Childhood Obesity and the Metabolic Syndrome
advertisement
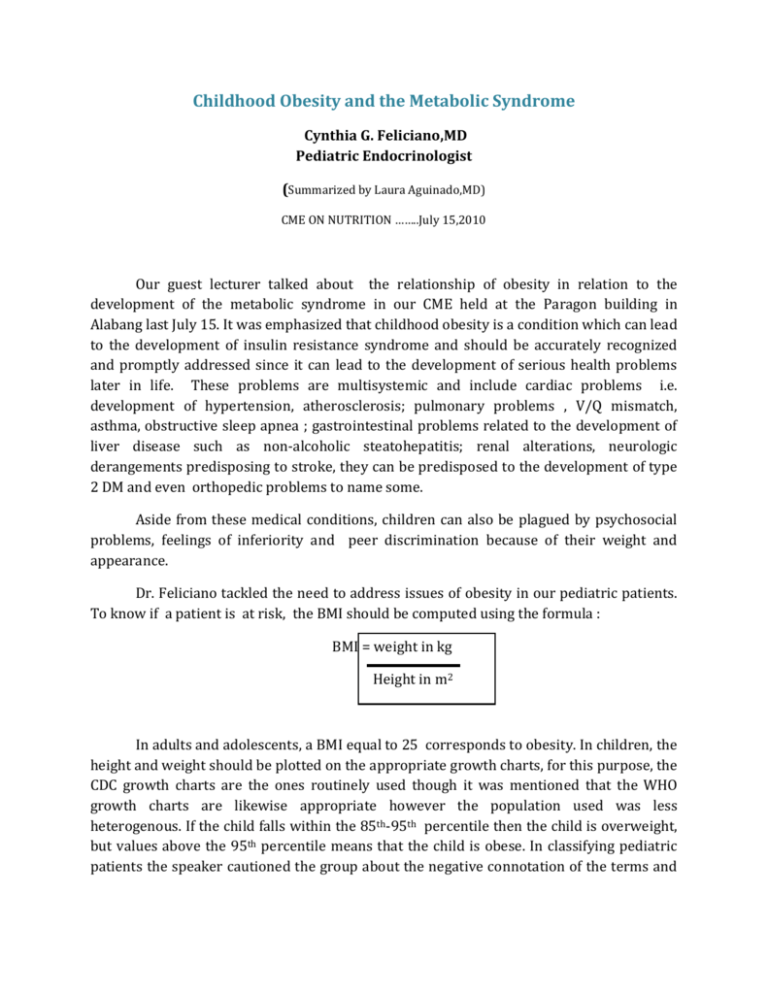
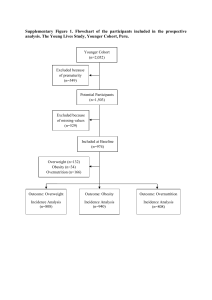
Childhood Obesity and the Metabolic Syndrome Cynthia G. Feliciano,MD Pediatric Endocrinologist (Summarized by Laura Aguinado,MD) CME ON NUTRITION ……..July 15,2010 Our guest lecturer talked about the relationship of obesity in relation to the development of the metabolic syndrome in our CME held at the Paragon building in Alabang last July 15. It was emphasized that childhood obesity is a condition which can lead to the development of insulin resistance syndrome and should be accurately recognized and promptly addressed since it can lead to the development of serious health problems later in life. These problems are multisystemic and include cardiac problems i.e. development of hypertension, atherosclerosis; pulmonary problems , V/Q mismatch, asthma, obstructive sleep apnea ; gastrointestinal problems related to the development of liver disease such as non-alcoholic steatohepatitis; renal alterations, neurologic derangements predisposing to stroke, they can be predisposed to the development of type 2 DM and even orthopedic problems to name some. Aside from these medical conditions, children can also be plagued by psychosocial problems, feelings of inferiority and peer discrimination because of their weight and appearance. Dr. Feliciano tackled the need to address issues of obesity in our pediatric patients. To know if a patient is at risk, the BMI should be computed using the formula : BMI = weight in kg Height in m2 In adults and adolescents, a BMI equal to 25 corresponds to obesity. In children, the height and weight should be plotted on the appropriate growth charts, for this purpose, the CDC growth charts are the ones routinely used though it was mentioned that the WHO growth charts are likewise appropriate however the population used was less heterogenous. If the child falls within the 85th-95th percentile then the child is overweight, but values above the 95th percentile means that the child is obese. In classifying pediatric patients the speaker cautioned the group about the negative connotation of the terms and advised that it would be better to label them as “at risk for overweight” and “overweight”, respectively. The body fat distribution is also correlated with the development of the metabolic syndrome with the android body type (apple shaped) or those whose fat is concentrated around the belly area being more predisposed than the bottom-heavy gynecoid body type (pear shaped). Once recognized, the parents should be advised on a treatment regimen under the supervision of a subspecialist especially if there are risk factors present or there is a positive family history . The treatment involves a step-wise approach starting with lifestyle based treatments which includes food management, exercise and behavior modification before going to the more intensive modalities such as administering weight loss medications and surgical procedures. Obesity is best prevented before associated disease conditions develop. Even though the problems which were discussed commonly manifests itself around the 4th decade of life, compelling evidence shows that the initiating events take root during childhood and may even start as early as the prenatal period hence good nutrition of the mothers was also emphasized. The success in the treatment and management of obesity, involves a concerted effort of the primary specialist, the pediatric endocrinologist , nutritionist and the childs parents or other primary caregiver to ensure that the goals of a healthier and more active lifestyle can be achieved. (This CME on Nutrition was PPS-STC’s 1st scientific meeting broadcasted live through USTREAM’s videostreaming)