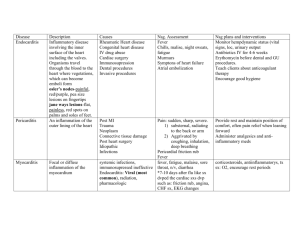
Inflammatory Disease Affecting the Heart
Infective Endocarditis, Pericarditis/Cardiac tamponade, Myocarditis
Inflammatory Diseases Affecting Heart
Pathophysiology
Various causes of inflammatory disease affecting heart (bacteria, fungus)*
Review rheumatic fever and RHD management;*Also Valvular
Endocarditis: precipitated by bacteria/fungal infection; untreated > death
from emboli and valvular disturbance
Myocarditis: virus, toxin or autoimmune response damaging heart muscle >
cardiomyopathy and death (recall Mod 5-cardiomyopathy)
Pericarditis: Bacterial, fungal or viral infection affecting visceral and parietal
pericardium; restricts heart pumping action> cardiac tamponade/death!
INFECTIVE ENDOCARDITIS –You Tube Video Endocarditis
Etiology/Pathophysiology
Infective endocarditis (IE) (previously known as bacterial endocarditis)infection of endocardial surface of heart > affects cardiac valves; commonly
treated with IV antibiotics as penicillin (see Tab. 37-5); 15,000 cases
diagnosed yearly in US
o Occur in people with congenital & valvular disease; history RHD &
people with normal values with inc. amts bacteria
o Valvular damaged > blood flow slows > clot forms; bacteria present in
blood stream > bacteria or fungal vegetative growths deposits form on
abnormal valves
Risk factors (Tab. 37-2)9,: Hx RHD, prior hx endocarditis, invasive
procedures (introduce bacteria into blood stream); recent dental surgery;
permanent central lines; IVDA, valve replacements, etc
Classification system
o Subacute (typically affect those with preexisting valve disease)
Gradual onset; systemic manifestation
o Acute (typically those with healthy valves), usually staph aureus.
Abrupt onset; rapid course; usually staph aureus
o **Generally classified according to: 1. Cause as IV drug use, 2.
Site of involvement (prosthetic valve), 3. Agent as fungal
endocarditis.
Most common causative organisms of IE –Bacteria: Staphylococcus aureus
and Streptococcus viridian; Viruses and Fungi. (Tab. 37-1)
Vegetations (fibrin, leukocytes, platelets, & microbes), primary lesions of
IE, adhere to valve surface or endocardium can embolize to various
organs (particularly lungs, brain, kidneys, and spleen) and to extremities, >
limb infarction. Occurs when blood turbulence within heart allow causative
agent to infect previously damaged valves or other endothelial surfaces
See Sequence of Events- Endocarditis Fig 37-3
o
Primary cause rt sided endocarditis-*IVDA- embolize to lungs
(why?)- agent -staph aureus
1
o
Lt.-sided endocarditis- patients with heart disease, bacterial
infections- embolize to brain, kidneys, spleen etc)
Infection may spread locally > damage to valves or their supporting
structures > dysrhythmias, valvular incompetence, and eventual
invasion of myocardium > heart failure (HF), sepsis, and heart block.
*Development of infective endocarditis (click to access Merck Manual)
need two conditions: (understand concept)
o
o
o
*Due to alteration (roughened areas) in endocardial surface, allows
deposition of platelet and fibrin; resulting thrombus or vegetation usually
develops in areas inc. turbulence (from roughened areas > acts as site for
bacterial attachment.
Condition of bacteremia, results in colonization of lesion…primary sites
infection include mouth, genitourinary (GU) tract (particularly after procedures
involving instrumentation), gastrointestinal (GI) tract, skin, decubitus ulcers,
surgical wounds, and IV catheters.
Some bacteria have properties (eg, certain streptococcal and
staphylococcal species have inc. adherence) > more likely to cause
infective endocarditis.
