Type II and III Hypersensitivity Type I hypersensitivity Mediated by
advertisement
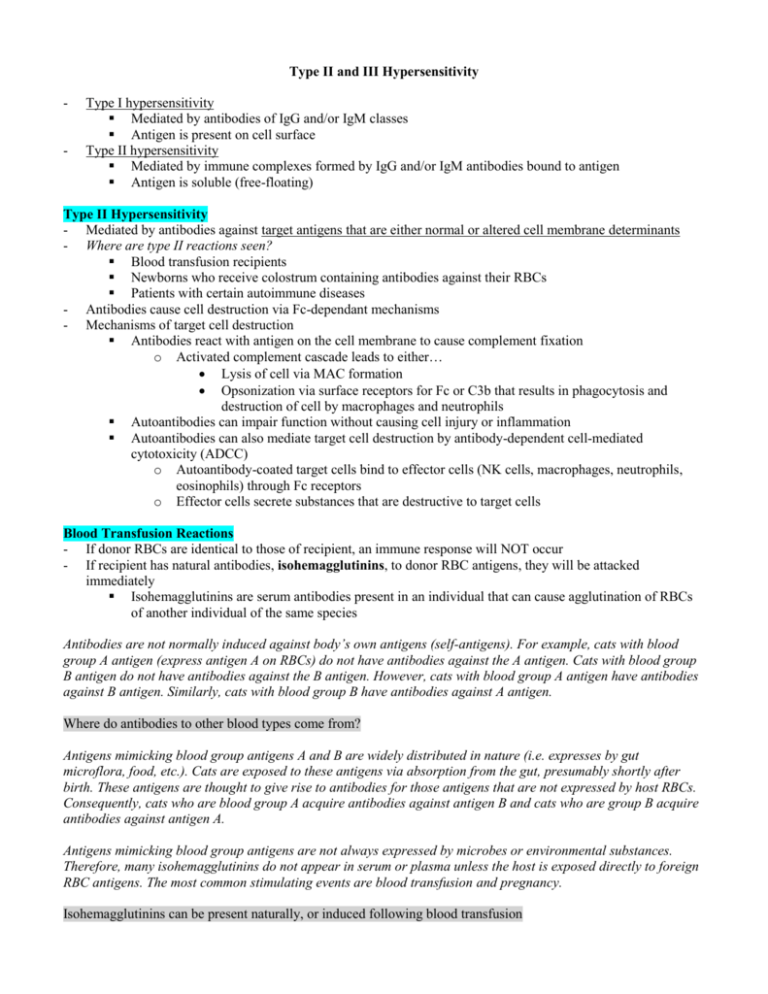
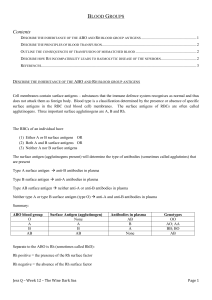
Type II and III Hypersensitivity - Type I hypersensitivity Mediated by antibodies of IgG and/or IgM classes Antigen is present on cell surface Type II hypersensitivity Mediated by immune complexes formed by IgG and/or IgM antibodies bound to antigen Antigen is soluble (free-floating) Type II Hypersensitivity - Mediated by antibodies against target antigens that are either normal or altered cell membrane determinants - Where are type II reactions seen? Blood transfusion recipients Newborns who receive colostrum containing antibodies against their RBCs Patients with certain autoimmune diseases - Antibodies cause cell destruction via Fc-dependant mechanisms - Mechanisms of target cell destruction Antibodies react with antigen on the cell membrane to cause complement fixation o Activated complement cascade leads to either… Lysis of cell via MAC formation Opsonization via surface receptors for Fc or C3b that results in phagocytosis and destruction of cell by macrophages and neutrophils Autoantibodies can impair function without causing cell injury or inflammation Autoantibodies can also mediate target cell destruction by antibody-dependent cell-mediated cytotoxicity (ADCC) o Autoantibody-coated target cells bind to effector cells (NK cells, macrophages, neutrophils, eosinophils) through Fc receptors o Effector cells secrete substances that are destructive to target cells Blood Transfusion Reactions - If donor RBCs are identical to those of recipient, an immune response will NOT occur - If recipient has natural antibodies, isohemagglutinins, to donor RBC antigens, they will be attacked immediately Isohemagglutinins are serum antibodies present in an individual that can cause agglutination of RBCs of another individual of the same species Antibodies are not normally induced against body’s own antigens (self-antigens). For example, cats with blood group A antigen (express antigen A on RBCs) do not have antibodies against the A antigen. Cats with blood group B antigen do not have antibodies against the B antigen. However, cats with blood group A antigen have antibodies against B antigen. Similarly, cats with blood group B have antibodies against A antigen. Where do antibodies to other blood types come from? Antigens mimicking blood group antigens A and B are widely distributed in nature (i.e. expresses by gut microflora, food, etc.). Cats are exposed to these antigens via absorption from the gut, presumably shortly after birth. These antigens are thought to give rise to antibodies for those antigens that are not expressed by host RBCs. Consequently, cats who are blood group A acquire antibodies against antigen B and cats who are group B acquire antibodies against antigen A. Antigens mimicking blood group antigens are not always expressed by microbes or environmental substances. Therefore, many isohemagglutinins do not appear in serum or plasma unless the host is exposed directly to foreign RBC antigens. The most common stimulating events are blood transfusion and pregnancy. Isohemagglutinins can be present naturally, or induced following blood transfusion - - Blood group antigens are glycolipids and/or glycoproteins IgM class isohemagglutinins Very efficient at activating complement Mediate destruction of RBCs via complement-mediated lysis o Results in massive hemolysis, leading to the release of large amounts of free Hb Free Hb can be detected in plasma (hemoglobinemia) and urine (hemoglobinuria) within hours o Large amounts of lysed RBCs can trigger blood clotting and disseminated intravascular coagulation (DIC) o Kidney damage may occur from blockage by large quantities of RBC membranes and Hbmediated acute tubular necrosis o Complement activation results in anaphylatoxins release, mast cell degranulation, and the release of vasoactive amines (agents that provoke circulatory shock) IgM class isohemagglutinins Less effective than IgM at activation