May 2015 Large Animal Benchmark
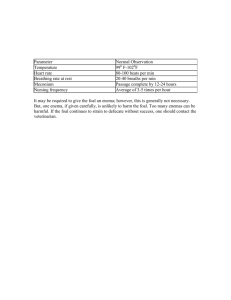
advertisement
Case 1 A 5-hour-old Quarter Horse filly (45 kg) presents to your clinic. The owners report that they assisted delivery when they noticed the mare was not progressing as they thought she should. Extraction was “difficult” and the foal appeared to decline rapidly after birth. They fed the filly milk from the mare with a syringe, administered an enema and 2 cc procaine penicillin IM. The breeding date was unknown, and the owners report no vaginal discharge or other complications during pregnancy. On arrival, mentation was dull, and cranial nerve exam was normal, save for a lack of menace. The foal has an unusually domed head, but no obvious synovial effusion in any of the joints, and no abnormalities noted on ultrasound of the umbilicus. Comet tails were noted diffusely on bilateral transthoracic ultrasonography. Provide an explanation for the lack of menace in this foal. List your top 3 differentials for this foal’s presenting neurologic signs. Bloodwork showed a slightly increased percentage of segmented neutrophils. The IgG was between 400 and 800 mg/dl. (Reference range >800 mg/dl). The concentration of sodium and chloride in the blood was increased (158 mmol/L, reference range 126-137 mmol/L, 117 reference range 95-105, mmol/L). You assess the foal as euhydrated and well-perfused, with a rectal temperature of 100.9F. PCV and total solids are 32% and 4.6 g/dL. Venous electrolytes are within normal limits. The foal’s end tidal and arterial CO2 are 48 mm Hg and 55 mm Hg, respectively. You also recognize that ventilatory drive appears adequate. You recognize ineffectual chest excursions and provide intranasal oxygen via a nasal cannula. Arterial blood gas re-evaluation (the patient is still spontaneously breathing with flow by oxygen) reveals the following: pH: PaO2: PaCO2: HCO3-: BE: 7.11 95 mmHg 80.0 mmHg 23.5 mmHg -2.4 mmol/L What is the most likely cause of the severe and progressive respiratory acidosis in this foal? Due to the progressive respiratory acidosis, perceived poor thoracic wall excursions, and concern for impending ventilatory failure, the decision is made to place the foal on the mechanical ventilator. You choose the mode of ventilation depicted below for this patient. Identify and characterize this mode of ventilation. Provide 2 GENERAL advantages and 2 disadvantages associated with its selection of the mode of ventilation. You anticipate that long-term ventilator support might be indicated for this foal. List and briefly discuss 5 potential complications associated with prolonged anesthesia and immobility in human and/or veterinary patients and your interventions to minimize the occurrence of each. On day 2, a spontaneous breathing trial (SBT) reveals improved respiratory muscle strength. Mechanical ventilation is re-implemented with the incorporation of pressure support (PS). Describe this mode of ventilation in terms of trigger, limit and cycle. List one advantage and one disadvantage associated with PS ventilation. What is PEEP and when would you apply it? The foal recovers and is successfully weaned from the ventilator. Unfortunately, at 8 days of age, the mare kicks the foal, causing a simple, closed, mid-diaphyseal femur fracture. The surgeons decide to internally plate the fracture, and the foal is prepared for surgery. What is the recommended induction agent for foals and what evidence is there for, or against, this practice? Isoflurane anesthesia is used, and the surgery is completed without complications in 4 hours. During recovery, the foal becomes tachycardic, hypercapneic, begins sweating profusely, develops muscle spasms and a fever of 108F. What is the cause of hyperthermia in this foal? What electrolyte abnormalities and alternations in serum chemistry values do you expect with this genetic disease? Describe the pathophysiology of both fever and hyperthermia. How are they similar and what are their differences? How does the cause of each reflect on the choice of treatment? Is this foal experiencing hyperthermia or fever? How do you treat this condition in this foal? Case 2 A 17 year old Draft-cross nursemare presents to you with an acute history of severe colic. She has just foaled 10 days ago and the manager of the farm found her during the evening barn rounds in severe distress. He is only 15 minutes from your hospital, and brings her and her orphan foal in immediately. On physical exam, you note a heart rate of 90 bpm, decreased pulse quality, and slow jugular filling. Mucous membranes are congested, with a delayed CRT. Her extremities are cold to the touch. You note a sporadic arrhythmia, with a heart rate of 80, and her lungs auscult normally. The abdomen is severely distended, and you suspect a large colon volvulus. A jugular catheter is placed, and 2 liters of hypertonic saline is administered, followed by a bolus of 20 ml/kg of Normosol R. A rectal exam confirms a distended, gas filled viscous. The mare is unresponsive to analgesia, and the manager agrees to go to surgery. Additional routine diagnostics include a PCV (62%) and TP (6.1 g/dl), as well as a venous and peritoneal L-lactate of 4.5 mmol/L and 9.3 mmol/L respectively. Serum calcium was 9.4 mg/dl (range of 11-13 mg/dl). An ECG noted the following abnormalities: Name the arrhythmia. You also notice the mare is salivating profusely and has a synchronous diaphragmatic flutter. What are differentials for hypocalcemia and arrhythmias for this mare, and how will you presumptively treat her. Before induction you decide to trocharize the mare to reduce abdominal pressure. Describe this procedure in detail, the different techniques, and possible complications. Is the mare’s lactate on presentation of clinical significance? Complete the following table relating to the American Society of Anesthesiologists classification of physical status. Category I II III IV V