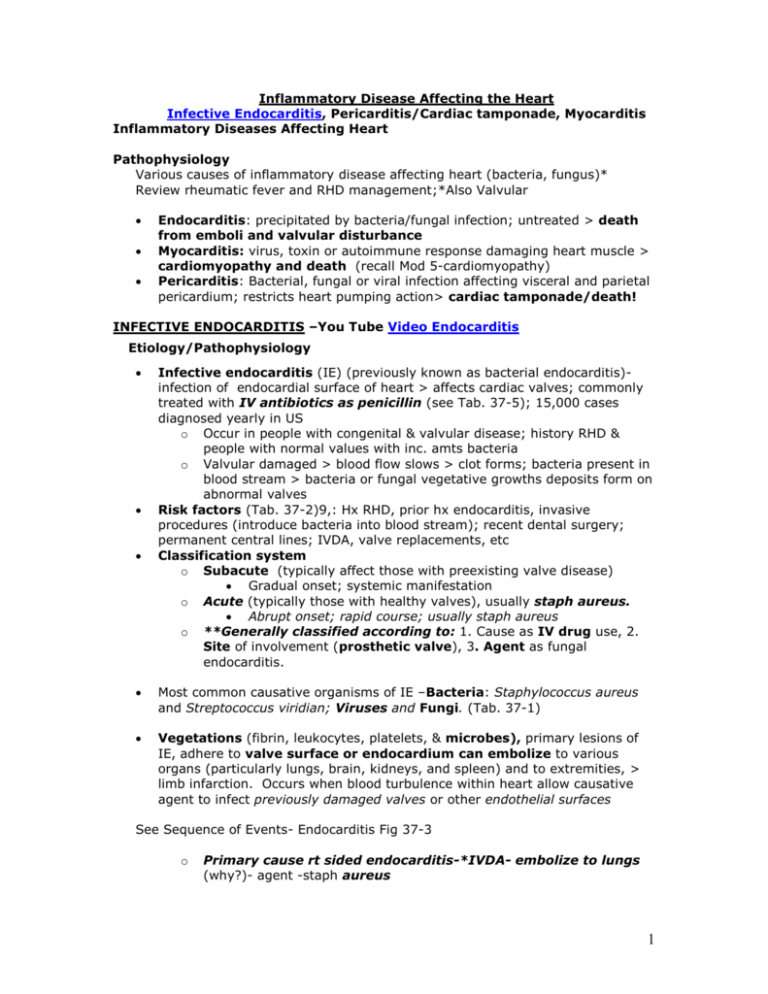
Clinical Manifestations- see also PPT slides
Nursing Assessment-Findings in IE-nonspecific; can include:
o *Low-grade fever (90% of cases), chills, weakness, malaise,
fatigue, anorexia (*Elderly- may present atypically, no fever,
unexplained anemia, large systemic emboli, renal failure, central
nervous system syndromes (eg, rapid-onset dementia, stroke)
o Arthralgias, myalgias, back pain, abdominal discomfort, weight loss,
headache, and clubbing of fingers
o Vascular finding: Splinter hemorrhages (black longitudinal streaks) in
nail beds (*recognize these)
o Petechiae- *most common (result of fragmentation/
microembolization of vegetative lesions that lodge in small vessels of
2
o
o
o
o
skin, nail beds, and mucous membranes in the conjunctivae, lips,
buccal mucosa, palate and over the ankles, feet, and the antecubital
and popliteal areas
Osler’s nodes (painful, tender, red or purple, pea-size lesions) on
fingertips or toes and Janeway’s lesions (flat, painless, small, red
spots) on palms and soles
Hemorrhagic retinal lesions called Roth’s spots
*About 40% have cutaneous or peripheral manifestations
*A new or changing murmur- aortic or mitral valve most affected;
*Tricuspid endocarditis- mumur likely absent due to lower pressure;
HF esp if aortic involvement
Osler’s nodes
Splinter hemorrhages
Janeway lesions
Roth spots
Copyright © 2007, 2004, 2000, Mosby, Inc., an affiliate of Elsevier Inc. All Rights Reserved.
