Dr. Samir Matloub Acid peptic diseases include: gastroesophageal
advertisement

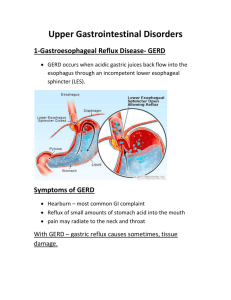
Dr. Samir Matloub Acid peptic diseases include: gastroesophageal reflux disease (GERD), peptic ulcers (DU & GU) and stress related mucosal injury. Acid and pepsin versus mucosal resistance: peptic ulcers are produced when the balance between (acid and pepsin) and the mucosal resistance is disturbed (i.e. the balance between the aggressive factors and the defensive mechanisms is disturbed). This is usually either by ↑aggressiveness or ↓mucosal resistance. Usually the ↓in the mucosal resistance is the predisposing factor. Both genetic and environmental factors play an important role in the causation of ulcers… environmental factors include: 1. Helicobacter pylori infection (over 90% of peptic ulcers are caused by infection with this organism) 2. NSAID 3.Smoking Factors protecting the mucosa: 1. Ability to secrete mucus and bicarbonate ion (HCO3). 2. Impermeability to H+ by the tight junctions between the mucosal cells and their lipo-protein layers. 3. Blood flow (microvasculature) of mucosa. 4. Capacity of quick replacement of the damaged epithelial cells PGs play a critical role in the protection of mucosa. 1 P cells + G cells Gastrin + Histamine ECL _ _ Somatostatin D cells (Oxyntic mucosa) Somatostatin D cells (Pyloric mucosa) Endocrine and paracrine cells that stimulate or inhibit HCl secretion From parietal cells directly or indirectly Ach M3 Hist. PGE H2 PGE ̶ cAMP + IP3 CCK-B Ca+ kinase Model for regulation of the parietal cell secretion Blood gastrin Proton pump H-K ATPase + + H K Histamine is the most potent stimulant for gastric acid secretion. Histamine by stimulating H2 receptors results in activation of adenylate cyclase thus increasing cAMP which leads to activation of protein kinase which in turn will stimulate the proton pump leading to secretion of acid . ACh and gastrin on the other hand increase Ca+ and IP3, which will ↑gastric acid secretion. PGs are inhibitory; they inhibit adenylate cyclase to inhibit acid secretion. Proton pump is the final stage, so if we block it, all acid secretion whatever is the stimulus will be blocked. 2 To approach a patient with peptic ulcer: drugs can alter the balance towards healing and prevention of recurrence of ulcer in the following ways: 1. Reduction of acid secretion by: a. Histamine H2 receptor antagonists e.g.: cimetidine, ranitidine, nizatidine, and famotidine. b. Proton pump inhibitors e.g.: omeprazole, lansoprazole, pantoprazole, rabeprazole, and esomprazole. c. Antimuscarinic drugs: e.g.: pirenzepine, and telenzepine. 2. Neutralization of secreted acid by antacids e.g.: magnesium trisilicate, aluminum hydroxide. 3. Enhancement of mucosal resistance by: a. Protecting the base of peptic ulcer e.g.: bismuth chelate, sucralfate. b. Cytoprotection (misoprostol) a PGE1 analog. c. Eradication helicobacter pylori infection by antimicrobials (amoxicillin, metronidazole, clarithromycin and tetracycline), we use two Abcs preferably (clarithromycin and amoxicillin) + an antisecretory agent (e.g. PPI) and /or bismuth. 1. Reduction of Acid Secretion: A. Histamine H2-Receptor Antagonists: They differ in structure: Cimetidine contains imidazol ring. Ranitidine contains phenol ring. Famotidine and nizatidine contain thiazol ring. All are equally effective in producing healing; however these drugs may differ in their pharmacokinetics, potency and range of S/E. Mechanism of Action: H2 receptors are present on the parietal cells. H2 receptors blockers inhibit gastric acid secretion by competitively blocking of H2 receptors in the parietal cells; therefore, they inhibit the direct action of histamine on gastric acid secretion and inhibit the potentiating action of histamine on acid secretion stimulated by gastrin and Ach . H2-receptors blockers ↓basal acid secretion and nocturnal acid secretion more than 90% and food stimulated acid secretion by ≈70%. Both concentration and volume of H+ will ↓and the concentration of pepsin is also ↓ by the effect of H2-receptor blockers. 