Mr Maitra Alternate Friday PM Rapid Access Friday PM Day Tuesday AM Site Whiston Friday AM St Helens Wednesday AM Whiston Thursday AM St Helens Thursday AM Whiston Friday PM St Helens Monday AM Whiston Thursday AM Whiston Monday AM Whiston Multidisciplinary Team Meeting held, every Monday at 13.00 Venue: X-ray Seminar Room Produced by Cancer Services - Version Four (April 2007) - 27 - 4.3 CANCER SERVICE – Gynaecology Multidisciplinary Team Members Role Mr G. Cawdell Vacant Lead Clinician Medical Oncologist Dr J Zekri Clinical Oncologist Dr J. Kirwan Gynaecology Oncologist Dr N. Hasan Dr O. Harris Consultant Histopathologist Consultant Radiologist Diane Dearden Clinical Nurse Specialist Jill Atherton MDT Co-ordinator Extended Multidisciplinary Team Colette Murray Role Sarah Simpkin Dr M. Abass Gill Levey Maria Embleton Specialist Palliative Care CNS Clinical Trials Nurse Oncology Staff Grade Psychosocial / psychosexual counsellor Staff Nurse Contact Details Monday to Friday 9-5 0151 430 1663 Clatterbridge Centre for Oncology 0151 334 4000 Clatterbridge Centre for Oncology 0151 334 4000 Women’s Hospital 0151 702 4265 0151 430 1824 0151 426 1600 Ext.2491 0151 426 1600 Ext. 2348 0151 430 1061 Contact details Monday to Friday 9-5 0151 430 1274 0151 430 1147 0151 430 1910 0151 430 1687 0151 426 1600 OUT OF HOURS CONTACT INFORMATION Out-patient Advice Via GP/NHS Direct. If urgent local A&E Department. In-patient Advice H4 or Via Gynaecology On Call Team. G5 if chemotherapy related. Non-urgent Advice Gynaecology Oncology Nurse Answer Phone Service. Produced by Cancer Services - Version Four (April 2007) - 28 - OUTPATIENT CLINICS Clinic Type Gynae-Oncology Rapid Access Pelvic Mass Rapid Access Post-Menopausal Bleeding Rapid Access Post-Menopausal Bleeding Rapid Access Post-Menopausal Bleeding Vulvoscopy Day Alternate Monday AM Wednesday AM Tuesday PM Wednesday PM Friday PM Alternate Wednesday PM *Clinics take place in Maternity and Gynaecology Unit COLPOSCOPY SESSIONS Colposcopy Monday am/p.m. Colposcopy Tuesday am/p.m. Colposcopy Thursday am/p.m. Colposcopy Thursday am/p.m. Colposcopy Friday am/p.m. Site *Whiston *Whiston H1, Whiston H1, Whiston H1, Whiston HI, Whiston H1, Whiston H1, Whiston H1, Whiston H1, Whiston H1, Whiston Multidisciplinary Team Meeting held alternate Mondays at 09.15 prior to Oncology Clinic Venue: X-Ray Seminar Room Produced by Cancer Services - Version Four (April 2007) - 29 - 4.4 CANCER SERVICE – Haematology Multidisciplinary Team Members Role Dr G. Satchi Dr J. Tappin Dr T. Nicholson Dr R. Kawonga Lead Clinician Consultant Haematologist Consultant Haematologist Staff Grade – Haematology Jeanette Ribton Oncology Nurse Specialist Haematology/Oncology Macmillan CancerNurse Specialist Ward Manager – G5 Unit Manager – Lilac Centre Trials Practitioner Angela Madigan Sr. I Kearney Sr. B. Jost Dawn Porter Contact Details Monday to Friday 9-5 0151 430 1887 0151 430 1292 0151 430 1825 0151 426 1600 Ex 2473 Bleep 1826 0151 430 1687 Bleep 0014 0151 430 4111 Bleep 4111 0151 430 1560 0151 430 1687 0151 430 1147 Bleep 1148 OUT OF HOURS CONTACT INFORMATION Out-patient Advice Via Switchboard to Consultant on-call In-patient Advice G5 Ward OUTPATIENT CLINICS Consultant Clinic Type Dr G. Satchi Anticoagulation Dr G. Satchi Anticoagulation Dr G. Satchi Haematology Dr G. Satchi Haematology Dr J. Tappin Haematology Dr J. Tappin Haematology Dr T. Nicholson Haematology Dr T. Nicholson Haematology Day Monday AM Site St Helens Tuesday PM Whiston Wednesday AM Thursday AM Wednesday AM Friday AM Wednesday AM Friday AM Whiston St Helens Whiston Whiston Whiston Whiston Multidisciplinary Team Meeting held weekly on Wednesday at 14.00 Venue: X-ray Seminar Room. Joint MDT with North Cheshire Hospitals 1st Wednesday of the month 15.00 Venue: X-ray Seminar Room. Produced by Cancer Services - Version Four (April 2007) - 30 - 4.5 CANCER SERVICE – Head & Neck Multidisciplinary Team Members Role Mr Nandapalan Consultant Otolaryngologist Consultant Otolaryngologist Consultant Otolaryngologist Medical Oncologist Mr Daud Mr Jones Dr Husband Dr Hasan Consultant Histopathologist Contact Details Monday to Friday 9-5 0151 430 1598 0151 430 1573 0151 529 5248 Clatterbridge Centre for Oncology 0151 334 4000 0151 430 1190 OUT OF HOURS CONTACT INFORMATION Out-patient Advice Via GP/NHS Direct. If urgent local A&E Department. In-patient Advice D2 Ward OUTPATIENT CLINICS Consultant Clinic Type Mr Daud ENT Mr Daud ENT Mr Nandapalan ENT Mr Nandapalan ENT Mr Jones ENT Dr Husband Mr Jones Head & Neck Day Monday AM Friday PM Tuesday AM Thursday PM Tuesday PM 2nd, 4th & 5th Tuesday PM 1st & 3rd Site Whiston Hospital Whiston Hospital Whiston Hospital Whiston Hospital Whiston Hospital Whiston Hospital Multidisciplinary Team Meeting held at University Hospital Aintree Produced by Cancer Services - Version Four (April 2007) - 31 - 4.6 CANCER SERVICE – Lung Multidisciplinary Team Members Role Dr. J. Hendry Dr. P. Stockton Respiratory Physician – Clinical lead for Lung Cancer Respiratory Physician Dr S Twite Respiratory Consultant Joanne Brown Dr. J. Wide Lung Cancer Clinical Nurse Specialist Lung Cancer Clinical Nurse Specialist Lung Cancer Clinical Nurse Specialist Specialist Palliative Care CNS Consultant Radiologist Dr N. Mohsin Consultant Radiologist Dr A. Dar Dr E. Marshall Mr. Shackcloth Dr. Z. Malik Consultant Histopathologist Consultant Oncologist Thoracic Surgeon Consultant Oncologist Lorraine Price MDT Co-ordinator Extended Multidisciplinary Team Members Dr Littlewood Pool member Rob Rosser Jane Shepherd Role Pauline Murphy Carol Dawson Robert Case Willowbrook Hospice Palliative Care physician Social Worker Clinical Psychologist Chaplain/ pastoral care worker Bereavement care worker Contact Details Monday to Friday 9–5 0151 430 1899 0151 426 1600 Ex 2638 0151 426 1600 Ex 2638 0151 430 1367 0151 430 2326 0151 430 2326 0151 430 1274 0151 426 1600 Ex 2485 0151 426 1600 Ex 2485 0151 430 1827 0151 430 1910 0151 228 1616 Clatterbridge Centre for Oncology 0151 334 4000 0151 430 1061 Contact details Monday to Friday 9-5 0151 430 1347 0151 430 1634 0151 430 1657 0151 430 8736 OUT OF HOURS CONTACT INFORMATION Out-patient Advice Via GP/NHS Direct. If urgent local A&E Department. In-patient Advice Ward F2, G16, C1 or Via Medical On Call Team. Non-urgent Advice Lung Cancer Nurse Answer Phone Service. Produced by Cancer Services - Version Four (April 2007) - 32 - OUTPATIENT CLINICS Consultant Clinic Type Dr Hendry Lung Shadow Clinic Dr Stockton Lung Shadow Clinic Dr Marshall Cancer Clinic Dr Marshall Cancer Clinic Mr Soorae Thoracic Surgery Clinic Dr Z Malik Oncologist Radiotherapy Day Thursday am Site Whiston Hospital Thursday am Whiston Hospital Monday am Thursday am 1st and 3rd Tuesday p.m. Thursday am Whiston Hospital Whiston Hospital Whiston Hospital Whiston Hospital BRONCHOSCOPY SESSIONS Alternate Monday p.m. Dr Stockton Tuesday am Dr Ridyard Wednesday p.m. Dr Hendry/Dr Corless H2, Endoscopy Unit H2, Endoscopy Unit H2, Endoscopy Unit Multidisciplinary Team Meeting held every Thursday morning, at 08.30 Venue: Brandreth Suite Pre-thoracic Surgery MDT Meeting alternate Tuesdays, at 14.00. Venue: Hackworh Suite X Ray MDT Wednesday 12.30 – 14.00 Venue: X-Ray Seminar Room Produced by Cancer Services - Version Four (April 2007) - 33 - 4.7 CANCER SERVICE – Skin Multidisciplinary Team Members Mr Green Mr Hancock Dr Curley Dr Herbert Role Dr Marshall Dawn Porter Consultant Oncologist Clinical Trials/Research Practitioner Dermatology Nurse Specialist Dermatology Nurse Specialist Consultant Pathologist Consultant Oncologist Tom Crowe Chris Hunt Dr Gradwell Dr Husband Consultant Plastic Surgeon Consultant Plastic Surgeon Consultant Dermatologist Consultant Radiologist Contact Details Monday to Friday 0151 430 1664 0151 430 1044 0151 430 1507 0151 426 1600 Ext. 2265 0151 430 1910 0151 430 1147 Bleep 1148 0151 430 1953 0151 430 1482 0151 430 1827 Clatterbridge Centre for Oncology 0151 334 4000 OUT OF HOURS CONTACT INFORMATION Out-patient Advice Via GP/NHS Direct. If urgent local A&E Department. In-patient Advice Holbrook Unit Non-urgent Advice Dermatology Nurse Specialist Answer Phone Service OUTPATIENT CLINICS Consultant Clinic Type Mr Green *Skin Cancer Dr Curley Skin Cancer Dr Marshall Skin Cancer – Oncology Day Tuesday PM Tuesday PM Tuesday PM 1st & 3rd Site Whiston Hospital Whiston Hospital Whiston Hospital *Note – although patient’s with Skin Cancer are mainly seen at this clinic they can be seen by other consultants at clinics in Whiston & St Helens Multidisciplinary Team Meeting held 1st & 3rd Tuesday in the month at 12.30 Venue: Burns & Plastics Seminar Room Produced by Cancer Services - Version Four (April 2007) - 34 - 4.8 CANCER SERVICE – Upper Gastrointestinal Multidisciplinary Team Members Mr Khan Role Lead Clinician Contact Details Monday to Friday 9-5 0151 430 1239 Mr A. Li UGI Surgeon 0151 430 1528 Ms Chagla UGI Surgeon 0151 430 1607 Mr Kanwar Dr Preistley UGI Surgeon 0151 430 1528 Physician Gastroenterologist 0151 430 1252 Dr Marshall Medical Oncologist 0151 430 1910 Dr Meek Consultant Radiologist 0151 430 1589 Dr Kelly Consultant Histopathologist 0151 430 1824 Paul Madigan 0151 430 1599 Laura Evans Nurse Consultant Gastroenterology Oncology Dietician Kathy McDermott Chest Physiotherapist Bleep 1188 Barbara Ashall Upper GI Nurse Specialist Peter Smith MDT Co-ordinator 0151 290 4143 Bleep 2600 0151 430 1061 Dr Littlewood Consultant in Palliative Care Medicine 0151 430 1381 0151 430 1347 OUT OF HOURS CONTACT INFORMATION Out-patient Advice Via GP/NHS Direct. If urgent local A+E Department Lilac Centre 0151 430 1687 In-patient Advice Ward D3 0151 430 1440 Ward G5 – if chemotherapy related Non-urgent Barbara Ashall CNS Answer Phone service 0151 290 4143 Produced by Cancer Services - Version Four (April 2007) - 35 - ENDOSCOPY SESSIONS Dr Francis Miss Chagla Paul Madigan Mr Khan Mr Kanwar Monday am Alternate Monday p.m. Tuesday/Thursday p.m. Alternate Wednesday p.m. Alternate Monday a.m. and every Friday a.m Alternate Wednesday p.m. Mr Memon Dr Turner OUTPATIENT CLINICS Consultant Clinic Day Site Whiston Ms Chagla UGI/GEN Mr Li General Alternate