Subjective data; Functional health patterns (Tab 37-6)
o Review history-previous valvular problems, immunosuppressive
therapy, etc
o Review history for IVDA, ETOH, etc.
Complications- refer to above
o Emboli (right and left sided) know why each occurs;
o HF
o Dysrhythmia (a-fib most common)
o Death
Collaborative Care
Note- Fungal & prosthetic valve endocarditis
o Respond poorly to antibiotics
o Valve replacement –adjunctive procedure
Diagnostic Studies
History IVDA, recent surgical procedure, etc
*Blood cultures-2 blood cultures, 30 minutes apart, 90% positive (unless
antibiotics within past 2 weeks) *Accurate organism ID- critical
o *Remember- blood cultures prior to start of antibiotics
*Elevated WBC, ESR, C-reactive protein
*Definitive diagnosis of IE if two of following major criteria present:
o positive blood cultures
o **new or changed cardiac murmur
3
o intracardiac mass or vegetation noted on echocardiography
o Serologic immune testing for circulating antigens
o Monitor BUN, creatinine with use of antibiotics necessary in treatment
Echocardiogram-TEE-best to view vegetations on valves
Medications Tab. 37-5 & 37-4 *conditions requiring antibiotics
*Key-accurate identification of organism when IE present
o *Prophylactic antibiotic therapy recommended for “high risk”
patients (Tab 37-3 and 4): those with mechanical or natural
prosthetic heart valves; prior infective endocardititis; valve repair with
prosthetic material; most congenital heart diseases and prior to
o Removal/drainage of infected tissue; renal dialysis, or having
ventriculoatrial shunts for management of hydrocephalus.
*Drug therapy- usual need long-term IV antibiotics & subsequent
blood cultures-evaluate effectiveness of antibiotic therapy & monitor
therapeutic blood levels (Tab. 37.5) may need IV abx 4-8 weeks, correct
drug; *monitor renal function (BUN, creatinine); oral antibiotics rare!
Fever-use aspirin, acetaminophen (Tylenol), ibuprofen (Motrin), fluids, rest.
Prosthetic valve endocarditis (PVE) and fungal endocarditis-need
o Valve replacement
o Prolonged antibiotic therapy (6 weeks or more- IV)
Surgical/Therapeutic/Nursing Interventions
As above-early valve replacement plus prolonged (6 weeks or longer)IV drug therapy recommended for patients with fungal infection and
prosthetic valve endocarditis (Tab 37-5). *Know types antibiotics
Complete bed rest - not uless temp remains elevated or signs HF
Overall goals
normal or baseline cardiac function
performance of activities of daily living (ADLs) without fatigue
knowledge of therapeutic regimen to prevent recurrence of
endocarditis.
o Priority Nursing Diagnosis
o Decreased cardiac output
o Activity intolerance
o Hyperthermia
o Risk for Ineffective Tissue Perfusion-emboli
o Deficient knowledge
Priority Teaching
o *Signs/symptoms of life-threatening complications of IE, as cerebral
emboli, HF etc.
o *Monitor fever (chronic or intermittent)- sign that drug therapy
ineffective
o *Monitor lab data and blood cultures- determine effectiveness
of antibiotic therapy
o *Critical-prophylactic antibiotic therapy prior to invasive procedure
Teaching/Evaluation
o Recognize signs/symptoms of life-threatening complications of
IE, such as cerebral emboli (e.g., change in mental status), pulmonary
edema (e.g., dyspnea), and HF (e.g., chest pain).