3 Pharmacokinetics: All of them are well absorbed after oral dose. Antacids ↓their absorption in about 10-20%. Peak serum concentration is reached within 1-2hrs. after oral dose. All cross BBB and placenta. They are excreted in milk. Bioavailability of cimetidine, ranitidine, and famotidine is decreased by 3050% by 1st pass elimination while nizatidine has no 1st pass metabolism, bioavailability of nizatidine is 90-100% (they are excreted by liver and kidney). Efficacy is the same for all, but potency differs (different doses are used). Ranitidine binds 4-10 times less avidly than cimetidine to P450. Negligible interactions occur with nizatidine and famotidine. Side Effects: They are few in short term use. Minor side effects include headache, dizziness, constipation, diarrhea, tiredness, and muscular pain. Bradycardia and cardiac conduction defects may occur after I.V. injection of cimetidine (due to blockade of H2 receptors in the heart). Cimetidine has weak anti-androgenic effect and it ↑ prolactin secretion leading to gynecomastia and sexual dysfunction in males other H2 antagonists have no anti-androgenic effects. In elderly, H2 receptor antagonists may cause CNS disturbances including lethargy, confusion, and hallucination. Nizatidine may cause pruritis and rhinitis. H2 antagonists may rarely cause blood dyscrasias and reversible abnormalities in the liver chemistry Main Uses of H2-receptor Antagonists: 1. 2. 3. 4. GERD. Peptic ulcer disease. Non-ulcer dyspepsia. Prevention of bleeding from stress related gastritis complicating burns, hepatic failure, renal failure or trauma. 5. Healing of NSAID ulcers if the NSAID is discontinued. 6. Given before emergency surgery or labor to decrease risk of aspiration pneumonia. 7. Combined with H1 blockers in the treatment of chronic urticaria 4 Cimetidine: Is a well known inhibitor of hepatic digesting oxidizing enzyme system P450, so it leads to↑ plasma level of many drugs like: warfarin, cyclosporine, Ca + channel blockers, Propranolol, theophylline, diazepam, sulfonyl ureas, TCA, and antiarrhythmic like quinidine, mexiletine, Phenytoin, and lignocaine.It also inhibits the excretion of procainamide by the renal tubules. Treatment Course: This course continues for 4-6 weeks and for gastric ulcer 6-8 weeks. B. Muscarinic Antagonists: These agents reduce basal secretion by about 50% but stimulated secretion is less affected because of the unselectivity and the many inconvenient side effects like dry mouth, blurred vision, constipation, tachycardia..etc.they are no more used. The newer selective antagonists acting on (M1 receptors) like pirenzepine, telenzepine made them more useful. These selective drugs have higher affinity for M1 receptors and less affinity to M2 and M3 receptors. M1 receptors are found in the intramural neurons and probably on the enterochromaffin like cells which are responsible for secretion of histamine. M1 receptors antagonists are used in the treatment and prevention of recurrence of peptic ulcer, but they are less effective than H2-receptors blockers. Side Effects: Are the same of atropine and selectivity is lost with increasing the dose. Usual dose is 100-150 mg/d for pirenzepine (t1/2 =11hrs), absorption from the stomach is poor and it is excreted unchanged in urine and bile. 5 C. Proton Pump Inhibitors PPI: Are omeprazole, lansoprazole, pantoprazole, rabeprazole, and esomprazole(it is the S- isomer of omeprazole) , of which omeprazole is the prototype. They act at the final stage or step of acid secretion, they inhibit the action + of H -K+ ATPase enzyme (i.e. the proton pump) found on apical membrane of parietal cells in the stomach and no other place in the body, it catalyzes the exchange of H+ and K+ in the process of acid secretion, so PPI antagonize all stimulants of acid secretions. These agents are substituted benzimidazole containing sulfinyl group, they are lipophilic