complement IgG antibody-coated cells are destroyed via two mechanisms o Complement-mediated lysis o Phagocytosis (mediated by receptors for Fc and C3b) - Crossmatching Process of determining the compatibility of a donor’s blood with that of a recipient’s blood before transfusion Reveals the presence or absence of isohemagglutinins Major crossmatch o Used when RBCs are to be transfused o Involves combination of recipient serum or plasma and donor RBCs After mixing, plasma is examined for red tinge If red tingue noted, donor RBCs have been lysed and blood is not compatible Minor crossmatch o Used when plasma is to be transfused o Involved combination of recipient RBCs and donor serum or plasma After mixing, plasma is examined for red tinge If red tingue noted, donor RBCs have been lysed and blood is not compatible If whole blood (plasma and RBCs) transfusion is to be given, both major and minor crossmatching should be performed (if incompatibility in either, blood should not be given) Blood Transfusion Reactions in Dogs - There are 8 major blood group antigens in dogs (dog erythrocyte antigens – DEAs) 1.1, 1.2, 3, 4, 5, 6, 7, 8 - Natural isohemagglutinins are only present against DEAs 3, 5, and 7 Dogs that are negative for these three blood groups antigens (do not express DEAs 3, 5, or 7 on RBCs) may have natural isohemagglutinins against all three When dogs receive blood from donor RBCs that express DEA 3, DEA 5, DEA 7, or all three, hemolysis of donor RBCs will occur o Hemolysis is a delayed type hemolysis that does not cause clinically significant transfusion reaction Why? The transfusion reaction results in the production of antibodies against donor DEAs, However, the progression of antibody production occurs at a steady pace, much like the steady pace of the incompatible RBC levels declining (lifespan of incompatible donor RBCs is <12 hours). By the time there are maximal levels of antibodies in the body, there aren't enough RBCs to illicit a strong blood transfusion reaction In the situation where a dog who does not express DEA 3, 5, or 7 and received a blood transfusion from donor RBCs that do express DEA 3, 5, or 7 – is it possible that recipient dog DOES NOT have isohemagglutinins for the donor blood group antigens (i.e. recipient possesses isohemagglutinins for DEA 3, but the donor expresses DEA 5)? - Blood groups of clinical significance in dogs are DEA 1.1 and 1.2 These blood group antigens are potent stimulators of antibody production Dogs are either positive for DEA 1.1, positive for DEA 1.2, or negative for both Dogs do not have natural isohemagglutinins against DEA 1.1 and 1.2 What does this mean for a first-time blood transfusion? If a DEA1.1- (negative) dog receives blood from a DEA 1.1+ (positive) dog, the DEA1.1- recipient will mount an antibody response against DEA1.1 antigens present on the donor’s RBCs. A measurable antibody response takes more than five days, and a strong response even longer. Thus, a clinical reaction is not seen following the first blood transfusion (for the same reasons the delayed type hemolysis is not clinically significant). What about subsequent blood transfusions? The DEA1.1- dog will have high levels of circulating antibodies against DEA1.1 antigen within 2-4 weeks of the first transfusion. Therefore, a subsequent blood transfusion from a DEA1.1+ donor several months (or even years) later will cause an acute hemolytic transfusion reaction within minutes to hours. Thus, acute hemolytic transfusion reactions only occur in dogs negative for DEA1.1, DEA1.2, or both when they are sensitized against DEA1.1 or DEA1.2 (i.e. via the first blood transfusion). Therefore, crossmatching in dogs does not need to be done at the first blood transfusion (but probably should to avoid complications). However, crossmatching in dogs does need to be performed at second transfusion. Blood Transfusion Reaction in Cats - Cats have one blood group system – the AB system Three blood types – A, B, AB - Blood group antigens are inherited as a simple autosomal trait A antigen allele is dominant