o Fever (chronic or intermittent)- common early sign drug therapy
4
ineffective
o Follow-up monitoring lab data and blood cultures Prevention
o Eliminate risk factors
o Patient teaching
o Penicillin prophylaxis
o Note-not all require prophylaxis- high risk only (Tab 37-3, 4)
If have prosthetic valve
History of endocarditis
Certain congenital heart defects
Heart transplant recipients
Removal or drainage of infected tissue
Renal dialysis
Ventriculoatrial shunts
__________________________________________________________________
ACUTE PERICARDITIS/Pericardial Effusion/Cardiac Tamponade
Click for YouTube Pericardiditis and Cardiac Tamponade
Etiology/Pathophysiology
Pericarditis- an inflammation of the pericardial sac, the thin, fluid filled
sac surrounding the heart > severe chest pain, esp upon taking a deep
breath/ shortness of breath. (Tab 37-7)
o Infectious- viral (Coxsackievirus B, etc), bacterial
o Noninfectous- as uremia, acute MI, neoplasm, acute MI. etc
o
Hypersensitive or autoimmune (Dressler’s –Syndrome) post MI,
rheumatic fever, drug reaction, etc.)
Acute pericarditis - often idiopathic; can be due to uremia (40-50%
patients with uremia develop), viral or bacterial infection, acute myocardial
infarction (MI), tuberculosis, neoplasm, trauma (as above).
Pericarditis- in acute MI , may be described as two distinct syndromes:
o
Acute pericarditis ( within initial 48 to 72 hours after MI)
o
Dressler syndrome (late pericarditis - 4 to 6 weeks after MI).
*Heart loses natural lubrication (15-20cc’s) > layers roughen/rub;
damage to pericardial tissue >inflammation/ inc. capillary permeability >
plasma proteins seep into pericardial space forming exudates **
Scar tissue or adhesions may form between pericardial layers; chronic
inflammation > pericardium > rigid > Chronic Pericarditis.
Clinical Manifestations
5
Findings include:
o Progressive, frequently severe sharp chest pain, worse on deep
inspiration, esp. when lying supine: *pain relieved by sitting,
leaning forward -moves heart away from diaphragmatic side of
the lung pleura- (pericardial friction rub). *Understand this! Pain
NOT related to lack of O2
o Pain referred to trapezius muscle (shoulder, upper back).
o *Hallmark finding in acute pericarditis- pericardial friction rub
(click to hear); leathery grating sound due to inflamed layers rubbing
together; heard best at left lower sternal border/client
sitting/leaning forward during expiration.
**Complications- pericardial effusion and cardiac tamponade.
o Pericardial effusion- Abnormal collection of fluid in pericardial space
> impairs normal cardiac function; fluid may be pus, blood, serum,
lymph or combination: rate of effusion development effects
manifestations: (Why significant??)
Slow build up > no immediate effects- usually 250 cc before
reflected on x-ray
Pulmonary effusion; cough, dyspnea, hiccups with phrenic
nerve compression
*If rapid buildup > compression of heart by fluid > interfere
with myocardial function > lead to life threatening cardiac
tamponade
o **Cardiac tamponade- (*Medical emergency when develops
rapidly) as above- due to rapid collection of fluid > interferes with
ventricular filling, pumping, reducing cardiac output; *know
manifestations
Chest pain, cough, mild dyspnea
*Paradoxical pulse (pulsus paradoxus): pulse marked dec.
in amplitude during inspiration; also indicated by drop in
systolic blood pressure of more than 10 mm HG during
inspiration (Tab 37-8) *Know steps to measure a pulsus
paradoxus
*Distant, muffled heart sounds
Dyspnea, tachypnea, tachycardia
Narrowed pulse pressure
*Elevated CVP
*Distended neck veins
6
In medicine, pulsus paradoxus (PP), also paradoxic pulse and
paradoxical pulse- exaggeration of normal variation in pulse during
inspiratory phase of respiration, which pulse becomes weaker as one
inhales and stronger as one exhales; sign that is indicative of several
conditions including cardiac tamponade, pericarditis, chronic sleep
apnea, etc
In pulsus paradoxus …on clinical examination… detect beats on
cardiac auscultation during inspiration that cannot be palpated at the
radial pulse…due to an accentuated dec. of blood pressure >leads to
(radial) pulse not being palpable… may be accompanied by inc. in
jugular venous pressure…Also as usual with inspiration, the heart rate
is slightly inc. due to dec. left ventricular output.