Monday am Monday am Mr Li UGI/Gen Tuesday pm Whiston Mr Khan UGI/Gen Wednesday am Whiston Mr Khan General Friday pm St Helens Dr Francis Gastro Tues/Thurs pm Whiston 2 week rule Rapid Access Friday pm Whiston Multidisciplinary Team Meeting held every Thursday 08.30 Venue: X-Ray Seminar Room Produced by Cancer Services - Version Four (April 2007) - 36 - St Helens 4.9 CANCER SERVICE – Urology Multidisciplinary Team Members Role Mr Massey Mr Gana Mr Khattak Dr Marshall Dr Malik Lead Consultant Urologist Consultant Urologist Consultant Urologist Medical Oncologist Clinical Oncologist Dr Meek Lead Radiologist Dr M. Pinto Sue Charles Nancy Chisholm Nerys Williams Julie Keith Lead Histopathologist Nurse Specialist Nurse Specialist Nurse Specialist MDT Co-ordinator Extended Multidisciplinary Team Claire Littlewood Role Dennis McComas Lorna Evans Mary McBirnie Consultant in Palliative Care Senior Nurse Specialist Dietitian Urology Sister Ann Caton Urology Sister Carolyn Swash Dr Clark Stoma Nurse Clinical Oncologist (testes patients + bladder patients who required chemotherapy treatment only) Assistant Counselling Manager Shirlie Deveney Contact Details Monday to Friday 9-5 0151 430 1976 0151 430 1907 0151 430 1907 0151 430 1910 Clatterbridge Centre for Oncolgy 0151 334 4000 0151 426 1600 Ex 2492 0151 430 1731 0151 430 1076 0151 430 1898 0151 430 1076 0151 430 1061 Contact Details Monday to Friday 9-5 0151 430 1058 0151 430 1898 0151 430 1201 0151 426 1600 Ex 2528 0151 426 1600 Ex 2528 0151 430 1221 0151 430 1687 OUT OF HOURS CONTACT INFORMATION Out-patient Advice Via GP/NHS Direct. If urgent local A&E Department. In-patient Advice A1 Ward / D1 Ward or Via Urology Surgical On Call Team. Non-urgent Advice A1 Ward / D1 Ward Monday – Friday 9 am – 4pm Urology Nurse Specialist Answer Phone Service. Produced by Cancer Services - Version Four (April 2007) - 37 - OUTPATIENT CLINICS Consultant Clinic Type Mr Massey Urology Mr Massey Urology Day Tuesday pm Thursday pm Mr Gana Urology Wednesday am Mr Gana Mr Gana Urology Urology Mr Khattak Mr Khattak Nursing Team Urology Urology Rapid Access Haematuria Clinic Nursing Team Prostate Assessment Clinics Mr Gana Flexible Cystoscopy Lists Flexible Cystoscopy Flexible Cystoscopy Friday am 1st Wednesday pm Monday AM Thursday PM Monday am & Alternate Thursday pm Monday pm Wednesday am & Alternate Thursday pm Thursday am Mr Massey Dennis McComas Dennis McComas Sue Charles Sue Charles Sue Charles Site Whiston Hospital St Helens Hospital St Helens Hospital Whiston Hospital Newton Hosptial Whiston Hospital Whiston Hospital A1 Ward A1 Ward A1 Ward Friday am Tuesday am A1 Ward A1 Ward Flexible Cystoscopy Wednesday pm A1 Ward Stable Prostate Cancer Clinics Stable Prostate Cancer Clinics Chemotherapy Intravesical Immunotherapy Monday pm Thursday am St Helens Hospital Whiston Hospital Friday pm On the district Multidisciplinary Team Meeting held weekly on a Monday at 11.45 – 12.15 Venue: X-Ray Seminar Room Produced by Cancer Services - Version Four (April 2007) - 38 - 5. PALLIATIVE CARE 5.1 PALLIATIVE CARE - Hospital Specialist Palliative Care Team Team Members Role Dr C Littlewood Consultant in Palliative Medicine Consultant in Palliative Medicine Dr J Wiseman S.P.R. (Rotational every 12 months) Dr Jenny Smith Mrs Jan Leatherbarrow Robert Case Mrs Collette Murray Ms Debbie Maddox Miss Claire Johnston Mr Andrew Dickman Mrs Jackie Bruce Mrs Josie Dold Mrs Denise Delaney Mrs Simone Taylor Team Leader, Specialist Palliative Care CNS Specialist Palliative Care CNS Specialist Palliative Care CNS Specialist Palliative Care CNS CNS – Heart Failure/ FCP Facilitator Pharmacist P.A. to Dr Littlewood Team Secretary Team Secretary Data Entry Clerk/ Admin Assistant Contact Details Monday to Friday 9-5 0151 430 1347 0151 430 1347 0151 430 1347 0151 430 1274 0151 430 1953 0151 430 1274 0151 430 1274 Pager: 07654661703 Or 0151 430 1274 0151 430 1058 0151 430 1274 0151 430 1274 0151 430 1274 OUT OF HOURS CONTACT INFORMATION Out-patient Advice Via GP or Community Nurse In-patient Advice Via Willowbrook Hospice Nurse in Charge 0151 430 8736. Non-urgent Advice Answer Phone Service. Multidisciplinary Team Meeting held weekly, every Wednesday, at 14.00 Venue: Palliative Care Office The Hospital Specialist Palliative Care Service adopts the concept of shared care with other health professionals, aiming to ensure a quality of service and improved quality of life for patients within St Helens & Knowsley Hospitals. The service is aimed at patients with specialist needs relating to life limiting disease and is based on need and not diagnosis. The service provides: Produced by Cancer Services - Version Four (April 2007) - 39 - Specialist support from diagnosis for the patient and family, psychologically, spiritually and socially. Advice on pain and symptom control for patients, relatives and staff. Liaison between hospital and hospice and regular contact with the Specialist Palliative Care Community Nursing Team is maintained. Education is provided both formally and informally, and is available to hospital staff. Support and advice for staff, in their difficult and sometimes complex role of caring for patients with advanced disease. Referrals Referrals to the Specialist Palliative Care Team should be made with: The full agreement of the patient. The full knowledge of the doctor and nurse undertaking the patients care and management. Referral forms can be found in Web Communities under Specialist Groups ‘Specialist Palliative Care http://nww.sthkhealth.nhs.uk/palliative_care. Fax referral 0151 430 1925, or contact direct. A Secretary/answer phone will take messages until a Team member is available to return your call. Produced by Cancer Services - Version Four (April 2007) - 40 - PROTOCOL - How do I use the Referral Form? This 2-sided protocol is to enable Specialist Palliative Care (SPC) Teams within St Helens & Knowsley to standardise and unify practice with respect to (SPC) patient referrals. This protocol was designed and developed collaboratively by the St Helens & Knowsley Integrated Care Network. The aim of the (SPC) referral form is to enhance and develop the exchange of patient referral information across Hospital, Community and Hospice settings. Please note the revised (SPC) referral forma replaces all previous referral forms as at 5th April 2004. To this end please note the following points as well as the ‘Reasons for Referral’ table on side-2, as they apply within each of the (SPC) referral form headings: Page 1 Patient Details: Please provide at least one of the following as they relate to your SPC team NHS number, Hospital ID and Hospice ID At the D.O.B (Date of Birth) please complete as follows: 2 digits to represent day of month; 2 digits to represent month and 4 digits to represent year of birth. e.g If Patient born on the 12 June 1967 this would be 12 06 1967.Plaese note this convention is applicable to all date data-fields within the (SPC) referral form. Please provide were possible Ethnicity/Religion – if this is unavailable insert NA at appropriate data-field Carer Details: Within the ‘Is the Patient Living Alone’ data-field please tick at the appropriate box. (N = No, Y = Yes and NK = Not Known). Involved Professional Details: Community Contact: Within the PCT data-field please tick at the appropriate PCT. Within the ‘DN’ (District Nurse) data-field please insert the name of the DN involved with the patient. This will aid communication between SPC & Community professionals. History of illness: Within ‘Disease Stage’ please tick at the appropriate box Within ‘Disease Management’ please tick at the appropriate box Within ‘Is Patient Aware of Referral’ please tick at the appropriate box Details of Understanding and Medication: Please use free-text were appropriate. Produced by Cancer Services - Version Four (April 2007) - 41 - Page 2 Reasons for referral: Please note the guidance at the top of this section and complete as appropriate. Within the ‘Where is Patient Presently?’ data-field please tick as appropriate Except at Hospital (Ward) – please insert hospital name and ward as appropriate. Service Required: Tick as appropriate for the (SPC) required Tick as appropriate which patient service is required at Willowbrook Hospice Referrer Details: Please state your designation i.e. Consultant, Community Nurse Specialist, Hospital Doctor etc... Your signature shall confirm approval of patient’s GP or Consultant. If (SPC) Referral is More Urgent: Please contact relevant service by telephone Produced by Cancer Services - Version Four (April 2007) - 42 - Reasons for Referral Table Reason for Referral Role of the Health Care Team with Advice and Support from Specialist Palliative Care Team as needed Pain Control Assessment, investigation, diagnosis. Initiate treatment according to Trust formulary. World Health Organisation pain ladder. Monitor and document effect of treatment (at least daily) Criteria for Direct Patient Contact by Specialist Palliative Care Team in conjunction with Ward Team Any Other Symptoms Assessment, investigations, diagnosis. Initiate treatment, evaluate and document outcome (at least daily) Incomplete symptom control. Unacceptable side effects. Complex multiple problems. Psychological Support for Patient +/- Family Basic psychological support. Review and document outcome. Complex psychological and spiritual support. Patient Dying Identify the patient is dying. Assess and address symptom, psychological and spiritual distress. Use of Care Pathway for the Dying Patient. Specialist support to achieve symptom control, psychological and spiritual support. Information/ Communication Provide information about diagnosis and current condition, patient/family needs. Up-date as necessary. Document discussions. Difficult communication issues. i.e. denial, collusion, complex family dynamics. Discharge/ Placement Discharge planning to commence at time of admission as per Hospital Policy. Facilitate rapid discharge to enable patient to die at home. Initiate Hospice Transfer. Uncontrolled/escalating pain (Adapted from Referral Criteria RLUH Palliative Care Team, March 2002) Produced by Cancer