NOTES Mod #6 Inflammatory
advertisement

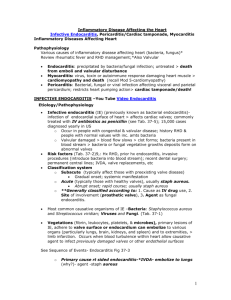
NOTES Mod #6 Inflammatory Endocarditis/Myocarditis/Pericarditis Cardiac Tamponade cmj Inflammatory Disease affecting the Heart Etiology/Pathophysiology (general) A. Pathophysiology 1. Various causes of inflammatory disease affecting heart (bacteria, fungus)* Review rheumatic fever and RHD management) a. Endocarditis: precipitated by bacteria/fungal infection; untreated lead to death from emboli and valvular disturbance b. Myocarditis: virus, toxin or autoimmune response damaging heart muscle> lead to cardiomyopathy and death! c. Pericarditis: Bacterial, fungal or viral infection affecting visceral and parietal pericardium; restricts heart pumping action> lead to cardiac tamponade and death! Endocarditis (Infective) A. Etiology/Pathophysiology: 1. Pathogens: enter bloodstream through dental work, invasive procedures> vegetation forms on damaged endothelium a. Organisms colonize vegetations> become covered with platelets and fibrin b. Friable vegetations break off> *embolize> travel through blood stream to other organ systems c. Emboli lodge in small vessels > hemorrhages, infarcts, abscesses** d. *Vegetation scars, deforms valves > causes turbulent blood flow through heart 2. Classifications (See p. 891, Tab 30-5) a) Acute infective endocarditis 1) Abrupt onset, rapidly progressive severe disease 2) Staphylococcus aureus most common infective organism (associated usually with IV drug use) RNSG 2432 141 b) Subacute infective endocarditis 1) Gradual onset; systemic manifestation 2) Occurs with preexisting heart disease 3) Organisms include Streptococcus viridans, enterococci, yeasts, fungi c) Prosthetic valve endocarditis (PVE) (generally 2 mo after surgery; esp aortic valve) 1) Early onset usually due to contamination during surgery or preoperative bacteremia;has high mortality rate 2) Late onset similar to subacute endocarditis 3. Risk factors a. Previous heart damage as deformed valves, valve prostheses, areas of heart damaged by congenital or ischemic disease (left sided valves, especially mitral); history rheumatic fever! (Subacute) b. *Intravenous illicit drug use (right sided valves usually affected): why? Due to IV site injection > travel to rt side of heart (Acute) c. Invasive catheters (central venous lines, indwelling urinary catheters) d. Dental procedures, poor dental health e. Recent heart surgery B. Common Manifestation/Complications 1. Temperature above 101.5o F. (39.4o C); flulike symptoms (cough, shortness of breath, joint pain); esp acute endocarditis; blood cultures required! 2. Acute staphylococcal endocarditis; may present with sudden onset of chills. high fever 3. Heart murmurs occur (new or worsening)…occurs in 90% of all cases…** 4. *Embolic complications (Recall why this happens!) a. Splenomegaly with chronic disease b. Peripheral manifestations due to microemboli (some findings significant, others not) 1) Petechiae 2) Splinter hemorrhages (hemorrhagic streaks under finger or toenails) 3) Osler’s nodes: small, reddened painful raised growths on finger and toe pads 4) Janeway lesions: small nontender purplish red macular lesions on palms of hands or soles of feet 5) Roth’s spots, small whitish spots seen on retina 142 RNSG 2432 Osler’s nodes: small, reddened, painful growths, finger and toe pads Janeway lesion, nontender on palms of hand, soles of feet Splinter hemorrhages Roth’s spots (cotton wool) seen on retina 5. Complications include heart failure, organ infarction a. RT emboli (50% break off; have septic clots 1) Right sided endocarditis develop pulmonary emboli 2) Left sided emboli affect brain, spleen, heart and limbs b. CHF c. Arrhythmia (a-fib most common) d. Death e. Cardiac tamponade C. Therapeutic Interventions/Collaborative Care 1. Diagnostic tests: *Identify, eradicate infected organism with antibiotics; minimizing valve damage and complications a. Blood cultures: considered positive if infecting organism identified from 2 or more separate blood cultures (different sites, different times); temp above 101 drawn from different sites, different times) (Recall how blood cultures done!) b. WBC, ESR for elevations; dec. HCT and HGB c. Echocardiography: visualization of vegetations and eval. of valve function; TEE visualization of vegetation d. Serologic immune testing: test for circulating antigens e. Monitor Bun, creatinine with use of antibiotics necessary in treatment 2. Medications (*understand reason why!) a. *Antibiotic prophylaxis-for pre-existing valve damage or heart disease prior to high risk procedures b. *Infective endocarditis involves extended course of multiple intravenous antibiotics (2 – 8 weeks); repeat blood cultures c. *Prosthetic valve endocarditis includes extended treatment (6 – 8 weeks) with combination of antibiotics 