16. OBESITY
advertisement
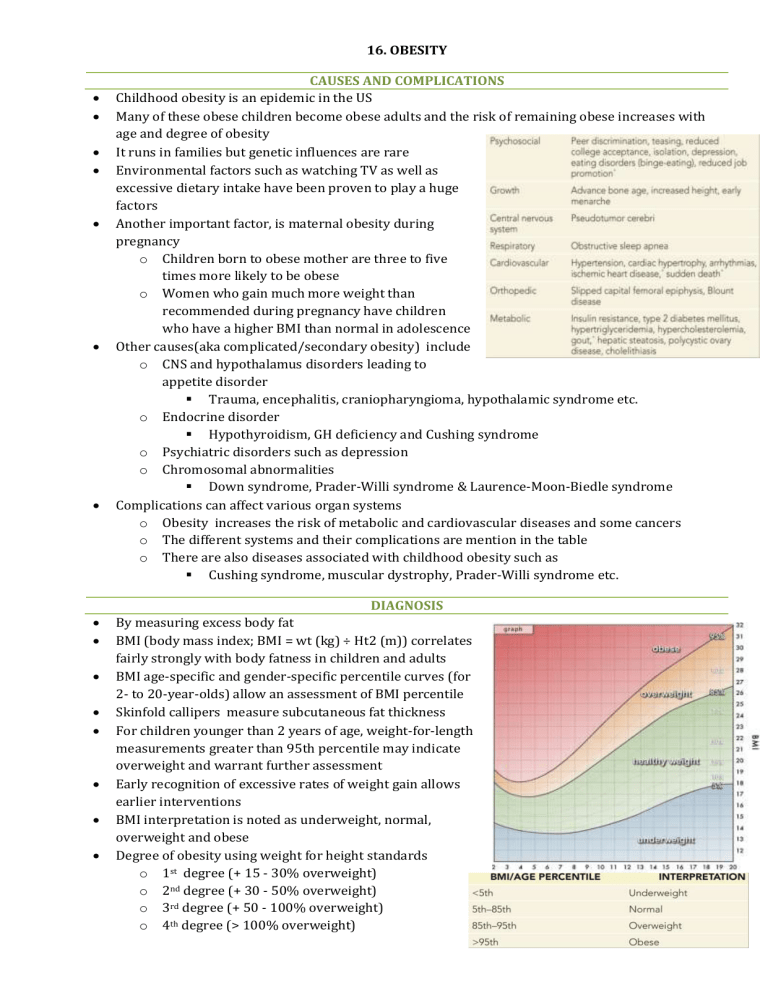
16. OBESITY CAUSES AND COMPLICATIONS Childhood obesity is an epidemic in the US Many of these obese children become obese adults and the risk of remaining obese increases with age and degree of obesity It runs in families but genetic influences are rare Environmental factors such as watching TV as well as excessive dietary intake have been proven to play a huge factors Another important factor, is maternal obesity during pregnancy o Children born to obese mother are three to five times more likely to be obese o Women who gain much more weight than recommended during pregnancy have children who have a higher BMI than normal in adolescence Other causes(aka complicated/secondary obesity) include o CNS and hypothalamus disorders leading to appetite disorder Trauma, encephalitis, craniopharyngioma, hypothalamic syndrome etc. o Endocrine disorder Hypothyroidism, GH deficiency and Cushing syndrome o Psychiatric disorders such as depression o Chromosomal abnormalities Down syndrome, Prader-Willi syndrome & Laurence-Moon-Biedle syndrome Complications can affect various organ systems o Obesity increases the risk of metabolic and cardiovascular diseases and some cancers o The different systems and their complications are mention in the table o There are also diseases associated with childhood obesity such as Cushing syndrome, muscular dystrophy, Prader-Willi syndrome etc. DIAGNOSIS By measuring excess body fat BMI (body mass index; BMI = wt (kg) ÷ Ht2 (m)) correlates fairly strongly with body fatness in children and adults BMI age-specific and gender-specific percentile curves (for 2- to 20-year-olds) allow an assessment of BMI percentile Skinfold callipers measure subcutaneous fat thickness For children younger than 2 years of age, weight-for-length measurements greater than 95th percentile may indicate overweight and warrant further assessment Early recognition of excessive rates of weight gain allows earlier interventions BMI interpretation is noted as underweight, normal, overweight and obese Degree of obesity using weight for height standards o 1st degree (+ 15 - 30% overweight) o 2nd degree (+ 30 - 50% overweight) o 3rd degree (+ 50 - 100% overweight) o 4th degree (> 100% overweight) Diagnostic steps 1. Anthropometric data including weight, heights and calculation of BMI and compared to gender and age appropriate charts 2. Dietary and physical activity history 3. Physical examination o BP, adiposity distribution (central or generalised), markers of comorbidities (acanthosis nigricans, hirsutism, hepatomegaly, orthopaedic abnormalities such as advanced bone age and flat foot ) o Physical stigmata of genetic syndromes 4. Lab studies o For obese children or children with comorbidities o Children between 9-11 should be screened for cholesterol o Other tests include haemoglobin A1c, fasting lipid profile, fasting glucose levels, liver function tests, and thyroid function tests PREVENTION AND TREATMENT Therapy depends on risk factors, including age, severity of overweight and obesity, and comorbidities, as well as family history and support Healthy eating and activity are the primary goal for all children with uncomplicated obesity and fast-rising weight for height In complicated obesity cases or if any comorbidities exist, specific treatment of the complication is necessary Obesity treatment programs can lead to sustained weight loss and decreases in BMI when the focus lies behavioural changes is family centred and simple straight-forward instructions are necessary like the ones suggested in the table Goals needs to be specific and realistic such as walking/biking to school two or three days a week or watching no v on school days rather than just saying “stop watching TV” or “do more sports“ o It needs to be comprehensive and it is necessary to discuss it with the family as they also need to make healthy life style changes including: Promotion of breast feeding Appropriate transition to complementary and table foods Important age-appropriate portion sizes for meals and snacks Use of smaller bowls and not eat directly form a bag or a box Little juice and no soda Less refined sugars found in sweets, chocolate, biscuits etc. and higher fibre content e.g. fruits, vegetables and cereals Food as reward should be avoided Physical activity should be emphasises especially organised sports as well as increase activities of daily living such as using stair, walking etc. TV in a child’s room should be avoided Treatment o More aggressive therapies are considered for those patients where the above mentioned have not worked o Treatment options may include Enrolment in a weight loss program In severe cases surgical treatment is considered