Services - Version Four (April 2007) - 43 - ACCESS TO PALLIATIVE CARE OUT-PATIENT CLINICS WHEN & WHERE? MONDAY Held at: WILLOWBRO OK HOSPICE (p.m.) WHISTON (p.m.) COPD – Monthly (commencing 19.04.04) Dr C.M. Littlewood WEDNESDAY THURSDAY FRIDAY WILLOWBROOK HOSPICE (p.m.) Community linked WHISTON (a.m.) Stephenson House Brandreth Suite Parallel clinic to Dr. E. Marshall Oncology/Lung Cancer WHISTON (a.m.) Stephenson House Brandreth Suite Parallel clinic to Dr. A. Flavin Oncology/Breast Cancer Dr. C.M. Littlewood Dr. C.M. Littlewood NEWTON COTTAGE (alternate Wednesdays) Dr. J. Wiseman HOW TO REFER? Referrals for WHISTON clinics - by formal letter to Dr C.M Littlewood, c/o Palliative Care Team, Whiston Hospital Tel: 0151-430-1058 Jackie Bruce, P.A/Supervisor Fax: 0151-430-1925 General Office Referrals for HOSPICE clinics – by formal letter. Referrals will be put into next available clinic with Dr. C.M. Littlewood or D. J. Wiseman. Tel: 0151-430-8736 Paula Younger, Medical Co-ordinator Fax: 0151-493-1006 General Office NOTE: Patients initially attending Whiston clinics may be linked into Hospice services, as felt appropriate. Produced by Cancer Services - Version Four (April 2007) - 44 - Referral for Specialist Palliative Care Services Patient Details NHS Number: Hospital ID: Hospice ID: Title: Forename(s): Gender: Surname: Address: Carer Details Name of Carer: Relationship to Patient: Carer Tel: Is Patient Living Alone? Y Involved Professional Community Contact PCT: GP Name: GP Surgery: GP Tel: Postcode: DN Name: Tel: Hospital Contact Details Age: D.O.B Hospital Consultant: Ethnicity: Religion: Hospital Dept: History of Illness (Please include Diagnosis. Secondary Site – Relevant Treatment) Diagnosis: Date of Diagnosis: Spread/Complications: Disease Stage EARLY ADVANCED Current Treatments: Disease mang’t N CURATIVE NONCURATIVE Past Treatment: Is Patient Aware of Referral: Y Details of Understanding for Patient/Carer Patients Understanding of Diagnosis: N Carers Understanding of Diagnosis: Current Medication Previous Medication (State Reaction/Poor response) 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Produced by Cancer Services - Version Four (April 2007) - 45 - Referral for Specialist Palliative Care Services NHS Number Hospital ID 2 Hospice ID Reason(s) for Referral Please state the main problems that have led to the request for SPC assessment. Include relevant information on physical symptoms (including mobility), carer’s needs, psycho-social/spiritual issues and different ethical needs as appropriate: ……………………………………………………………………………………………………….. ………………………………………………………………………………………………………. ………………………………………………………………………………………………………. ………………………………………………………………………………………………………. ………………………………………………………………………………………………………. Where is Patient Presently? Home Hospital (Ward) N/Home R/Home Service Required ( Please FAX referral to appropriate number) Hospital Palliative Care Team Fax (0151) 430 1925 Community Palliative Care Team Fax (0151) 289 8776 Willowbrook Hospice Fax (0151) 493 1006 Referral to MEDICAL OUTReferral to MEDICAL OUTPATIENT CLINIC FORMAL PATIENT CLINIC FORMAL LETTER ONLY TO: LETTER ONLY TO: Dr Littlewood Dr Wiseman Consultant in Palliative Care Consultant in Palliative Care Medicine, Medicine Whiston Hospital Willowbrook Hospice Prescot L35 5DR Prescot L34 2QT Tel: 0151 430 1274 Tel: 0151 430 8736 If you think this Referral requires ‘OUT-OF HOURS’ Service – Please see details below Referrer Details Print Name Date of Referral Referrer Tel No: If More Urgent: 9.00 am – 5.00 pm Monday to Friday Hospital Palliative Care Team: Tel: 0151 430 1274 Community Palliative Care Team: Tel: 0151 431 0156 OUT-OF-HOURS SERVICE Willowbrook Hospice Tel: 0151 430 8736 All referral will be reviewed within 24-48 HOURS Designation: Signature: (Signature Confirms Approval of Patient’s GP or Consultant). WILLOWBROOK Office Use Only: DATE REFERRAL Received …………….. DATE of INTIAL CONTACT ……………….. DATE of INTIAL ASSESSMENT …………… DATE of ACCEPTANCE ……………………. TO BE COMPLTED ON ORGINAL FORM ACCEPTED REFUSED on OTHER GROUNDS (e.g. too unwell) CANCELLED (e.g. died) Date ………….. Signature ………………….. Produced by Cancer Services - Version Four (April 2007) - 46 - 5.2 PALLIATIVE CARE - Willowbrook Hospice Willowbrook Hospice Portico Lane Prescot Merseyside L34 2QT Telephone: 0151 430 8736 Fax: 0151 493 1006 Willowbrook Hospice is an independent charitable organisation providing specialist palliative care services for the adult population of St Helens and Knowsley Boroughs. Willowbrook Hospice aim to enhance the quality of life, and relieve the suffering of patients with cancer, and other life threatening illness, by providing quality Specialist Palliative Care for those in need, and support for their carers. We are a NO smoking hospice. Specialist Palliative Care In-Patient Service Currently we have nine In-Patient beds. There is no restriction on visiting times and families are encouraged to take an active part in the care of their loved ones if they wish. Staff at the Hospice are always available to offer advice and support whenever it is needed. Referral Criteria For patients with advanced, progressive, incurable, malignant and nonmalignant disease who have complex physical, psychological, spiritual, and social or carer needs. Where the above patient and / or family needs are unable to be met by health professionals in the current care setting and may be met by a specialist palliative care service. Where the current health professionals require the support and advice of the specialist palliative care service. Discharge Procedure Preparation for the discharge of our patients begins on their admission. Willowbrook Hospice is for short periods of treatment only. Patient care is reviewed regularly and future care planned as necessary. Services provided include: In-patient care 9 beds for assessments, symptom control, rehabilitation and terminal care. Outreach Services Day therapy providing up to 10 places on a given day and time. Services offered include: Key worker system - each patient is allocated a key worker to ensure consistency of care. Produced by Cancer Services - Version Four (April 2007) - 47 - Complementary Therapies: Aromatherapy / Massage / Guided Visionary / Reiki / Reflexology Relaxation therapy Physiotherapy / Exercise Programmes /Breathlessness Groups / Anxiety Management Group activity Craft classes Bereavement support Medical review The Day Therapy Team consists of: Team Leader – responsible for Complementary and Creative Therapies Sister Staff Nurse Senior Physiotherapist Therapy Assistant Chaplaincy Team Out patient Service Patients who require initial or follow up appointments can be seen within the out patient facilities at Willowbrook Hospice. Medical Clinics are held at the Hospice weekly, in addition to medical clinics at Whiston Hospital and Newton Community Hospital. Request for appointments are received from Hospital Consultants, General Practitioners or Nurse Specialists via a letter or referral form. Physiotherapy and complementary therapy may be accessed via the outpatient service. Also referrals are accepted from any member of the multi-professional team. Individual or family visits can be arranged to offer a consultation with a doctor. Carers Support Service – Family Support Co-ordinator A Carers’ Support Service is offered at Willowbrook Hospice, as part of our Philosophy of Care. The service aims to provide personal advice, comfort, empathy and support to patients’ carers and relatives including: Offering comfort and support to carer's and relatives of patients attending the Hospice in the anticipatory and post bereavement stages. Trying to ensure the current physical, psychological, social and spiritual needs are met in order to minimise any future harmful effects on health. Facilitating expressions of grief and discuss the grieving process. Advising on available resources and provide practical help when needed. Aiding recovery and assist in resolution. Produced by Cancer Services - Version Four (April 2007) - 48 - Education Education is a major part of our work. Willowbrook Hospice aims to offer coordinated, multi-professional educational programmes, to all members of staff providing Palliative and Specialist Palliative care within Knowsley and St Helens. The Hospice is committed to supporting education and training. Services available include: Raising awareness of the role of Willowbrook Hospice and Hospice services. Involvement within, local organisations, societies, clubs and other groups in the local community. Clinical placements for medical under-graduates, student nurses’, other staff undertaking specialist courses, and overseas visitors, as appropriate. A resource centre on specialist palliative care for multi-professional staff and carers. Providing speakers to inform, educate local organisation – societies, clubs, schools and other community organisations. Committed to the on going development of staff in-house training. Referral The Hospice accepts referrals from the patients’ General Practitioner, Hospital Consultant, or any member of the multi-professional team. In no case will contact be made with the patient without the express prior permission of the patient’s General Practitioner nor without the patient being aware of their diagnosis and that Hospice involvement has been requested. Referrals should be made on the Hospice Referral Form by letter or fully completed single assessment documentation. Produced by Cancer Services - Version Four (April 2007) - 49 - Medical Team Team Members Dr Jenny Wiseman Dr Anthony Thompson Clinical Team Mrs Chris Haywood Mrs Margaret McConaghy Lucy Scriven Role Consultant in Palliative Medicine Assistant Medical Director Head of Clinical Services Team Leader for In-Patient Services Team Leader for Outreach Services Chief Executive Neil Wright Produced by Cancer Services - Version Four (April 2007) - 50 - 5.3 PALLIATIVE CARE - Macmillan Clinical Nurse Specialist Palliative Care Community Community Clinical Nurse Specialists Palliative Care Willowbrook Hospice Portico Lane Prescot Merseyside L34 1QT Telephone: 0151 431 0156 Fax: 0151 289 8776 The service