weak bases. At neutral PH, PPIs are chemically stable and are devoid of inhibitory activity (prodrugs). After intestinal absorption, they reach the parietal cells from the blood and when they are in the canaliculi of parietal cells they become active where PH is about 1. In the canaliculi they are protonated to form a cationic sulfinamide which forms covalent bonds with the sulfhydryl group at critical sites of the enzyme, they form a complex called (cystinyl sulfinamide complex) and this step will irreversibly block the pump. Omeprazole produces a profound and long lasting enzyme inhibition of both basic and stimulated acid secretion, this is probably irreversible. Single dose of 20mg of omeprazole decreases acidity by about 90% over 24hrs. PPIs have minor direct anti-helicobacter properties. Pharmacokinetics of PPIs: Omeprazole must be given in enteric-coated formulations(capsules or tablets), for it is degraded at low PH, t1/2=1.5hr, peak plasma level is reached within 2-3hrs and the metabolite is inactive and excreted in the urine. It's metabolized by cytochrome P450 oxidase. Omeprazole is also available as a nonenteric coated powder that contain NaHco3 that becomes immediate release suspension when mixed with water,it is given by mouth or through entral tube resulting in rapid absorption and rapid onset of acid inhibition. Lansoprazole is also available as tablet formulation that disintegrates in the mouth or maybe mixed with water and administrated via oral syringe or oral tube. Esomprazole, lansoprazole, pantoprazole are also available as I.V formulation. Rabeprazole due to its high PKa also have faster onset of acid inhibition. 6 Up to 3 – 4 days of daily medication are required before the full acid inhibiting potential is reached. Similarly after stopping the drug 3-4 days are also needed to regain full acid secretion. The bioavailability of these agents is decreased by 50% by food hence these drugs should be administrated 1hr before meals. PPIs are inhibitors of P450 oxidase too, but less than cimetidine (pantoprazole, rabeprazole have no significant interactions) . The dose of PPIs should be reduced in patients with severe hepatic disorders while compromised renal function patients are not affected by PPIs. Uses of PPIs: 1. Duodenal and benign gastric ulcer. 2. Reflux esophagitis better than H2-blockers. 3. They are drugs of choice for hypersecretory conditions such as gastrinomas and the Zollinger-Ellison syndrome. 4. They are drugs of choice for ulcers produced by NSAID, they can produce healing inspite of continuation of the NSAIDs. It is also used to prevent NSAID ulcers and their complication. 5. Prevention of rebleeding from peptic ulcer. 6. Prevention of stress related mucosal bleeding. 7. Non-ulcer dyspepsia. Side Effects: they are extremely safe Nausea, vomiting, headache, diarrhea, constipation, abdominal pain and rash occur but usually are uncommon. PPIs may impair the absorption of vit. B12, calcium, zinc, and iron. Omeprazole inhibits metabolism of warfarin, Phenytoin and diazepam but much less than cimetidine. Potential problems due to suppression of acid secretion by PPIs: 1. Suppression of acid secretion →↑gastrin release →leads to hyperplasia of enterochromaffin cells →carcinoid tumors may develop (this has not been documented in human).also hypergastrinemia leads to increased colonic mucosal proliferation potentially promoting carcinogenesis (also not documented in humans) 7 2. Decreased gastric acidity (prolonged hypochlorhydria) →bacterial overgrowth in the stomach → these bacteria convert the ingested nitrates into carcinogenic nitrites and N-nitroso amines. This has been demonstrated in animals but not in human so they are safe to be used. 3. Patients infected with H. pylori, long term acid suppression → atrophic gastritis and intestinal metaplasia which ↑the risk of adenocarcinoma (again there is no evidence that this has occurred in human). 