over B (overwhelming majority of cats express blood group A antigen) Inheritance of AB allele is unknown - Percentage of cats that are A or B positive is breed-dependent - AB positive cats are quite rare (5% in USA) Cat Breeds and Blood Groups Type B Frequency None 1-10% 11-20% 20-45% Type AB - Cat Breeds Burmese, Tonkinese, Russian Blue, Siamese and related breeds Maine Coone, Norwegian Forest, DSH, DLH Abyssinian, Birman, Himalayan, Persian, Somali, Sphinx, Scottish Fold Cornish, Devon Rex, Exotic and British shorthair cats Bengal, DSH, Scottish Fold, Birman, British shorthair, Somali, Abyssinian Cats have naturally-occurring antibodies responsible for potentially life-threatening transfusion reactions In type B cats, anti-A antibodies (especially of IgM class) are strong agglutinins and hemolysins In type A cats, anti-B antibodies (of both IgM and IgG classes) are weaker agglutinins and hemolysins Type AB cats lack naturally-occurring antibodies Type AB cats are universal recipients and can safely receive blood from either type A or B cats Blood Group A B AB Natural Isohemagglutinin Anti-B Anti-A None Transfusion significance Slightly delayed hemolysis Acute hemolytic reaction None What happens in transfusion of type A blood into type B cats? Results in an acute hemolytic reaction – rapid destruction of the donated type A RBCs. Severe clinical signs include hypotension, defecation, vomiting, hemoglobinemia, neurologic depression, and even death. Due to the presence of naturally-occurring antibodies, cats must be crossmatched prior to first transfusion (especially in those breeds with a higher incidence of type B individuals) Transfusion Reactions in Equines - Over 30 blood groups in horses - 7 internationally-recognized blood groups A, C, D, K, P, Q, U - Aa and Qa are the most important blood groups for hemolytic reactions - Antibodies against Aa and Qa antigens are not present in horse blood naturally - Natural antibodies against blood group antigens do exist (especially for Ca antigens) Cause weak agglutination and hemolytic crossmatch reactions Newborn Hemolytic Disease - Female animals may become sensitized to foreign RBCs by leakage of fetal RBCs into their blood stream through the placenta during pregnancy - In sensitized females, the anti-RBC antibodies may become concentrated in colostrum Newborns receive anti-RBC antibodies via colostrum feeding Antibodies cause rapid destruction of newborn RBCs Immune disorder is called hemolytic disease of the newborn (HDN) or neonatal isoerythrolysis - - - Four conditions must be met for HDN to occur Newborn must inherit RBC antigen from its sire that is not present in the mother Mother must be sensitized to RBC antigen Mother’s response to antigen can be enhanced by transplacental hemorrhage in late gestation Young animal must ingest colostrum containing high levels of anti-RBC antigen Dog – HDN is reported in pups born to DEA1.1- female dogs mated to DEA1.1+ male dogs Cats – HDN is reported in A or AB kittens born from B queens mated to A or AB toms Equines Blood group Aa in the A system and Qa in the Q system are more important for HDN o Blood groups are more antigenic that other o Incidence of HDN in foals is 1% (relatively common) All horses lack RBC antigen to donkeys, so HDN will develop when exposed to fetal donkey RBCs Ways to prevent HDN at subsequent pregnancies Foal should not drink colostrum from its mother Foal should receive alternate source of colostrum Strip the mare's udder every 2 hours for 2 days Provide an alternate source of milk for the first 24-36 hours Drug-induced Reactions - Hypersensitivity reactions to drugs are uncommon in dogs and cats, and rare in other domestic animals - May result from any of the four types of hypersensitivity reactions - Drugs most commonly associated with hypersensitivity reactions Penicillins, trimethoprim, sulfonamides Bind to RBCs and platelets to induce drug-specific antibody formation o Antibodies cause destruction of drug-coated cells via complement pathway or phagocytosis o Examples of drug-induced