compliments those services provided by the Primary Health Care Team and other providers/agencies. A key principle is that the specialist nurse seeks to work with these other teams/professionals equipping them with the required skills and knowledge. Referral Criteria The Community Macmillan Clinical Nurse Specialists (CNS) within Knowsley PCT and St Helens PCT operate an open referral system. Anyone may refer themselves, or someone else for assessment. Any patient with a malignant disease or life-limiting condition will be accepted to the service. Referrals will be with the full knowledge of the doctor and the nurse-in-charge of the team undertaking the patient’s care and management. The Macmillan CNS will assist the District Nurse Team Leader in assessing the needs of patients and relatives. The Macmillan CNS will not take over care but act as a specialist resource. Patients requiring nursing care should be referred directly to the District Nurse. Not all patients with malignant disease or life-limiting conditions will require intervention from a Macmillan CNS. Referrals should be made with the patient’s agreement and for: Patients who have problematic pain or other symptoms. Patients or their relatives requiring informed support at time of diagnosis/recurrence. Relatives or carers requiring support over and above what Primary Carers provide, and where there are complex needs. Staff requiring support in order to continue caring effectively for the above patient group. Bereavement problems in families known to the Macmillan Service. Referrals can be made by: Completing a referral form Telephone, if urgent, followed by a completed referral form. Contact from the Macmillan CNS, and frequency of visits, will be determined by the Macmillan CNS on an individual basis. Produced by Cancer Services - Version Four (April 2007) - 51 - Team Members Dr Jenny Wiseman Gillian Harthen Amanda Watson Helen Mack Geoff Prince Julie Parr Zoe Keating Maggie Cooke Role Consultant in Palliative Medicine Clinical Nurse Specialist Team Leader Macmillan CNS Macmillan CNS Macmillan CNS Macmillan CNS Macmillan CNS Macmillan CNS Out of hours service Willowbrook Hospice Tel 0151 430 0156 MDT Meeting Clinical Meeting every Monday 9.30 am at Willowbrook Hospice Produced by Cancer Services - Version Four (April 2007) - 52 - 5.4 PALLIATIVE CARE – St Helens Integrated Palliative Home Based Project Integrated Palliative Home Care Team The St Helens PCT and Integrated Palliative Home-Based Project aims to enhance it’s home-based services to those with life threatening conditions. The project will compliment existing health and social care input to enable patients, carers and families to continue with their everyday lives during this time. Referral to this service can be made by any Health Care Profession, patient/carer as long as the patient has been assessed by a District Nurse or Senior Hospital Staff. As care and support is provided according to the needs of the patient and carer, referrals should whenever possible be pre planned so that the service can respond quickly to an urgent situation. Aims of the service. To enable terminally ill patients to be cared for and die at home, where that is their identified wish. To provide nursing care which is supplementary to the existing District Nursing Service. To offer a combination of psychological and practical support to the patient and family. To support the patients with palliative needs from hospital or hospice. To provide support during times of crisis for patient or carer and to prevent unnecessary admission to hospital or hospice. To increase the overall provision of home based Palliative Care. To increase the availability of care for longer periods of the day. To extend community palliative care services to people with cancer and other life threatening conditions. Criteria for Accessing the Integrated Palliative Home Care Team Produced by Cancer Services - Version Four (April 2007) - 53 - The patient must be listed on the Palliative Care Register or have a life expectancy of six months or less [DS1500]. This service is available to any patient who is in the terminal stage of their illness [registered with a St Helens GP], and aims to increase the availability of care for longer periods of the day and night. To access 24 hour round the clock care patients need to be commenced on an Integrated Care Pathway. All patients who are referred and are living at home must have been assessed by the District Nursing Service. All patients must be aged eighteen and over. All patients in hospital who are referred must have been assessed by the ward manager or DN Liaison. The DN Service must be made aware of any referrals of patients being discharged with any of the services. All patients referred to the service must be referred with the full knowledge of the GP These services are here to enhance the District Nursing Services and not to replace them. They will give families added support and security in difficult times. It is very important that families are aware that these services are available to allow patients to choose where they wish to spend their final days. Please try to plan ahead and refer to the service as soon as you have identified the need. Produced by Cancer Services - Version Four (April 2007) - 54 - 5.5 PALLIATIVE CARE - Integrated Palliative Home Care Team – Henrietta Project Any Health Care Professional Patient/Carer can make referral to this service as long as a District Nurse or Senior Hospital Staff has assessed the patient As care and support is provided accordingly to the needs of the patient and carer, referrals should whenever possible be pre planned so that the service can respond quickly to an urgent situation Aims of the service To enable terminally ill patients to be cared for or die at home, where that is their identified wish To provide nursing care which is supplementary to the existing District Nursing Service To offer a combination of psychological and practical support to the patient and family To support the patients with palliative needs from hospital or hospice To provide support during times of crisis for patient and carer and to prevent unnecessary admission to hospital or hospice To increase the overall provision of home based Palliative Care To increase availability of care for longer periods of the day To extend community palliative services to people with cancer or other life threatening conditions Produced by Cancer Services - Version Four (April 2007) - 55 - Criteria for Assessing the Integrated Home Care Team The patient must be listed on the Palliative Care Register or have a life expectancy of six months or less (DS 1500) This service is available to any patient who is in the terminal stage of their illness (Registered with a Knowsley GP) and aims to increase availability of care for longer periods of the day The District Nursing Service must have assessed all patients who are referred and are living at home The patients must be aged eighteen and over The Ward Manager or DN Liaison must have assessed all patients in hospital who are referred. The DN Service must be made aware of any referrals of patients being discharged with any of the services All patients referred to the service must be referred with the full knowledge of the GP These services are here to enhance the District Nursing Service and not to replace them. They will give families added support and security in difficult times It is very important that families are aware that these services are available to allow patients to choose where they wish to spend their final days Please try to plan ahead and refer to the service as soon as you have identified the need Produced by Cancer Services - Version Four (April 2007) - 56 - 6.0 EXTENDED SERVICES 6.1 EXTENDED SERVICES - Hospital Based Pain Team Medical Team Members Role Dr Konstantin Levshankov Dr Mike Forsyth Mrs Mary Doolan Consultant Anaesthetist Staff Grade Anaesthetist Theatre/Chronic Pain Nurse Theatre/Chronic Pain Nurse Secretary Mrs Eileen O’Neil Mrs Anne Roberts Contact Details Monday to Friday 9-17 0151 430 1455 0151 430 1455 OUT OF HOURS-CONTACT INFORMATION Outpatient advice 0151 430 1455 (answer machine) Inpatient advice 0151 430 1455 (answer machine) Anaesthetist on call via switchboard for urgent advice OUTPATIENT CLINICS Consultant Clinic Type Dr K Levshankov Multidisciplinary Spinal Clinic Dr K Levshankov Multidisciplinary Spinal Clinic Dr K Levshankov Theatre session (invasive procedures/TENS/a cupuncture) Dr K Levshankov Outpatient Pain Dr M Forsyth Clinic Dr K Levshankov Pain Management Programme Day Monday pm Site Whiston Tuesday pm St Helens Thursday am Whiston Thursday pm Whiston Friday am Whiston Produced by Cancer Services - Version Four (April 2007) - 57 - Description of the service: Chronic Pain Clinic works in collaboration with Hospital Palliative Care team to provide a range of services aimed at alleviating pain, enhancing the quality of life and functioning of the patients with chronic pain. We aim at improving pain control and addressing pain-modifying issues in the multidisciplinary context. We offer: Initial assessment of pain and pain related issues in the context of its multifactorial and multidimensional nature. Assessment and modification of the treatment regime according to individual needs. Formulation of the pain management approach based on specific needs of the patient in collaboration with Hospital Palliative Care team. Non pharmacological interventions – transcutaneous electrical nerve stimulation, acupuncture. Interventional therapies – neuromodulation, specific neuroablative procedures, systemic and regional drug infusions, somatic and autonomic blocks. Reassessment of the patient’s progress at appropriate and regular intervals and modification of the treatment regime according to individual response. Education of the patient and those involved in the care of the patient. Produced by Cancer Services - Version Four (April 2007) - 58 - 6.2 EXTENDED SERVICES - Chaplain/Pastoral Care Spiritual Care Services The Spiritual Care Team is made up of whole time and part time chaplains representing