3. Surgery a. Surgery may be part of treatment RNSG 2432 143 1) replace damaged valve 2) remove large vegetation 3) remove valve if source of infection/not responding to antibiotics b. *Surgery usually indicated for clients with valvular regurgitation causing heart failure -not responding to antibiotic therapy; also for fungal endocarditis 4. Nursing Diagnoses (p. 893-894) a. Risk for Imbalanced Body Temperature b. Risk for Ineffective Tissue Perfusion c. Ineffective Health Maintenance d. Knowledge deficit include: use of medications/need to complete therapy/ need to notifying health practitioners of need for *prophylaxis with all invasive procedures (penicillin) ; need for dental care and hygiene and follow-up with physician (understand this) ______________________________________________________________ Myocarditis A. Etiology/Pathophysiology: 1. Inflammation of heart muscle from infectious process, immunologic response to radiation, toxins, medications 2. Due to Coxsakie B virus** (in US) 3. More common with altered immunity (10% HIV clients develop this) 4. Dec. contractitility 5. Viral myocarditis usually self-limiting-can become chronic > lead to *dilated cardiomyopathy 6. Myocardial cells damaged by inflammation and invading pathogens 7. Extent of damage determines outcome* 8. Risk factors: URI, toxic or chemical effects (radiation, alcohol); autoimmune; metabolic disturbance-lupus; heat stroke or hypothermia & a complication of pericarditis and rheumatic fever •This is an infection in the muscles of the heart, most commonly caused by the Coxsackie B virus that follows upon a respiratory or viral illness, bacteria and other infectious agents. 144 RNSG 2432 View of transverse section of heart from above. •Note area of myocardial pallor (2 arrows) mostly to the left of the left ventricular cavity involving less than 1/2 of the wall thickness…due to a dense interstitial infiltrate of inflammatory cells. •The normal appearing red myocardium elsewhere could also show microscopic infiltrates, which are not dense enough to see grossly Patho (click here for more information) B. Common Manifestation/Complications 1. Dependent on degree of myocardial damage; from asymptomatic to heart failure 2. Non-specific: fever, fatigue, general malaise, dyspnea, palpitations, arthralgias (may be preceded by nonspecific febrile illness or upper respiratory infection) 3. Heart sounds: muffled S1, S3, murmur, pericardial friction rub, tachycardia 4. **Manifestations of heart failure, chest pain, maybe MI, signs CHF, arrhythmia C. Therapeutic Interventions/Collaborative Care 1. Diagnostic tests: a. Electrocardiography: may show ST segment and T wave changes, dysrhythmias, possible heart block b. Cardiac markers (Creatinine kinase, troponin T and I) may be elevated c. Endomyocardial biopsy for definitive diagnosis-show patchy cell necrosis and inflammatory process 2. Medications a. To eradicate infecting organism, including interferon-alpha for virus (antibiotics, antiviral with interferon-a) b. Immunosuppressive therapy- corticosteroids & others c. Other medications for symptoms:heart failure drugs including ACE inhibitors, beta blockers, antiarrhythmics if indicated; anticoagulants, to prevent emboli d. Bedrest and restricted activity during the acute inflammatory process; may be limited 3- 6 months (Very imortant!!)…why? (see p. 895) 3. Nursing diagnosis/Nursing Care a. Nursing Care focus: dec. myocardial work; maintain cardiac output b. Nursing Diagnoses (See p. 895) 1) Activity Intolerance 2) Decreased Cardiac Output 3) Fatigue 4) Anxiety 5) Excess Fluid Volume 6) Knowledge Deficit a) Home Care_ teach activity restriction; recognition early manifestations heart failure; medications, diet modifications; follow-up with medical care RNSG 2432 145 ______________________________________________________________ Pericarditis and Cardic Tamponade A. Etiology/Pathophysiology: 1. Inflammation of pericardium (may be 1st or 2nd to other cardiac/systemic disorders 2. Types: acute (usually viral in nature, bacterial or fungal) or chronic a. *Result from end-stage renal disease and uremia, post-MI, post open heart surgery b. Heart loses natural lubrication (15-50cc’s) > layers roughen and rub c. Damage occurs to pericardial tissue > lead to inflammation d. Increased capillary permeability and plasma proteins seep into pericardial space forming exudates** e. Scar tissue or adhesions may form between pericardial layers 3. Chronic inflammation > cause** pericardium to become rigid. 4. Risk factors: Post MI (Dressler’s syndrome); secondary to chemo and cancer; secondary to uremia in renal failure-(40-50% of ESRD pts. develop this); trauma or cardiac surgery B. Common Manifestation/Complications (know this!) 1. **Chest pain: aggravated by respiratory movement, changes in body position; sitting upright, leaning forward may reduce the pain (moves the heart away from side of lung pleura)! 