4. Enteric infection: ↑the risk of salmonella and shigella enteric infection and increased risk of cl.difficile infection ,there is also increased tendency of respiratory infections (increased risk of CAP and nosocomial infections). 2. Neutralization of the Acidity by Antacids: Antacids are basic substances that ↓the acidity by neutralization of HCl (antacids react with HCL to form salt and water) . the most commonly used bases include: trisilicate, hydroxide,carbonate and bicarbonate ions. They protect gastric mucosa from pepsin which is inactive above PH of 5. The therapeutic efficacy and the S/E depend also on the metal with which the base is combined( Al, Mg, Na). The therapeutic efficacy also depends on the rate of dissolution, water solubility, rate of reaction with the acid and rate of gastric emptying. Aluminum hydroxide also ↓H. pylori colonization and stimulate endogenous PGE production (some cytoprotective properties). Continuous elevation of PH is limited by the rate of gastric emptying. Ca+-containing antacids are not used anymore because it neutralizes the acidity, but then causes hypersecretion of acid. Bismuth containing antacids are also no more used. Uses of Antacids: 1. Mainly used to in non-ulcer and to relieve ulcer symptoms especially in the 1st few days in the course of treatment with H2-receptor blocker. 2. Large amount of antacids are shown to accelerate healing of peptic ulcer, but patient compliance is poor. 8 Individual Antacids: (no single one is satisfactory and mixtures are often used) A. Magnesium Oxide and Hydroxide: React quickly but cause diarrhea, Mg trisilicate reacts slowly to form MgCl2 which reacts with intestinal secretion to form the carbonate, the chloride being released and reabsorbed. Systemic acid-base balance is thus not significantly altered. B. Aluminum Hydroxide: Reacts with HCl to form AlCl3 which reacts with intestinal secretion to form insoluble salts especially phosphate. The chloride being released and reabsorbed, thus acid-base balance is not affected. It may cause constipation, hypophosphatemia, and it creates a risk of encephalopathy in patients with chronic renal failure. Usually Magnesium antacids are combined with aluminum hydroxide to neutralize the effect on the bowel. C. NaHCO3: Reacts quickly with acids to produce Co2 and NaCl, Co2 causes bletching. NaHCO3 is absorbed causing alkalosis. Na+ absorption may exacerbate edema in patients with heart failure or renal disease. D. Ca+ and Bismuth-Containing Antacids: They should be avoided. Those containing Ca+ may cause: rebound acid hypersecretion, hypercalcemia, and alkalosis. Bismuth may be absorbed and cause encephalopathy and arthropathy. E. Alginic Acid (Graviscon): Combined with antacid to encourage the adherence of the mixture to the mucosa, e.g.: for reflux esophagitis. F. Dimethicone: Added to antacids to reduce flatulence (anti-foaming agent), it is a silicone polymer that ↓the surface tension. Antacids may interfere with absorption of certain drugs as iron supplement, digoxin, tetracycline, and antifungal agents, so the patient either stop using these drugs or take it at least 2 hrs. after the antacids. 9 3. Enhancement of Mucosal Resistance: A. Eradication of H. pylori by Antimicrobials: 70-90% of patients with peptic ulcer have antral gastritis.Experimental infection of healthy volunteers with H. pylori produces gastritis. Its eradication protects against relapse of peptic ulcer. It ↑the placebo healing rates and of anti-secretory drugs. Eradication of H.pylori results in long term remission of the ulcer. Regimens of Eradication: 1. Antimicrobial therapy (1-2 weeks) compromising 2 ABCs (antibiotics): metronidazole with amoxicillin or clarithromycin or both (clarithromycin and amoxicillin) + suppression of acid secretion (omeprazole). (this is the most efficacious) Note: the preferred 2 ABCs combination is clarithromycin and amoxicillin. 