the different Christian denominations; we also have a Secretary and a large group of carefully selected and trained volunteers. We are here to make provision for the spiritual and religious needs of patients, relatives, and staff of all faiths and none. We are available at all times of the day and night, either through the department (0151 430 1657) or, in emergency and out of hours, by calling the switchboard and asking for the on call chaplain. If you need to contact a religious leader of a non-Christian faith for yourself or a patient in your care we can give details of names and telephone numbers. We can also liase with local churches. Services are held at St Helens and in the Chapel at Whiston at Christmas and Easter and to mark particular events. Our regular services at Whiston Chapel are as follows: Every Sunday there is a Mass at 11 am and Holy Communion at 2 pm On Wednesdays 1.30 – 2 pm Exposition and Quiet Prayer Every Friday staff of the Islamic faith, meet in the Chapel at lunchtime to pray. The Chapel at Whiston is open at all times for prayer or reflection. The Prayer Room at St Helens can also be made available by request. NB For more information please refer to our Patient Information Leaflet and our Staff Support leaflet. We also have a Spiritual Care page on the Intranet. How to Contact the Chaplains: The Spiritual Care Department at Whiston is our main base and Ann Wright, Spiritual Care Secretary, works in the Office on weekday mornings. Our Direct Line is (0151) 430 1657, this can be used for all routine calls. Alternatively please use the bleeps or long range pagers via switchboard. Produced by Cancer Services - Version Four (April 2007) - 59 - Chaplaincy Team Sister Susan Molloy Denomination Roman Catholic Sister Eileen O’Riordan (Part-time) Revd. Jayne Shepherd Head of Department Revd. Jamie Hartwell Roman Catholic Church of England Free Church Contact details Whiston Hospital Site Bleep 0042 St Helens & Peasley Cross Sites Bleep via switchboard All sites – Bleep 0041 All sites – Bleep 0041 Contact details for other Faiths & Special Needs Jehovah’s Witness Church of Jesus Christ Latter Day Saints (Mormon) Unitarian Jewish Othodox Reformed Progressive Lay Visitor Islam/Moslim/Muslim Hindu/Sikh Ba’hai Buddist Seventh Day Adventist Produced by Cancer Services - Version Four (April 2007) - 60 - 0151 430 3296 01744 811077 0151 263 4899 0151 722 2079 0151 722 5438 0151 733 5871 0151 722 1810 0151 709 2560 0151 263 7965 0151 733 8614 0151 727 0108 0151 226 4385 6.3 EXTENDED SERVICES - Department Of Nutrition and Dietetics REFERRAL PROCEDURE If a patient meets the following criteria, please complete a Dietetic referral request form in full. REFERRALS: A doctor or registered nurse (D grade or above) must sign all referrals. PATIENTS WILL NOT BE SEEN IF A REFERRAL REQUEST FORM IS NOT COMPLETED & SIGNED. NUTRITION RISK SCORE MUST BE CALCULATED AND DOCUMENTED ON THE REFERRAL REQUEST FORM. Phone the Dietetic Department on Ext 1201 or 1474 to inform your ward Dietitian that you have a referral. Indicate reason for referral. A referral request form must still be completed, which will be collected when the Dietitian attends the ward. Alternatively the form can be faxed to the Dietetic Department on 1461. The Dietitian aims to see referrals for Enteral and Parenteral Nutrition within one working day (applicable Whiston only). The Dietitian aims to see all other referrals within 2 working days of receiving the referral (applicable Whiston only). Refer as early as possible. Patients referred on day of discharge will NOT be seen as an inpatient. Referrals received after 12.00 noon on Fridays may not be seen until the following Monday. Produced by Cancer Services - Version Four (April 2007) - 61 - DEPARTMENT OF NUTRITION AND DIETETICS REFERRAL CRITERIA PATIENTS WHO WILL BE SEEN AS AN IN-PATIENT: Nutritional risk score High (> 10). Nutritional risk score Moderate (5-9) after review. Patients requiring Parenteral Nutrition (PN). Patients requiring Enteral Nutrition i.e. nasogastric (NG), nasojejunal (NJ), Percutaneous Endoscopic Gastrostomy (PEG), jejunostomy (JEJ) feeding. N.B. Starter feeding regimen available on all wards. Diabetes if: Newly diagnosed New to insulin therapy Poor appetite, weight loss or REGULAR hypos. If patients do not fit one of the categories stated above, give the diet sheet ‘Food and Diabetes’. All newly diagnosed individuals should also be given this booklet to give them basic information until they see the Dietitian. Ulcerative Colitis All newly diagnosed. Patients with previously diagnosed Ulcerative Colitis experiencing weight loss and diarrhoea. Crohn’s Disease All newly diagnosed. Patients with previously diagnosed Crohn’s disease experiencing weight loss and diarrhoea. Coeliac Disease All newly diagnosed. N.B. Gluten free diet available from Catering. Gluten free bread and biscuits available from Pharmacy. Dysphagic patients with a poor oral intake. Patients presenting with cancer cachexia. Oesophagogastrectomy / oesophageal stent. Colostomy / Ileostomy Refer if indicated by nutritional risk score. Produced by Cancer Services - Version Four (April 2007) - 62 - Pressure sores Refer if indicated by nutritional risk score. Liver disease Refer if indicated by nutritional risk score. N.B. Nursing staff to provide patient with “No Added Salt” diet sheet. Renal failure Refer if indicated by nutritional risk score or dietary restrictions are required. Note Low albumin is NOT an appropriate reason for referral as it is a poor marker of nutritional status. Albumin is a good indicator of the severity of illness when used in conjunction with the acute phase proteins, such as C-reactive protein (CRP). Assuming normal hepatic function, When CRP is increased and albumin is low = illness. When CRP is normal and albumin is low = protein depletion. PATIENTS SEEN AS OUT-PATIENTS if complete written referral received. Obese Patients with a BMI > 35 and no other pre-existing medical condition. Those with BMI > 30 with Ischaemic Heart Disease (IHD), Diabetes, COPD or 2 or more risk factors for cardiovascular disease. Nursing staff to provide “Eating for Health” booklet whilst patient is an inpatient. Lipid lowering Patients with a cholesterol > 6mmol/l. Provide non-MI patients with a ‘Healthy Eating for Healthy Heart’ leaflet. MI patients will receive this in their pack from the Cardiac Nurse. PATIENTS NOT SEEN Diverticular Disease Give “High Fibre” diet sheet and Diverticular Disease leaflet produced by the Digestive Disorders Foundation (if purchased by Ward Manager). Gallstones Give “Eating for Health” booklet. N.B. There is no evidence to suggest a role for low fat diets in the management of gallstones. Produced by Cancer Services - Version Four (April 2007) - 63 - Constipation Give “High Fibre” diet sheet and ensure adequate fluid intake. Check medication. Gastric Ulcers Give the leaflet “Practical Advice for Gastric Discomfort” along with “Eating for Health” booklet. Hiatus Hernia, Indigestion, or Heartburn Give the leaflet “Practical Advice for Gastric Discomfort” along with “Eating for Health” booklet. Produced by Cancer Services - Version Four (April 2007) - 64 - Referral to the Dietetic Service – Inpatients St Helens & Knowsley NHS Hospitals Trust Department of Nutrition & Dietetics Request for Dietetic Assessment Date Date Received Ward Consultant Please attach patient information label. If none available, please insert details. (Include NHS Number) Diet Suggested Clinical Details Weight Nutrition Risk Score Signature of Medical Officer Please call the Dept of Nutrition & Dietetics with the above details on Ex 1201. Alternatively fax to 1461 Produced by Cancer Services - Version Four (April 2007) - 65 - Referral to the Dietetic Service – Referral to the Community Dietetic Service For Patients Requiring a Domiciliary Visit Referrals will be triaged. Please use BLOCK CAPITALS and complete in full. Incomplete referrals will be returned Name: ………………………………………………………………………………..….. Address: ………………………………………………………………………..…….... Postcode: …………………………………………………………………………….… Tel No.: ……………………………………………………………………………..…… DOB: ……………………………………………………………………………….……. GP name: ……………………………………………………………………….……… GP address: ……………………………………………………………………….…… ----------------------------------------------------------------------------------------------------------------1) Appetite reduced from normal quantities for >2 weeks? : Yes □ No □ 2) Is visual weight loss apparent? : Yes □ No □ 3) Recent 3 month weight history: …………… …………… …………… Current BMI :…………... 4) Is the patient palliative? : Yes □ No □ ----------------------------------------------------------------------------------------------------------------Diagnosis & Clinical Details: ……….……………………………………………..… ……………………………………………………………………………………………… ……………………………………………………………………………………………… Diet Suggested ……………………………………………………………………………… ………………………………………………………………………………………………….. Relevant Medication: ……………………………………………………………..… ……………………………………………………………………………………………….. ___________________________________________________________________ GP Signature: Date: Print name: Designation & Base: Please send to Dietetics, Birch House, Whiston Hospital or fax to 0151 430 1461 Produced by Cancer Services - Version Four (April 2007) - 66 - Referral to the Dietetic Service – Referral to ‘CHANGES’ the Adult Weight Management Service (Inclusion criteria – BMI ≥ 35kg/m2) Please use BLOCK CAPITALS and complete in full (any incomplete or inappropriate referrals will be returned) Name: ………………………………………….. Title: ………. D.O.B: ……………………… Address: ……………………………………………………………………………………… Postcode: …………………………………….. Tel No: ………………………………….. GP name: ……………………………………………………………………………………. GP address: …………………………………………………………………………………. ___________________________________________________________________________________ Medical History Diagnosis & Clinical Details ……………………………………………………………….. ………………………………………………………………………………………………… Diabetes □ Stroke □ Osteoporosis □ Sleep Apnoea □ MI □ Cancer □ Chronic Joint Pain □ Epilepsy □ Angina □ Renal □ Thyroid Dysfunction □ Psychiatric Illness □ PCOS □ COPD □ Anxiety/Depression □ Post Surgery □ Weight related infertility □ History of eating Disorder □ Others ………………………………………………………………………………………... __________________________________________________________________________________ Height ………….cm Weight ……………..kg BMI ………………..kg/m2 (Inclusion criteria – BMI ≥ 35kg/m2) Biochemistry Cholesterol ………mmol/L TG ………mmol/L HDL ……… mmol/L LDL ……… mmol/L FBS………..mmol/L HbA1c …………….