**Mechanism of reduced blood pressure during inspiration in
normal conditions (understand this)
During inspiration, systolic blood pressure dec. slightly, pulse rate goes up
slightly…as intrathoracic pressure becomes more negative relative to
atmospheric pressure. This inc. systemic venous return, so more blood flows
into right side of heart. However, the dec. in intrathoracic pressure also
expands the compliant pulmonary vasculature. This inc. in pulmonary blood
capacity pools blood in the lungs, and decreases pulmonary venous return, so
flow is reduced to left side of the heart. Reduced left-heart filling leads to a
reduced stroke volume which manifests as a decrease in systolic blood
pressure. The decrease in systolic blood pressure leads to a faster heart rate
due to the baroreceptor reflex, which stimulates sympathetic outflow to
Measurement of PP
PP is quantified using a blood pressure cuff and stethoscope, by measuring
variation of the pressure in systole with respiration. Normal systolic blood
pressure variation (with respiration) is considered to be ≤10 mmHg. Pulsus
paradoxus is an inspiratory reduction in systolic pressure >10 mmHg. Pulsus
paradoxus can also be measured by listening to Korotkoff sounds during blood
pressure measurement -- slowly decrease cuff pressure to the systolic
pressure level where sounds are first heard. Then, cuff pressure is slowly
lowered further until Korotkoff sounds are heard throughout the respiratory
cycle. If the pressure difference between hearing the first sounds and hearing
them throughout the respiratory cycle is >10mmHg, it can be classified as
pulsus paradoxus.
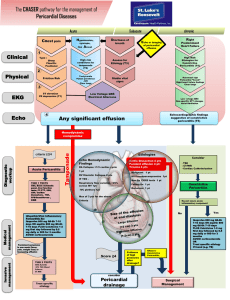
Collaborative Care (Tab 37-9)
Diagnostic Studies -Pericarditis/Pericardial effusion/Tamponade
ECG monitoring- distinguishing ischemic pain from pericardial pain
(ischemia involves localized ST-segment changes; diffuse ST-segment
changes in acute pericarditis)
Chest X-Ray (cardiomegaly if large pericardial effusion)l
ECHO important esp. for cardiac tamponade
Labs elevated CRP, ESR etc; analysis fluid from pericariocentesis (remove
fluid with effusion/tamponade), biopsy
Medications
Acute Pericarditis
7
*Pain and anxiety management during acute pericarditis- primary nursing
consideration.
*Pain relief- Bed rest-HOB elevated to 45 degrees; overbed table for
support; leaning forward reduces pain (moves away from
diaphragmatic side of the lung pleura)
o
o
o
Corticosteroids for pericarditis secondary to systemic lupus
erythematosus, patients already taking corticosteroids for a
rheumatologic or other immune system condition, or patients who do
not respond to nonsteroidal antiinflammatory drugs (NSAIDs)
Pain and inflammation-usually treated with NSAIDs or high-dose
salicylates (e.g., aspirin).
Colchicine, an antiinflammatory agent used for gout, may be
considered for patients who have recurrent pericarditis.
Surgical/Therapeutic/Nursing (*Important (Fig 37-6)
Tamponade/Purulent Pericarditis/Pericardial Effusion
o **Pericardiocentesis- performed for pericardial effusion with acute
cardiac tamponade, purulent pericarditis, and a high suspicion of
a neoplasm. *Read how this is done
Complications -pericardiocentesis include dysrhythmias,
further cardiac tamponade, pneumomediastinum,
pneumothorax, myocardial laceration, and coronary artery
laceration
Careful monitoring for dysrhythmias etc .
o *Pericardial Window: excision of rectangular piece of pericardium to
allow fluid to drain into pleural space if recurrent pericarditis or
effusion (not in text)
CHRONIC CONSTRICTIVE PERICARDITIS
Etiology/Pathophysiology
Due to scarring with consequent loss of elasticity of pericardial sac; begins
with initial episode of acute pericarditis followed by fibrous scarring,
thickening of pericardium from calcium deposition, and eventual obliteration
of pericardial space
End result-fibrotic, thickened, and adherent pericardium impairs
ability of atria and ventricles to stretch adequately during diastole.