2. Bismuth based therapies: these are more complicated and less well tolerated. B. Protection of the Base of Peptic Ulcer: (site protection) I. Colloidal Bismuth: Tripotassium dicitratobismuthate (de-nol), bismuth subsalicylate, and bismuth dinitrate is also available. Mechanism of Action: 1. Selectively chelates with protein material in the ulcer base forming a coating that protects it from adverse influence of acid, pepsin and bile. 2. It may also stimulate PGs, mucus, and HCO3 secretion. 3. Bismuth has anti H. pylori action. Conventional Bismuth triple therapy originally consisted of: Bismuth + metronidazole and tetracycline. 10 Uses of Colloidal Bismuth: 1. For benign gastric and duodenal ulcer. 2. It is also used for acute diarrhea and prevention of traveler’s diarrhea due to PG inhibition by salicylate also due to inhibition of chloride secretion.Bismuth also binds enterotoxins accounting for its benefit in treating and preventing traveler’s diarrhoea. Adverse Effects: Darkening of the tongue, teeth and stool for liquid formulation. Systemically may cause encephalopathy and arthropathy. II. Sucralfate: It's a salt of sucrose complexed to sulphated Al(OH)3 (basic Al. salt of sucrose octasulphate or octaphosphate). Mechanism of Action: In acidic environment of stomach the Al. moiety is released and the compound (-ve charged sucrose octasulphate) binds electrostatically to the (+ve charged protein molecule) that transudate form damaged mucosa. The result is a viscous paste that adheres to the ulcer base. It also inactivates pepsin and bile acids. and also enhances mucosal repair (angiogenesis and granulation tissue formation) by binding epithelial growth factor and fibroblast growth factor. Also it enhances endogenous production of PGs and thus enhances the mucosal defense and prevents recurrence. Uses of Sucralfate: For Benign gastric ulcer and chronic duodenal ulcer, it also prevents bleeding from stress-related gastritis. Efficacy is less than that of H2-receptor blockers Maintenance treatment is effective for preventing relapse. Side Effects: only constipation. 11 Drug Interactions: As it acts in acidic medium only, it should not be given with antacids.Sucralafate like antacids may bind to other medications impairing their absorption. C. Cytoprotection: PGs and their Analogues: Mechanism of Action: 1. It stimulates secretion of mucus and HCO3. 2. It maintains mucosal blood flow. 3. It prevents luminal H+ back diffusion to mucosa. 4. It enhances the rate of cell replication in the mucosa to hasten the repair of damaged epithelium. The mentioned effects are considered as (cytoprotective effects). PGE2 and I2 are potent inhibitors of gastric acid secretion.PGE2 and PGE1 and F2α enhance the protective mechanisms in the stomach and intestine. Misoprostol: Is a synthetic analogue of PGE1, that enhances mucosal resistance (cytoprotection). Also Misoprostol has acid inhibitory action at higher doses.Misoprostol inhibits acid secretion by reducing histamine stimulated cAMP production. Uses: 1. Used for the treatment of chronic gastric and duodenal ulcer due to its inhibition of acid secretion (independent of cytoprotective action). 2. Also it is used for prevention of NSAIDs-induced ulcer (considered the drug of choice for this purpose, PPIs may be as effective and better tolerated). Side Effects: Include diarrhea and abdominal pain. Contraindications: It is contraindicated in pregnant women because it may cause abortion. 12 How can you treat a patient with peptic ulcer? we can treat him by using one of the following: 1. The best treatment is by using proton pump triple therapy which consists of: a. PPI as omeprazole = one drug (antisecretory). b. Two of the following = 2 ABCs: amoxicillin, metronidazole, calrithromycin. The preferred: calrith. + amox. 2. We can use H2-receptor antagonist triple therapy but the first is better. 3. Also there is quadriple therapy used when PPI triple therapy is not successful and it consists of: 2 antibiotics + 2 adjunctive: bismuth + PPI Antibiotics are used for 1-2weeks with the PPIs and then you continue with the PPI treatment for 4-6 weeks. 13