2. Typically has abrupt onset; sharp, steady or intermittent pain, may radiate to back or neck! (acute) 3. Pericardial friction rub: leathery grating sound produced by inflamed layers rubbing together; heard most clearly at left lower sternal border with client sitting and leaning forward during expiration Pericardial Friction Rub (Go here to auscultate a pericardial friction rub) 146 RNSG 2432 Hear a typical friction rub-caused by the beating of the heart against inflamed pericardium or lung pleura; various etiologies. Sound usually continuous, heard diffusely over chest. Typically has three components, one systolic and two diastolic. Systolic occurs with ventricular contraction, diastolic occurs during both rapid ventricular filling and atrial contraction; accentuated when patient sits up, leans forward, may be accentuated during inspiration. If rub completely disappears when patient holds his breath it is more likely due to pleural, not pericardial, origin. 4. Fever (low grade) with dyspnea and tachycardia (less than 100) 5. Complications a. Pericardial effusion Heart huge due to fluid in pericardial space 1) Abnormal collection of fluid in pericardial space> threatens normal cardiac function 2) Fluid may be pus, blood, serum, lymph or combination 3) Rate at which effusion develops effects manifestations: (Why is this significant??) a) Slow build > no immediate effects b) **Rapid buildup > compress heart interfer with myocardial function (tamponade) c) May have distant or muffled heart sounds, cough, mild dyspnea b. Cardiac tamponade (*Important!) RNSG 2432 147 1) Medical emergency; rapid collection of fluid> interferes with ventricular filling, pumping, reducing cardiac output 2) Manifestations (know this!) a) Paradoxical pulse (pulsus paradoxus): pulse has marked decrease in amplitude during inspiration b) Paradoxical pulse indicated by drop in systolic blood pressure of more than 10 mm HG during inspiration c) Distant, muffled heart sounds d) Dyspnea and tachypnea e) Narrowed pulse pressure f) Elevated CVP g) Distended neck veins c. Chronic Constrictive Pericarditis Results from chronic pericarditis 1) Scar tissue forms between pericardial layers >restricts heart movement and filling 2) May follow viral infection, radiation therapy, heart surgery 3) Manifestations: dyspnea; fatigue, weakness; ascites; neck vein distension during inspiration (Kussmaul’s sign) C. Therapeutic Interventions/Collaborative Care (relieve symptoms; prevent complications) 1. Diagnostic tests: a. Differentiate from MI: CBC and ESR: Elevated WBC and ESR reflect acute inflammation b. Cardiac enzymes: elevation is lower than with MI c. Electrocardiography (ECHO): diffuse ST segment elevation in all leads; resolves more quickly than with MI; Q waves and T wave changes found with MI not present d. Echocardiography: assesses heart motion, pericardial effusion; any restricted movement 148 RNSG 2432 e. Hemodynamic monitoring: assesses pressures, cardiac output f. Chest xray: cardiac enlargement if pericardial effusion is present g. CT scan or MRI: identify effusion or constrictive pericarditis 2. Medications a. Aspirin or acetaminophen to reduce fever b. NSAIDS for comfort c. Corticosteroids for severe or recurrent pericarditis 3. Surgery/Other a. Pericardiocentesis: Removal of fluid from pericardial sac for diagnostic or therapeutic purposes; needle insertion into pericardial sac and withdrawal of fluid; emergency procedure for *cardiac tamponade Cardiac monitoring during procedure; catheter to V lead b. Surgery 1) Pericardial Window: excision of rectangular piece of pericardium to allow fluid to drain into pleural space if recurrent pericarditis or effusion RNSG 2432 149 A procedure in which an opening is made in the pericardium to drain fluid that has accumulated around the heart. A pericardial window can be made via a small incision below the end of the breastbone (sternum) or via a small incision between the ribs on the left side of the chest. 2) Partial or total pericardectomy with constrictive pericarditis 4. Nursing Care/Nursing Diagnoses Pericardidits (p. 898) a. Acute Pain b. Ineffective Breathing Pattern c. Risk for Decreased Cardiac Output d. Activity Intolerance e. Knowledge deficit: regarding anti-inflammatory medications; activity restriction; manifestations of recurrent pericarditis and seeking treatment Summary Inflammatory conditions of the heart can be life threatening, cause death Management will depend upon etiology and disease manifestation Surgery and in some cases, even transplant of the heart may be required. General nursing (during acute phase) care includes: O2 Bedrest Positioning Space Activities Prevent complications of immobility Psychological support 150 RNSG 2432