Clinical Manifestations
Findings:
o Mimic HF and cor pulmonale - include dyspnea on exertion,
peripheral edema, ascites, fatigue, anorexia, and weight
o Most prominent finding- jugular venous distention
o Auscultation- *pericardial knock (click to hear loud early diastolic
sound often heard along left sternal border)
Collaborative Care
Diagnostic Studies
See Diagnostic studies pericardial effusion
2D ECHO confirm restrictive. Also CT amd MRI to confirm
Medications/Medication/Surgery
Treatment of choice – pericardiectomy-involves complete resection of
pericardium through a median sternotomy with use of cardiopulmonary
bypass.
8
Summary Nursing Care/Nursing Diagnoses Pericardidits etc (not in text)
Acute Pain
Ineffective Breathing Pattern
Risk for Decreased Cardiac Output
Activity Intolerance
Knowledge deficit: regarding anti-inflammatory medications; activity
restriction; manifestations of recurrent pericarditis and seeking treatment
Keys
Inflammatory conditions of the heart can be life threatening, cause death
Management depend upon etiology and disease manifestation
Surgery and in some cases, even transplant of heart may be required
_________________________________________________________________
MYOCARDITIS (Click to open YouTube video)
Etiology/Pathophysiology
*Focal or diffuse inflammation of myocardium caused by viruses,
bacteria, fungi, radiation therapy, and pharmacologic and chemical factors.
*Infection in muscles of heart, most commonly caused by the Coxsackie B virus post
respiratory or viral illness, bacteria and other infectious agents.
Frequently associated with acute pericarditis, esp. when caused by coxsackie
virus B strains.
Results in cardiac dysfunction; * linked to development of *dilated
cardiomyopathy.
More common with altered immunity (10% HIV clients develop this)
Viral myocarditis usually self-limiting-can become chronic > lead to
*dilated cardiomyopathy (see Mod 5)
Extent of damage determines outcome*; may have localized involvement to
one area of heart or may affect entire heart
Risk factors: URI, toxic or chemical effects (radiation, alcohol);
*autoimmune; metabolic disturbance-lupus; heat stroke or hypothermia & a
complication of pericarditis and rheumatic fever
Clinical Manifestations
Findings:
o Fever, fatigue, malaise, myalgias, pharyngitis, dyspnea,
lymphadenopathy, and nausea and vomiting are early systemic
manifestations of the viral illness.
o Early cardiac manifestations appear 7 to 10 days after viral
infection, include
pleuritic chest pain with a pericardial friction rub and effusion.
9
Late cardiac signs relate to development of HF, may include
S3 heart sound, crackles, jugular venous distention, syncope,
peripheral edema, and angina.
Risk for sudden death
o
Collaborative Care
Diagnostic Studies
EKG changes non-specific
Various lab include- ESR, CRP, elevated myocardial markers, etc
*Histologic confirmation by EMB
**Endomyocardial biopsy (EMB) for definitive diagnosis-show patchy
cell necrosis and inflammatory process
Medications/Surgery/Nursing
Keys meds to manage cardiac decompensation/HF with:
o Digoxin (Lanoxin)- treat ventricular failure
o Diuretics- reduce fluid volume and decrease preload
o Nitroprusside (Nitropress), inamrinone (Inocor), and milrinone
(Primacor) to reduce afterload and improve cardiac output
o **Use of anticoagulation therapy- considered in patients with a
low ejection fraction who are at risk for thrombus formation due to
blood stasis in cardiac chambers.
o *Immunosuppressive therapy to reduce myocardial
inflammation and to prevent irreversible myocardial damage.* To
eradicate infecting organism, including interferon-alpha for virus
(antibiotics, antiviral with interferon-a)
o *Oxygen therapy, bed rest, and restricted activity- may be
required for 3-6 months**.
o Intra-aortic balloon pump therapy and ventricular assist devices (if
heart failure)
Nursing interventions focus on assessment for signs/symptoms of HF
o
assessing level of anxiety
o
instituting measures to decrease anxiety
o
keeping patient and family informed about therapeutic measures.
o Goal Decrease workload of heart-allow to heal!!