% (diabetes only) Blood Pressure …………..mm/Hg Others …………………….. Relevant medication List of current medications attached □ Not currently on any medication □ ____________________________________________________________________________________ Any special requirements e.g. wheelchair access, hearing impairment, literacy difficulties, learning difficulties, translator needed, registered blind please specify ………………………………………………………………………………………………………. ………………………………………………………………………………………………………. If a domiciliary visit is required is there any information which needs to be known? Please state: ………………………………………………………………………………………… ……………………………………………………………………………………………………… ____________________________________________________________________________________ Signature of referrer: Print Name: Address: Date: Designation: GP/PN/Other ….............. Please send to the Weight Management Service, Department of Nutrition and Dietetics, Old Tower Hill Health Centre, Moorfield, Kirkby, Merseyside, L33 1XD In collaboration with St Helens PCT and St Helens Council Produced by Cancer Services - Version Four (April 2007) - 67 - 6.4 EXTENDED SERVICES - The Speech & Language Therapy Service The Speech and Language Therapy Service is provided by Knowsley Primary Care Trust. All Speech and Language Therapists are licensed and registered by the Royal College of Speech and Language Therapists and are members of the Health Professions Council. The role of the Speech and Language Therapist is to provide assessment, treatment and advice to people and/or their relatives who have difficulties with communication and/or swallowing. There is an open referral policy, which allows anyone to make a referral to the service, however swallowing referrals must be signed by a doctor. Referrals from professionals must be in writing. Speech and Language Therapist generally work as a member of a multidisciplinary team which may consist of Doctors, Nurses, Physiotherapists, Occupational Therapists, and Dietitians according to need. Referrals should be sent to:The Speech and Language Therapy Service Henley House Delph Lane Whiston Merseyside L35 7JE Telephone Number: - 0151 290 2010 Fax Number:- 0151 290 2017 Please do not hesitate to contact us if you would like more information or would like to discuss a referral. Produced by Cancer Services - Version Four (April 2007) - 68 - 6.5 EXTENDED SERVICES – SUPPORT Smoking Cessation SUPPORT FOR THOSE WHO WANT TO QUIT SMOKING SUPPORT Smoking Cessation Service Do you support patients who are smokers ? St Helens & Knowsley SUPPORT aims to offer friendly advice and support to smokers who want to stop smoking. Since its launch in November 1999, we have received over 6000 referrals and helped nearly 4000 people to set a quit date. Over 50% of those setting quit dates with SUPPORT, stayed quit for at least 4 weeks. A smoker using SUPPORT is 6 times more likely to stay quit than someone using willpower alone. How can I find out more information, or be referred to SUPPORT ? Hospital patients can be referred to the community based SUPPORT service. Once they are discharged from hospital, they can receive weekly support from one of our smoking cessation specialists. Referral form can be completed and faxed to the most appropriate number on the referral form. Staff can also be supported in their quit attempt by attending regular counselling sessions, usually run in the hospital. Nicotine Replacement Therapy products or Zyban will be available on prescription, provided you are suited to their use. Intensive help and advice is also available. Leaflets and posters are available to any member of staff wishing to promote the stop smoking message. For further help/information, contact Emma Sloan on ext 1431 (Monday &Tuesday only) or Andrea Goodman 01744 811735 on any other day. Produced by Cancer Services - Version Four (April 2007) - 69 - Referral system for Hospital Patients Ask the patients Do you smoke? Have you ever tried to stop? Are you interested in stopping smoking? If no interest is shown If interested in stopping smoking Advise smoker to stop ADIVSE Give clear, strong, personalised advice Tie smoking to immediate health effects and consequences Give relevant information leaflets Inform of: National helpline for further info on 0800 169 0169 Self-referral to SUPPORT on 0800 1952131 Refer to SUPPORT Fax Referral Self Referral Complete patient details on referral form By ringing 0800 195 2131 (use for patients who live outside St Helens and Knowsley district) Fax form to one of the 4 numbers the bottom of the form depending on where the patient lives For further help/information, contact Emma Sloan on ext 1431 (Monday & Tuesday only) or Andrea Goodman 01744 811735 on any other day. Produced by Cancer Services - Version Four (April 2007) - 70 - SUPPORT ST HELENS & KNOWSLEY FOR THOSE WHO WANT TO QUIT SMOKING merseyside health action zone a healthy life for merseyside SECTION ONE – BRIEF INTERVENTION ASK/ASSESS SMOKER ADVICE ALL SMOKERS TO STOP ASSIST FOLLOW UP IF INTERESTED YES NO REFER TO SUPPORT YES/NO THIS PATIENT HAS EXPRESSED A GENUINE DESIRE TO STOP SMOKING PATIENTS NAME NHS No ADDRESS TELEPHONE No POSTCODE NAME OF PATIENTS GP PATIENTS SIGNATURE OF CONSENT DOES THE PATIENT HAVE ANY HEALTH CONDITIONS THAT YOU FEEL SUPPORT SHOULD BE MADE AWARE OF REFERRERS NAME REFERRERS TEL No/ADDRESS (if you require feedback of patients progress) REFERRER IS GP PN Hospital HV DN Cardiac Rehab Other (Please state) Midwife Hosp Facilitator Pharmacy FAX TO: ST HELENS (North & South) 01744 755439 NEWTON/HAYDOCK 01925 271014 KIRKBY 0151 545 0141 KNOWSLEY (Central & South) 0151 292 9355 Produced by Cancer Services - Version Four (April 2007) - 71 - EXTENDED SERVICES – ICCP (Integrated Cancer Care Programme) 6.6 Aims 1. To improve the overall quality of Cancer care by increasing co-ordination between care. Providers, thus strengthening communication links with patients and their carers. 2. To reduce duplication of effort and prolonged or unnecessary hospital admissions. 3. To improve the satisfaction of both patients carers and staff with the care delivered to people with cancer. Benefits for you... The right care at the right time in the right place. A single point of contact through a Care Co-ordinator for community services. Reduced anxiety and timely support for you, your family, carers and friends. Improved access to information at each stage of the care pathway. Improved quality of care by closely following your journey, ensuring compliance with care procedures. Eliminating gaps and avoiding duplication of services. Responding to your preferences for treatment and care. Use existing resources more efficiently and effectively, adjusting to local needs and priorities. More knowledgeable district nurses who will acquire additional training and skill in patient assessment, communication and management of changes in condition The Local Plan Patient’s will be contacted by ICCP Care Co-ordinator. The Care Co-ordinator will need 15 minutes to ask you about your health, living and support arrangements and any specific concerns you have. Throughout your care the Care Co-ordinator will co-ordinate information on your appointments, treatments, referrals, medication, periods of stay in different care settings and transfer between them. You will be offered support to increase awareness of your condition and enable you to identify and react appropriately to changes. The Care Coordinator, and a senior staff nurse, will be able to offer direct healthcare advice and, through links to specialists in Cancer care, will answer any concerns that arise. Produced by Cancer Services - Version Four (April 2007) - 72 - Data Safety To ensure the most appropriate care is offered, confidential records of your health and personal details will be held and maintained by the ICCP Care Coordinator in a secure, password protected electronic database, which is registered under the Data Protection Act 1998. All staff involved in this programme receive training and updates in data security and the Caldicott Guidelines, (Strict guidelines for releasing patient information therefore ensuring patient confidentiality). Specialist Support If you require this leaflet in another language, large print or another format, please contact the ICCP Care Co-ordinator. Your Views Your comments on the quality of our services are always welcome. The Care Co-ordinator will be happy to answer concerns and pass on feedback regarding this programme. For further information on the Integrated Cancer Care Programme, contact the ICCP Care Co-ordinator Jackie Ward Tel: 0800 121 8396 Produced by Cancer Services - Version Four (April 2007) - 73 - 7. SUPPORT GROUPS 7.1 SUPPORT GROUPS - Local Support Groups/Services Service Age Concern Role Advice and assistance to elderly people in the community. Benefits Agency Office Advice and assistance with benefits. Benefits Advice Free confidential advice the first Thursday of the month between 3 pm – 5 pm in the General Office Day Room outside the Lilac Centre, Rowan House. No appointment is required. This is supported by St Helens Carers Centre. Produced by Cancer Services - Version Four (April 2007) - 74 - Contact Details Age Concern St Helens Mansion House Victoria Park St Helens, WA10 2UE Tel: 01744 752644 ageconcern@acsthelens.or g.uk www.acsthelens.org.uk Age Concern Knowsley 1 Griffiths Road Huyton, L36 6NA Tel: 0151 480 4632 e-mail: frank.reppion@acknowsley .org.uk www.ageconcernknowsley. org.uk Benefits Agency Office Gregson House 2 Central Street St. Helens, WA10 1UF Tel: 08456088503 www.dwp.gov.uk Lilac Centre Rowan House Whiston Hospital Warrington Road Prescot, L35 5DR Tel: 0151 430 1687 Bosom Buddies Breast Cancer Support Group. The aim of the group is to help and