Word DOCX
advertisement

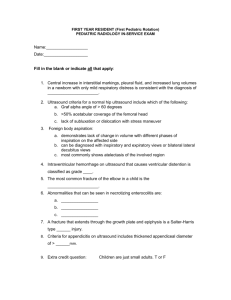
EMS Training Institute Office: (219) 947-6874 or (219) 947-6347 Fax: (219)947-6119 1500 South Lake Park Avenue, Hobart, IN 46342 E- Continuing Education May 2013- Pediatrics Due June 18, 2013 BLS portion: 2 hours ALS portion: 4 hours Complete packet: 6 hours See Robert Boby, Jessica Lawley, Jeffrey Lawley, or Robert Scott for CEU signatures Basic Life Support Research and Review (Brady’s Emergency Care 12th edition) 1. Complete the following regarding normal vital sign ranges in pediatrics: Age range Heart Rate Respiratory Rate Systolic Pressure Diastolic Pressure Newborn Infant 0-5 months Infant 6-12 months Toddler 1-3 years Preschooler 3-5 years School age 6-10 years Adolescent 11-14 years 2. Newly born or newborn refers to what age range: 3. Neonate refers to which age range? 4. Infant refers to which age range? 5. What is the average blood volume for the following: Age range Newborn 60 pound child 125 pound adolescent Blood volume 6. Complete the following regarding anatomical differences in pediatrics: Anatomic/physiology difference Potential impact on assessment/care Proportionally larger tongue Smaller airway structures Flat nose and face Head relatively heavier; underdeveloped neck Fontanelles/open sutures Thinner, softer brain tissue Nose/abdominal breathers Larger body surface area vs body mass Softer bones Flexible ribs Less protected abdominal organs Shorter, more narrow and flexible trachea 7. Complete the arms of the PAT and explain what you are observing for regarding each “arm” Observing for: Observing for: Observing for: 8. When may bulging fontanelles be a normal finding? 9. Abnormally bulging fontanelles indicates what? 10. Sunken or depressed fontanelles indicate what? 11. Anterior fontanel closes at ______ months and the posterior closes at ______ months. 12. How may you need to modify your interventions on a 3 year old pediatric trauma patient? 13. What is the proper positive pressure ventilation rate for a child infant to puberty? 14. What is the proper positive pressure ventilation rate for a child that has reached puberty? 15. Hypothermia can lead to what condition with newborns and infants? 16. Circle the appropriate terms: Croup is a (viral/bacterial) illness that often has a (rapid/gradual) onset with a (low/high) fever. Epiglottitis is a (viral/bacterial) illness that often has a (rapid/gradual) onset with a (low/high) fever Advanced Life Support Research and Review 1. The following diagrams represent congenital cardiac abnormalities. Label the type of anomaly. http://www.mayoclinic.com/health/congenital-heart-defects/CC00026 _________________ ___________________ _______________ ________________ ________________ ________________ ________________ ________________ ________________ ________________ ________________ ________________ Brady’s Paramedic Care, fourth edition 2. Complete the following regarding targeted/predicted SpO2 levels after birth: Minutes after birth Predicted SpO2 level Minutes after birth 1 4 2 5 3 10 a. Intubation of a full term newborn should require what size ET tube? b. 34-38 weeks gestation? C. 28-34 weeks gestation? Predicted SpO2 level 3. What are the common five fears of children, as it relates to illness or injury? a. b. c. d. e. 4. Newborns lose _____% of their birth weight within the first days of life, but should return to their birth weight by ____________________ (time frame). 5. Fever in a neonate indicates: 6. Infants should double their birth weight by _______ months. 7. Explain cephalocaudal progression, as it relates to development of muscle control: 8. List common illnesses/injuries to the patient age 6-12 months: a. b. c. d. e. f. g. h. i. j. 9. List the five most common injuries sustained in children ages 1-15 a. b. c. d. e. 10. Explain the following terms, and their indications, as it relates to pediatric respiratory issues: Head bobbing: Grunting: Stridor: Wheezing: 11. List six conditions that place a pediatric patient at risk for cardiopulmonary arrest: a. b. c. d. e. f. 12. Complete the pediatric GCS Eye Opening > 1 year < 1 year >1 year <1year 4 3 2 1 Best Motor Response 6 5 4 3 2 1 Best Verbal Response 5 4 3 2 1 >5years 2-5 years 0-23 months 13. Motor or sensory response for the pediatric GCS, should be assessed by: 14. Regarding intubation, why are straight blades often preferred to use with young children? 15. Describe the pediatric vagal response compared to the adult vagal response: 16. Why should esophageal detector devices be used with caution in the pediatric population? 17. Complete: D O P E 18. Indications for nasogastric tube (national scope if not in local protocol) placement in children include: a. b. 19. What medications may be beneficial to the 6 year old patient complaining of dyspnea with audible wheezing and the following vitals/readings? Respiratory rate 32, blood pressure 76/42, skin pale. After one combivent, you see this: What do you do now? 20. You have a 3 year old with trouble breathing. Parents state child has had an upper respiratory infection and ear infection for the past three days. Tonight the patient is more ill than he has been. A harsh, brassy cough has developed, temp 101.2F, slight nasal flaring, and slight inspiratory stridor. Vitals 140, 70/52, 28 with SpO2 93%. a. What will you be treating for? b. List five differential diagnoses for the above scenario: c. What care (including medications and dosages) will you be providing? 21. Why has the occurrence of epiglottitis decreased in recent years? 22. A patient that has had croup for the past few days, and experiences a worsening of symptoms (higher fever, productive cough, progressing sore throat) is likely to have what condition? 23. Why is status asthmaticus a critical situation that is treated aggressively? 24. Bronchiolitis is commonly caused by what virus? A. It presents similar to what other respiratory condition? B. Treatment for the patient that has symptomatic bronchiolitis includes: 25. What are the three main types of distributive shock? 26. Children with V-tach with pulses as a result of structural heart disease will/will not respond to medications. Treatment for these cases is : 27. The most common pediatric arrhythmias are: 28. Bacterial meningitis most commonly results from (list 3 bacteria):