reactions Thrombocytopenia Hemolytic anemia - Drug withdrawal cures condition Autoimmune Reactions - Ideopathic thrombocytopenia purpura (ITP) Antibodies against platelets lead to platelet destruction via complement or phagocytes Decrease in platelets leads to bleeding (purpura) Clinical signs reflect animal’s inability to repair minor damage to capillaries o Petechiae in skin, gingival, and other mucous membrane and conjunctiva Mortality rate in dogs up to 30% o Predominant cause of death is severe GI hemorrhage Immunosuppressive therapy usually treats the condition o Response to this therapy is typically rapid and complete Splenectomy is effective for relapsing ITP o Removing spleen reduces the destruction of platelets by splenic macrophages - Autoimmune hemolytic anemia (AIHA) Autoantibodies against RBC antigens provoke RBC destruction (results in anemia) Cause is unknown – perhaps due to alteration in RBC antigens induced by drugs or microbes Therapy – blood transfusion, immunosuppression, splenectomy - Myasthenia gravis Disease of skeletal muscle in dogs and cats Caused by autoantibodies against acetylcholine receptors (AChR) Autoantibodies bind to an AChR at the neuromuscular junction and affect the neuromuscular transmission of the nerve impulse via three mechanisms o Activation of complement cascade at the neuromuscular junction (major mechanism) o Accelerated degradation of AChR molecules crosslinked by anti-AChR antibodies o Blocking binding of Ach to AChR - - - Disease results in various manifestations of muscle weakness o Exercise intolerance, difficulty chewing, swallowing and breathing, death from respiratory failure Therapy – immunosuppression Male infertility Testicular trauma can cause release of sperm into the circulation Sperm antigens stimulate production of autoantibodies o B/c testes are immuno-priviledged and aren’t exposed to lymphocytes under normal conditions Autoantibodies agglutinate and immobilize sperm o Consequently, affected males may become infertile Pemphigus Autoantibodies directed against desmosomal proteins that function in cell-to-cell keratinocyte adhesion o Antibodies mediate release of proteases from keratinocytes o Proteases cause breakdown of intercellular bridges, resulting in loss of cohesion b/w and separation of keratinocytes (acantholysis) Loss of cellular adhesion leads to free-floating keratinocytes in bullae (vesicles or blisters) Bullae are fragile and rupture easily, leaving denuded areas that can become secondarily infected Bullous pemphigoid Autoantibodies directed against hemidesmosomal proteins that attach basal keratinocytes to the basemement membrane Though pathophysiology is similar to pemphigus, the bullae develops within the subepidermis and is less likely to rupture o Bullae may contain fibrins, eosinophils, or neutrophils Disease can result from type II and type III hypersensitivity reactions Immunofluorescence is essential for definitive diagnosis o Antibody deposits in type II hypersensitivity are ribbon-like o Immune complex deposits in type III hypersensitivity are lumpy-bumpy Generalized Type III Hypersensitivity - Soluble antigen-antibody complexes are produced during normal immune response Complexes facilitate the clearance of antigen by phagocytes - Complexes can cause disease if produced in excessive amounts and not cleared efficiently Pathology results more often from small immune complexes as large immune complexes are more efficiently cleared because they can bind complement and Fc receptors more avidly Immune complexes that are not cleared are deposited in blood vessel walls of tissues (i.e. kidneys, synovial membranes) and activate complement Complement products C3a, C4a, and C5a cause localized mast cell degranulation o Increase vascular permeability o Induces inflammation C3a and C5a are chemotactic factors that attract neutrophils to infected tissue sites o Neutrophils intend to bind to immune complexes by means of Fc and complement receptors o Because immune complexes are deposited on the basement membrane surface, phagocytosis is