support. Meetings the first Wednesday of every month at 7.00 p.m. Trinity Church Peel House Lane Widnes Widnes & Runcorn Cancer Support Group 21-23 Alforde Street Widnes WA8 7TR Tel: 0151 423 5730 Citizens Advice Bureau Confidential advice www.citizensadvice.org.uk and information on a wide range of subjects. HALEWOOD 15/21 Ravenscourt, Leathers Lane Halewood L26 OUP Tel: 08451221300 KNOWSLEY 10A Church Street Prescot L34 3LA Tel: 08451221300 HUYTON Nutgrove Villa 1 Griffiths Road, Huyton Merseyside, L36 6NA Tel:08451221300 www.knowsleycab.org.uk ST HELENS Millennium Centre Corporation Street St Helens, Merseyside, WA10 1HJ Advice line: 08701212027 Appt: 01744 737866 www.adviceguide.org.uk Knowsley Cancer Support Group for people with any kind of cancer. Offers support and information, social activities, library, telephone support, and home and hospital visits. Open Monday to Friday,10am–3:30 p.m. Produced by Cancer Services - Version Four (April 2007) - 75 - “Lyndale” 40 Huyton Lane Liverpool L36 7XG 0151 489 3538 Knowsley Carers Centre Patient Partnership Group Roy Castle Samaritans Offering: - Information, Support, Respite, Social Activities, Sign Posting, Advice, Carers Groups, Voucher Scheme, Emergency Cards, Benefits Advice, Newsletter The group was established in June ’06 and represent the voice of cancer service users to the Trust, covering all tumour types, social classes and ethnic minorities. The group provide a forum for patients and carers to influence the development of cancer services within the locality and are actively involved with Trust business and participate in service improvement initiatives. Support Group for people/carers with Lung Cancer Meets at 2 pm first Tuesday of each month. 24 hour telephone Helpline Produced by Cancer Services - Version Four (April 2007) - 76 - Knowsley –Carers Centre 149 Cherryfield Drive Kirkby Knowsley L32 8SE Tel: 0151 549 1412 Halewood –Carers Centre St Mary Day Centre Hillingten Avenue Huyton L26 9TY Tel: 0151 448 9771 Meeting take place every 6 weeks on a Tuesday evening at 1730 to 1930 in the Post Graduate Centre, Whiston Hospital. For further information contact Mrs Jacquie Kelly, Service Improvement Facilitator, Cancer Services, Whiston Hospital, Tel: 0151 430 1055 200 London Road Liverpool Meresyside L3 9TA Tel: 0800 358 7200 Website: www.roycastle.org 0151 708 8888 St Helens Cancer Support Group Travel the journey together. Informal atmosphere. Chance to meet people who have just had cancer. Share experiences or just sit and listen. Carers and family members welcome. Monthly meeting last Monday of each month at The Millennium Centre, St Helens, at 7pm, Weekly drop-in meeting every Friday Millennium Centre between 1 pm – 4 pm. Mr Denys Floyd 01744 884097 Widnes & Runcorn Cancer Support Group Offering: - Information, Support, Social Activities, Sign Posting, Advice, Carers Groups, Welfare Rights, Legal Advice and Benefits Advice. 21 Alforde Street Widnes WA8 7TR Tel: 0151 423 5730 Open 10am-3pm every day Cancer Self Help Group meets every Thursday afternoon 1.30 pm – 3.00 p.m. Hand-in-Hand group 2nd Wednesday of every month 7.30 pm at Old Police Station, Mersey Road, Runcorn. Website: Produced by Cancer Services - Version Four (April 2007) - 77 - Email: dee.graal@tiscali.co.uk www.widnesruncorncsg.org .uk 7.2 SUPPORT GROUPS - Local Bereavement Support Service Role Age Concern – Knowsley Free and confidential bereavement support. Contact Details 0151 480 4632 www.ageconcer nknowsley.org. uk Cancer Counselling Lilac Centre, Whiston Hospital Free and confidential bereavement support. 0151 430 1687 Knowsley Counselling Service Free and confidential bereavement support. 0151 480 6270 www.knowsleyc ounsellingagen cy.com Liverpool Bereavement Service Free and confidential bereavement support. 0151 708 6706 Samaritans – Liverpool Free and confidential bereavement support. 0151 708 8888 St Helens Bereavement Service Free and confidential bereavement support. 01744 451793 Produced by Cancer Services - Version Four (April 2007) - 78 - 7.3 SUPPORT GROUPS - National Support - General Service British Association for Counselling and psychotherapy Role BAC can refer people to a local counsellor. They have information sheets on counselling. Wessex Cancer Trust Offers emotional support and practical help where possible, through support groups around the country. Telephone and one-to-one counselling, telephone link service, holiday accommodation and information on other charities and cancer-related organisations. Offers confidential counselling to individuals, couples or families affected by cancer. Counselling is given by registered counsellors and psychotherapist. Face to face counselling is offered at the London office; for people unable to get to the London office telephone counselling is available. Gives information on cancer treatments and research trials. Cancer Counselling Trust Cancer Research UK Produced by Cancer Services - Version Four (April 2007) - 79 - Contact Details BACP House 15 St John’s Business Park, Lutterworth, Leicestershire LE17 4HB Tel: 0870 443 5252 Email: bacp@bacp.co.uk Website: www.bacp.co.uk www.cancercaresoci ety.org 1 Noel Road, London N1 8HQ Tel: 020 7704 1137 Fax: 020 7704 8620 Email: support@cctrust.org. uk Website: www.cctrust.org.uk P.O.Box 123 Lincoln's Inn Fields, London WC2A 3PX Support ServicesTel: 020 7121 6699 Switch:02072420200 Email: cancer.info@cancer. org.uk Website: www.cancerresearch uk.org Cancer BACUP Offers support and information on all aspects of cancer. Telephone advice provided by Specialist nurses. Cancer BACUP's cancer counselling service offers counselling at its London and Glasgow based offices The counselling service can provide information about counselling and what services are available in local areas. CancerLink Offers support and information on all aspects of cancer in response to telephone and letter enquiries. Acts as a resource to over 370 cancer support and self help groups throughout the UK and publishes a range of publications on issues about cancer. (merged with Macmillan Cancer Relief) Macmillan Cancer Relief Provides home care nurses through the Macmillan Service and financial grants for people with cancer and their families. Marie Curie Cancer Care Runs ten centres (hospices) throughout the UK and a community nursing service, which works with the district nursing service and supports cancer patients and their carers in their homes. Produced by Cancer Services - Version Four (April 2007) - 80 - Cancerbacup 3 Bath Place, Rivington Street, London, EC2A 3JR Support Service on 020 7696 9003 or Freephone 0808 800 1234 to speak to a cancer specialist nurse. Lines are open MondayFriday, 9am – 8 pm www.cancerbacup.or g.uk e-mail through website fax: 02076969002 cancerline@macmill an.org.uk www.macmillan.org. uk Macmillan Cancer Relief 89 Albert Embankment London SE1 7UQ Freephone: 0808 8082020 9 am to 10 pm Monday to Friday 89 Albert Embankment London SE1 7TP Tel: 02075997777 Email through website www.mariecurie.org. uk QUIT Provides telephone support and information leaflets for smokers who want to stop. Can also refer you to local stop smoking groups. General – Smoking Cessation see page 70 Tenovus Cancer Information Centre Cancer Buddies Network Provides an information service on all aspects of cancer and practical and emotional support for cancer patients and their families. Freephone cancer helpline staffed by nurses, social worker and counsellor. Drop-in centre and support group. Brings together people form all walks of life for support and friendship. Produced by Cancer Services - Version Four (April 2007) - 81 - Quit, Ground Floor, 211 Old Street London EC1V 9NR Helpline:: 0800 002200 Email: Counselling: stopsmoking@quit.o rg.uk Email: info@quit.org.uk Website: www.quit.org.uk 43 The Parade, Cardiff, CF24 3AB Tel:02920482000 www.tenovus.com www.cancerbuddies network.org National Support – Children Sargent Cancer Care for Children The Children’s Cancer and Leukaemia Group (CCLG) (Former The UK Children's Cancer Study Group) Winstons wish Offers emotional and financial support to young people under the age of 21 who have been diagnosed with cancer. Sargent Care Professionals are based at major centers throughout the UK and support each child and family from the date of diagnosis onwards. CLIC Sargent Griffin House 161 Hammersmith Road, London W6 8SG Tel: 020 8752 2800 Child Cancer Helpline: 0800 197 0068 Mon-Fri 9 am to 5 pm Email: helpline@clicsargent .org.uk Website: www.sargent.org Umbrella organisation of all UKCCSG children's cancer centres within University of the UK. It formulates treatment Leicester, 3rd Floor, plans, runs clinical trials, Hearts of Oak researches and monitors new House,9 Princess drugs and produces a booklet, Road, West available in four different Leicester, LE1 6 TH languages, called 'A parent's Tel:01162494460 Guide to Children's Cancer.' Fax: 01162549504 Email: info@cclg.org.uk Website: www.ukccsg.org.uk Winston’s Wish is a charity which supports bereaved children and young people. They also offer guidance and information to families and to anyone concerned about a child after bereavement. Produced by Cancer Services - Version Four (April 2007) - 82 - Winstons Wish Clara Burgess Centre, Bayshill Road, Cheltenham, GL50 3AW Tel:01242515157 Helpline:084520304 05 Email: info@winstonswish. org.uk Website: www.winstons.org.u k National Support – Teenagers Riprap General – support for teenagers A website developed especially for teenagers who have a parent with cancer Produced by Cancer Services - Version Four (April 2007) - 83 - www.riprap.org.uk Hilde Hjelmeland Ahmedzai Rip Rap Project Manager University of Sheffield. Trent Palliative Care Centre, Little Common Lane, Sheffield, S11 9NE 7.4 SUPPORT GROUP - National Support – Site-Specific BREAST Hereditary breast cancer helpline A national helpline giving information and help to women concerned about a family history of breast cancer. Has an information pack on genetic testing for breast cancer. UK Breast Cancer Coalition Organisation which campaigns to improve the welfare and health interests of all women in this country