*Most patients with myocarditis recover spontaneously, some may
develop dilated cardiomyopathy
Home Care- teach activity restriction; recognition early manifestations heart
failure; medications, diet modifications; follow-up with medical care
Nursing Diagnosis
o Activity Intolerance
o Decreased CO
o Anxiety
o Excess fluid volume
RHEUMATIC FEVER AND HEART DISEASE (read/review not on exam)
Rheumatic fever is an inflammatory disease of the heart potentially involving all
layers of the heart.
Rheumatic heart disease is a chronic condition resulting from rheumatic fever that
is characterized by scarring and deformity of the heart valves.
Acute rheumatic fever (ARF) is a complication that occurs as a delayed sequela of a
group A streptococcal pharyngitis and affects the heart, joints, central nervous system
(CNS), and skin.
About 40% of ARF episodes are marked by carditis, meaning that all layers of the
heart are involved, and this is referred to as rheumatic pancarditis.
10
o
o
o
o
Rheumatic endocarditis is found primarily in the valves. Vegetation forms and
valve leaflets may fuse and become thickened or even calcified, resulting in
stenosis or regurgitation.
Myocardial involvement is characterized by Aschoff’s bodies.
Rheumatic pericarditis affects the pericardium, which becomes thickened and
covered with a fibrinous exudate, and often involves pericardial effusion.
The lesions of rheumatic fever are systemic, especially involving the
connective tissue, as well as the joints, skin, and CNS.
Clinical manifestations of ARF include the following:
o The presence of two major criteria or one major and two minor criteria plus
evidence of a preceding group A streptococcal infection.
Major criteria:
Carditis results in three signs: (1) murmurs of mitral or aortic
regurgitation, or mitral stenosis; (2) cardiac enlargement and HF;
(3) pericarditis.
Mono- or polyarthritis causes swelling, heat, redness, tenderness,
and limitation of motion.
Chorea (Sydenham’s chorea) involves involuntary movements,
especially of the face and limbs, muscle weakness, and
disturbances of speech and gait.
Erythema marginatum lesions are bright pink, nonpruritic, maplike
macular lesions that occur mainly on the trunk and proximal
extremities.
Subcutaneous nodules are firm, small, hard, painless swellings
located over extensor surfaces of the joints.
Minor criteria:
Clinical findings: fever, polyarthralgia
Laboratory findings: elevated ESR, elevated WBC, elevated
CRP
Complications of ARF include chronic rheumatic carditis.
Skin should be assessed for subcutaneous nodules and erythema marginatum.
The overall goals for a patient with rheumatic fever include (1) normal or baseline
heart function, (2) resumption of daily activities without joint pain, and (3)
verbalization of the ability to manage the disease.
Health promotion emphasizes prevention of rheumatic fever by early detection and
treatment of group A streptococcal pharyngitis with antibiotics, specifically penicillin.
o The success of treatment requires strict adherence to the full course of
antibiotic therapy.
o The primary goals of managing a patient with ARF are to control and eradicate
the infecting organism; prevent cardiac complications; and relieve joint pain,
fever, and other symptoms with antibiotics; optimal rest; and antipyretics,
NSAIDs, and corticosteroids.
o Secondary prevention aims at preventing the recurrence of rheumatic fever
with monthly injections of long-acting penicillin. Additional prophylaxis is
necessary if a patient with known rheumatic heart disease has dental or
surgical procedures involving the upper respiratory, GI (e.g., endoscopy), or
GU tract.
Expected outcomes for patient with rheumatic fever and heart disease include (1)
ability to perform ADLs with minimal fatigue and pain, (2) adherence to treatment
regimen, and (3) expression of confidence in managing disease.
11