impeded o Unsuccessful attempts to ingest adhering immune complexes causes neutrophils to “frustratedly” release lytic enzymes on the basement membrane Induces cell injury Accumulation of aggregates on basement membrane causes formation of microscopic lumpy-bumpy deposits (viewed via immunofluorescence) - Prototype of systemic immune complex disease is serum sickness Historically observed in diphtheria patients treated with horse anti-diphtheria toxin serum Patients developed antibodies to horse serum proteins (i.e. albumin) that formed circulating immune complexes o Clinical signs include fever, generalized vasculitis (rashes), edema, erythema, arthritis, and glomerulonephritis - Systemic lupus erythematosus (SLE) Multi-organ disease of dogs and rarely cats and horses Autoantibodies are produced against nucleic acid (self-DNA), self-nucleoprotein antigens (antinuclear antibodies), and histones o Immune complexes are composed of self-DNA or self-nucleoprotein antigens and antibodies Immune complexes accumulate in tissues where filtration of plasma occurs due to high hydrostatic pressure o Kidney (glomerulonephritis), arteries (vasculitis), joints (arthritis) Accumulation of aggregates on basement membrane appears as lumpy-bumpy deposits Exposure to UV light intensifies the disease. - - - Deposition of immunecomplexes in glomeruli increases permeability and results in loss of plasma protein into urine (albuminuria or proteinuria) Cutaneous lesions may be localized or generalized o Erythema, depigmentation, alopecia, scaling, crusting, ulceration, stomatitis (inflammation of mouth mucous membrane), panniculitis (inflammation of subcutaneous adipose tissue) Diagnosis focuses on antinuclear antibodies (ANA test) Discoid lupus erythematosus Relatively common, mild variation of SLE No involvement of other organs Antinuclear titer is negative Lesions are limited to facial skin and oral mucosa (rarely) o Erythema, scaling, crusting, ulceration, erosion o Exacerbated by sunlight Feline leukemia Tumor antigens are shed into circulation, resulting in antibody and immune complex formation Immune complex deposition causes glomerulonephritis C3 deficiency In dogs, results in defective clearance of immune complexes from circulation Purpura hemorrhagica Horses recovering from Streptococcus equi infection occasionally develop acute purpura Deposition of immune complexes consisting of S. equi M protein antigen o Causes vasculitis and vascular wall necrosis, resulting in hemorrhage Rheumatoid arthritis IgM autoantibody (RF) specific for Fc portion of normal IgG forms immune complexes that are deposited in joints o Causes inflammation due to accumulation of neutrophils and release of lytic enzymes Localized Type III Hypersensitivity - Called the Arthus reaction Produced by injecting an antigen intradermally or subcutaneously into an individual that has high levels of circulating antibody specific for that antigen Circulating antibodies rapidly bind to injected antigen and form immune complexes Immune complexes are deposited in the walls of small blood vessels at the injection site Inability of neutrophils to ingest immune complexes causes release of lytic enzymes o Results in local cutaneous vasculitis with necrosis - Pneumonitis in cattle Localized type III hypersensitivity reaction may occur in lungs when sensitized animals inhale antigens o Cattle inhale of spores of thermophilic actinomycetes present in moldy hay o Induces high levels of specific IgG production IgG encounters spore within alveolar walls, resulting in neutrophil accumulation and inflammation (pneumonitis) - Chronic obstructive pulmonary disease (COPD) in horses Bronchiolitis associated with long term hay exposure o Horses respond to actinomycete exposure by developing respiratory distress Etiology is controversial as immune complexes containing actinomycetes are not generally observed o Hypothesis is that long-term activation of macrophages leads to excessive production of neutrophil chemotactic cytokines (neutrophils are responsible for causing lung damage)