with, or threatened by breast cancer. Breast Cancer Care A national organisation giving emotional support and practical advice to women who have, or fear they may have, breast cancer. Has a national volunteer support service. BRAIN British Acoustic Neuroma Association Gives information and support for people with acoustic neuroma. Produced by Cancer Services - Version Four (April 2007) - 84 - Information Centre, St Anne Cottage, Over Haddon, Derby, DE45 1JE Tel: 01629 813000 Email: canhelp@btopenwor ld.com Website: cancerhelp.org.uk 1D Broadway House 112-134 The Boarding Wimbledon, London SW19 IRL Tel: 020 8543 5577 Email: info@ukbcc.org.uk Website: www.ukbcc.org.uk Kiln House, 210 New King's Road, London SW6 4NZ Tel: 0207 384 2984 Tel: 0808 800 6000 Minicom helpline: 080 800 6001 Email: info@breastcancerc are.org.uk Website: www.breastcancerca re.org.uk Oak House, Ransom Wood Business Park, Southwell Rd West, Mansfield, Notts NG21 0HJ Tel: 01623 632143 Email: admin@banauk.com Website: www.bana-uk.com COLORECTAL Bowel Cancer (former: Colon Cancer Concern & Beating Bowel Cancer) Provides an information service; funds research into new treatments for bowel cancer; and campaigns for better treatments and screening programmes British Colostomy Association Offers support, reassurance and information to anyone who has had a colostomy or is facing one. Offers home and hospital visits by experienced colostomates, and telephone advice and support. Twenty area organisers throughout Great Britain. The Ileostomy and Internal Pouch Support Group Aims to help anyone who has had, or is about to have their colon removed and has an ileostomy or internal pouch. A network of over 60 branches throughout the UK provide advice, information leaflets and home/hospital visiting. Has membership fees. Produced by Cancer Services - Version Four (April 2007) - 85 - 7 Rickett Street, London, SW6 1RU Tel: 020 7381 9711 Helpline: 08708506050 Email: admin@bowelcance r.org.uk Website: www.bowelcancer.or g.uk 15 Station Road, Reading, Berkshire RG1 1LG Tel: 0800 328 4257 Tel: 0118 939 1537 Email: cass@colostomyass ociation.org.uk Website: www.colostomyassoi caition.org.uk Peverill House, 1-5 Mill Road Ballyclare, Co. Antrim BT39 9DR Tel: 0800 018 4724 Tel: 028 9334 4043 Fax: 028 9332 4606 Email: info@theia.org.uk Website: www.ileostomypouc h.demon.co.uk GYNAECOLOGY Gynae C A support organisation for women with gynaecological cancers and their partners, families and friends. Provides publications, meetings, telephone support and counselling. 1 Bolingbrooke Road, Swindon, Wiltshire, SN2 2LB Tel: 01793 491116 Email: Gynae_C@yahoo.co m Website: www.communigate.c o.uk/wilts/gynaec Ovacome A national support group for all Elizabeth Garrett those involved with ovarian Anderson Hospital, cancer, including patients, Huntley Street, families, friends, carers and London. WC1E 6DH health professionals. Tel: 020 73809589 Email: ovacome@ovacome .org.uk Website: www.ovacome.org.u k The Daisy Network Offers support, group meetings PO Box 183, (Premature and workshops for woman Rosendale, BB4 menopause support affected by premature 6WZ group) menopause. For written information send a large SAE Email: to the above address. Daisynetwork.org.uk Website: www.daisynetwork.o rg.uk Produced by Cancer Services - Version Four (April 2007) - 86 - HAEMATOLOGY International Myeloma Foundation: UK Office Funds research into myeloma and also provides information to patients on any aspect of myeloma and its treatment. Produces a helpful booklet 'A concise review of the disease and treatment options'. Myeloma UK, Lower Ground Floor,37 York Place, Edinburgh, Scotland EH1 3HP Tel:+44(0) 1315573332 Helpline: 0800 980 3332 Email: myelomauk@myelo ma.org.uk Website: www.myeloma.org.u k Unit 2-3 Heathgate Place 75-87 Agincourt Road, London NW3 2NU Tel: 020 7284 1234 Email: heathgate@anthony nolan.org.uk Website: www.anthonynolan.o rg.uk. Anthony Nolan Bone Marrow Trust Runs Europe's largest register of fully tissue-typed volunteer donors. Anyone wishing to be a bone marrow donor should contact the Donor department. Leukaemia Research Fund Devotes all its resources to research into the causes, treatment and cure of leukaemia, the lymphomas and melanoma. Provides a patient information service and booklets on the diseases and their treatment. 43 Great Ormond Street London WC1N 3JJ Tel: 020 7405 0101 Email: info@lrf.org.uk Website: www.lrf.org.uk Lymphoma Association The Lymphoma Association provides information and emotional support to anyone whose life has been affected by lymphoma (lymphatic cancer) . The helpline is staffed by people who have had training in understanding lymphomas, their treatments and related issues. P O Box 386, Aylesbury, Buckinghamshire HP20 2GA Freephone: 0808 808 5555 Email: information@lympho ma.org.uk Website: www.lymphoma.org. uk Produced by Cancer Services - Version Four (April 2007) - 87 - Leukaemia Care HEAD & NECK British Thyroid Foundation National Association of Laryngectomee Clubs Several local groups throughout Britain. Offers support and companionship to patients and their families. Some financial assistance is available and a small number of holiday caravans. One Birch Court, Blackpole East, Worcester WR3 8SG Tel: 01905 755977 24hour careline: 0800 169 6680 Email: enquiries@leukaemi aCARE.org.uk Website: www.leukaemiacare. org.uk Produces a newsletter and booklets about the thyroid gland, thyroid disease and thyroid cancer. Runs a network of local support groups. Aims to promote the welfare of laryngectomy patients and their families. Produces a range of booklets, including a handbook for patients. Supports 80 local laryngectomy clubs. Visits preand post-operative patients. PO Box 97, Clifford, Wetherby, West Yorkshire LS23 6XD Tel: 01423 709707 www.btf-thyroid.org Lower Ground floor 152 Buckingham Place Road, Victoria, London SW1W 9TR Tel: 0207 703 8585 www.patient.co.uk Produced by Cancer Services - Version Four (April 2007) - 88 - Information Website: www.laryngectomee s.inuk.com LUNG Roy Castle Lung Cancer Foundation British Lung Foundation Funds medical research, patient care, and advocacy. Has a lung cancer patient network which provides support groups, information booklets on lung cancer and treatments, and a video on dealing with breathlessness. Support group meets the first Tuesday of every month. Raises funds for research into lung diseases and provides information. Runs Breathe Easy: a free club for people who have breathlessness. Has a support network and a newsletter which offers a "keep in touch" service. Produced by Cancer Services - Version Four (April 2007) - 89 - 200 London Road, Liverpool, Merseyside L3 9TA Tel: 0800 358 7200 Website: www.roycastle.org 73/75 Goswell Road, London EC1V 7ER Tel: 020 7688 5555 Fax: 020 7688 5556 Email: breatheasy@britishl ungfoundation.com Website: www.lunguk.com SKIN MARCS Line (Melanoma and Related Cancer of the Skin) Wessex Cancer Trust is the home of the MARC’s helpline and advice centre MARCS Line is a telephone information service for people with skin cancer, their families and friends. Provides information, literature and advice about skin cancers and their prevention. Skin Cancer Research Fund Promotes research into all aspects of skin cancer and provides support and information to people with skin cancer. Skinship UK A telephone helpline for anyone with skin problems including cancer. Puts patients in touch with other patients. Offers one to one counselling. SKIN/ HEAD & NECK British Association Members are helped to of Skin Camouflage disguise skin problems with camouflage make-up. Produced by Cancer Services - Version Four (April 2007) - 90 - Wessex Cancer Bellis House 11 Westwood Road Southhampton S)17 1DL Email: MARCS line@salisbury.nhs.u k Website: www.wessexcancer. org Department of plastic surgery, Frenchay Hospital, Frenchay, Bristol, BS16 1LE Tel: 0117 970 1212 Email: caroline.newton@no rthbristol.swest.nhs.uk Plascow Cottage, Kirkgunzeon, Dumfries, DG2 8JT Tel: 01387 760567 P.O.Box 202 Macclesfield, Cheshire, SK11 6FP Tel: 01625 871129 Email: Basc9@hotmail.com Website: www.skincamouflage.net Disfigurement Guidance Centre Provides advice, support and practical help to patients and health professionals. Let's Face It Support Network Provides support, information and mutual help for people with facial disfigurement. Oesophageal Patients Association The Association’s objectives are to help new patients and their families to cope with any difficulties arising as a result of treatment. UROLOGY Urostomy Association Orchid Cancer Appeal Helps people who are about to have, or have had, surgery resulting in the diversion or removal of the bladder. Gives information, help and advice on appliances, work situations, and marital problems. Funds research and promotes awareness into testicular and prostate cancer. Produced by Cancer Services - Version Four (April 2007) - 91 - Website: www.dgc.org.uk 72 Victoria Avenus Westgate on sea Kent CT8 8BI Tel: 01843833724 Email: chrisletsfaceit@aol.c om Website: www.lets-faceit.org.uk Chairman: David Kirby 22 Vulcan House Vulcan Road Solihull B91 2JY Tel: 0121 704 9860 Website: www.opa.org.uk Central Office, 18 Foxglove Avenue, Uttoxeter,Staffs, ST14 8UN Tel: 08707707931 Email: secretary.ua@class mail.co.uk Website: www.uagbi.org St Bartholomew's Hospital, London EC1A 7BE Tel: 020 7601 7808 Email: info@orchidcancer.org.uk Website: www.orchidcancer.org.uk St Helens & Knowsley Hospitals Cancer & Palliative Care Service Directory 8. Amendment Form If you have any changes, please fill in the form below and return to: Anita Corrigan, Lead Nurse/Manager – Cancer Services, Whiston Hospital. Tel: 0151 430 1055 Fax: 0151 430 1074 Date………………………………………………Page……………………………… Name………………………………………………………………………………….. Title…………………………………………………………………………………….. Address……………………………………………………………………………….. ………………………………………………………………………………………….. Telephone………………………………………. E-mail………………………………... Website……………………………………………………………………………… Any other changes……………………………………………………………………………… ………………………………………………………………………………………….. Produced by Cancer Services - Version Four (April 2007) - 92 -