Physical Status Example of Category What ASA category is this horse? Following adequate resuscitation you anesthetize the patient, starting first with administration of a premedication. List the benefits of premedication in relation to anesthesia. What drug/drugs would you use in this patient for premedication, including dose? Justify your answer. For each of the following agents that can be used as part of an induction protocol describe their mechanism of action, dose and effects of the cardiovascular system. Propofol Alphaxalone Ketamine Midazolam Describe what drug or drug combination you would use to induce this patient to minimize cardiovascular dysfunction associated with many anesthetic agents. Upon induction, the patient in intubated with a cuffed ET tube and placed on isoflurane inhalation anesthesia. She is instrumented with an ECG, SpO2, ETCO2, IBP and temperature probe. There are many properties of inhalant anesthetics to consider in a critical patient. Define partition coefficient (PC) with regards to inhalant anesthetics. Would you like a low or high blood:gas partial coefficient (PC) in this patient and explain why? Given your response, which inhalant anesthetic agent available in North America is most appropriate in this case? What is the oil:gas PC and for which patients would you need to consider this possible complication of inhalant anesthetics? Define MAC (minimum alveolar concentration). Identify the MAC % for the anesthetic agent. Which agent is most potent? Agent Methoxyflurane Halothane Isoflurane Sevoflurane Desflurane Nitrous oxide MAC % Under anesthesia, you start the mare on a CRI of lidocaine in an effort to reduce the MIC. Your mentor is upset that the mare was not given a bolus prior to starting the CRI. Can you justify your actions? What general cellular mechanism/s is lidocaine postulated to have beneficial effects for horses with gastrointestinal disease? After surgery, the surgeon informs you that the horse required a colon resection, and was hypotensive several times while in the operating room. Exclusive of plasma lactate, list 3 negative prognostic factors related to large colon resection and anastomosis. After removing the tube in recovery, the mare begins to have difficulty breathing, with significant stridor, a stertorous noise on inhalation, and an abdominal component to her respiratory pattern. You attempt to replace the nasotracheal tube, both nasally, and orally, without success. You elect to perform an emergency tracheostomy. Describe this procedure, in detail. What could be possible causes of respiratory obstruction in this mare during recovery? Discuss pathogenesis of each, prevention and treatment. Case 3 You are presented with a 2 year old Tennessee walking horse colt that was castrated earlier in the day by a referring veterinarian. The owners had called the veterinarian back to the farm, due to uncontrolled hemorrhage from the incision sites. The RDVM attempted to locate the source, but was unsuccessful, and refers the horse to you. They arrive after a 90 minute trailer ride. On physical examination, the colt is shocky and pale, with a CRT of 4 seconds, and a heart rate of 80 bpm. There are numerous clamps in the inguinal region, and a steady stream of blood continues to pour from the incision sites. You place a catheter and administer a shock dose of 20 ml/kg of crystalloid fluids, while you wait for blood to be drawn from your donor. What parameters will you use to determine if a transfusion is needed? Describe the ideal donor for equine patients, the amount of blood you can take from the donor, considerations for donor health and the procedure in detail. During the transfusion, you attempt to staunch the bleeding with both physical and chemical means. Describe three different methods to directly address the hemorrhage and convert it to a controlled bleed. Regarding medications that are reported to reduce active bleeding, state mechanism/s of action, any evidence of a positive effect and the dose. Aminocaproic acid Formalin Vasopressin Yunan Bayao Conjugated estrogens Despite both local and systemic treatment, the horse continues to bleed unchecked. You decide to anesthetize the colt and either locate the vessel or re-emasculate the cord if needed. Define Total Intravenous Anesthesia (TIVA) and in basic terms describe the principle/s upon which this practice is based. List drugs that are recommended for use in equine TIVA (include in your response both initial IV loading dose, drugs for muscle relaxation and the combination you would use for CRI dose). Name three indications for the preferential use of TIVA over inhalant anesthesia Name three disadvantages of TIVA over inhalant anesthesia Under anesthesia, the horse’s mean arterial pressures are monitored continuously. Name two different ways to monitor blood pressure and the MAP recommended to maintain tissue perfusion. How can you provide pressure support to your patient? You are able to localize the hemorrhage to the spermatic artery. The cord was re-emasculated and double ligated. Once anesthesia has been discontinued, you notice the colt is having difficulty rising. What are four methods of assisted recovery you could use to help this colt to his feet? Name three reasons a horse may not be able to stand after surgery. The colt continues to flail, unable to stand, but attains a dog-sitting position. Palpation notes no firm muscle bellies, all are warm to the touch. Initially, the anal reflex is intact, tail tone is present, and deep pain is present in both hind limbs. The horse is able to voluntarily move the hindlimbs and no crepitus or swelling is noted. However, the colt continues to deteriorate, with loss of deep pain perception accompanied by paralysis in both hind limbs, and is euthanized the following day. Describe the neuropathological abnormality you suspect and describe some possible treatments that could have been attempted.