Andrea K. Balcom - eCommons@Cornell
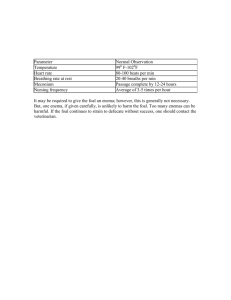
advertisement
1 Diagnosis and Treatment of Dysphagia in a Day Old Foal Andrea K. Balcom Dr. Kathleen Mullen Dr. Tom Divers Senior Seminar paper Cornell University College of Veterinary Medicine April 9, 2014 Key words: Aspiration Pneumonia, Dysphagia, White Muscle Disease, Hypothyroidism, Neonatal Maladjustment Syndrome, Pharyngeal Dysfunction 2 ABSTRACT A 24-hour-old Morgan Colt was presented to Cornell University’s Large Animal Medicine Service for evaluation and treatment of pneumonia. The foal was bright, alert, responsive, ambulatory and nursing well. Radiographs and a thoracic ultrasound showed cranial ventral consolidation of the lungs bilaterally. After nursing, an endoscopic examination revealed milk in the trachea, indicating that the foal was aspirating milk after he suckled. No oral or upper airway structural abnormalities were visualized. A nasogastric tube was placed, the foal was muzzled and he was started on a course of IV antibiotics to treat the aspiration pneumonia. Over the next two weeks, potential causes of the foal’s dysphagia were explored and different treatment options tried. This case report will explore etiologies of dysphagia in the neonatal foal such as white muscle disease, neonatal maladjustment syndrome, hypothyroidism, and pharyngeal dysfunction. It will also investigate the treatment options available and supportive care necessary to maintain these patients. INTRODUCTION Normal swallowing occurs in four phases, preparatory, oral, pharyngeal and esophageal. The preparatory and oral phases are under voluntary control, except in the neonate in which the sucking reflex is regulated at the level of the brainstem. Swallowing is a complex act that involves 26 muscles, 5 cranial nerves, and requires coordination between neural reflexes and a voluntary effort that matures with development. Abnormalities in neural or anatomic development can lead to swallowing dysfunction (Kakodkar, 2013). Dysphagia, or difficulty swallowing, is any defect in the ingestion or transport the endogenous secretions, food or water that may occur from the oral cavity to distal esophagus (Holcombe, Hurcombe, & Barr, 2012). 3 Dysphagia may be congenital, acquired, a main problem or part of a multi-systemic condition, and can be associated with muscular or neural disease. Problems specifically associated with the pharyngeal phase of swallowing can result in material coming from the nares and/or contaminating the lower airways. Because breathing and swallowing share the same pathways, a lack of coordination during swallowing can result in aspiration of liquid or solid material into the lungs. In adults, laryngeal contamination and irritation of the laryngeal mucous generally stimulates coughing which is designed to help protect the lower airway. In neonates, the cough response is not yet developed. Neonates may have a gag reflex present, but it may be weeks to months before they actually cough. The lack of a coughing response combined with dysphagia places the neonate at a much higher risk of pulmonary contamination that could likely result in aspiration pneumonia (Holcombe, Hurcombe, & Barr, 2012). SIGNALMENT 24 hour old Morgan Colt CHIEF COMPLAINT Increased bronchovesicular lung sounds with cranioventral crackles and wheezes on thoracic auscultation, and radiographic evidence of cranial ventral consolidation bilaterally, both highly suggestive of pneumonia. CASE HISTORY A 24 hour old Morgan Colt was seen by his veterinarian for his first routine wellness exam. The foal was born at approximately 350 days gestation to a multiparous mare. The birth was attended and was reportedly uneventful. The foal stood in an appropriate amount of time and nursed well. The placenta passed and other than one clean tear, appeared grossly normal with no 4 evidence of placentitis or early detachment. At the wellness exam with the veterinarian the following day, the foal appeared healthy, active, nursing with no visible difficulties, and had a normal temperature, heart rate and respiration rate. An IgG SNAP test was greater than 800 mg/dL, suggesting that the foal had received an adequate amount of colostrum from the mare. On thoracic auscultation, however, the veterinarian heard increased bronchovesicular sounds and cranioventral crackles and wheezes bilaterally. Radiographs were taken and revealed cranial ventral consolidation in the lungs bilaterally. An endoscopic examination showed no structural abnormalities in the oral cavity or upper airway. The foal was given 1.25 mg of Vitamin E and Selenium intramuscularly. Blood was drawn from the dam for Vitamin E & Selenium testing. The foal was then referred to Cornell for further diagnostics and treatment. PRESENTATION On presentation to Cornell later that afternoon, the foal was bright, alert, responsive, active and nursing well. Thoracic auscultation confirmed the referring veterinarian’s findings of increased bronchovesicular sounds bilaterally, crackles and wheezes cranial ventrally, as well as increased upper airway noise. The foal had a grossly normal umbilicus, a normal oral examination, and the remainder of the physical exam was unremarkable. A complete blood count (CBC) and ISTAT were run and revealed a mild lymphopenia (1.1 thou/ul) that was attributed to a stress response, and an elevated creatinine (4.6 mg/dL), which is not uncommon in newborn foals in the first 48 hours of life. A thoracic ultrasound showed mild to moderate pleuritis bilaterally in all lung fields, with the left lung worse than the right, and consolidation of the left cranial ventral lung lobes. An ultrasound of the umbilicus was normal. A Mila over-the-wire catheter was placed in the right jugular vein, a nasogastric tube was passed through the left nare and sutured in place, and the foal was muzzled so he could not nurse. Treatment for pneumonia 5 was initiated with intravenous potassium penicillin 1 million units every 6 hours and amikacin 900 mg every 24 hours, Plasmalyte 1liter boluses intravenously, and sucralfate 1 gram every 8 hours via the nasogastric tube. The foal was fed 15% of his body weight in mare’s milk over the course of 24 hours via the nasogastric tube. CLINICAL FINDINGS The following day, the foal’s muzzle and nasogastric tube were removed and he was allowed to nurse. While he suckled, his trachea was ausculted and no appreciable gurgles or noises were heard. An endoscopic examination was performed immediately after he nursed and milk was visualized in the trachea. No oral or upper airway abnormalities were seen. A Chemistry Panel was run and showed no significant abnormalities. A CBC revealed a neutropenia (1.4 thou/uL) with a left shift (0.9 thou/uL band neutrophils) and mild toxic changes, as well as an increased fibrinogen (400 mg/dL). These changes were attributed to an inflammatory response to pneumonia. Based on the foal’s clinical picture and the evidence of milk in the trachea after nursing, it was determined that the foal most likely had aspiration pneumonia due to dysphagia. DIFFERENTIAL DIAGNOSIS The list of differentials for dysphagia in the horse is extensive. The differentials that would be most likely in a neonatal foal include a cleft palate, prematurity or dysmaturity, a fourth branchial arch defect, cranial esophageal sphincter dysfunction, laryngeal abnormalities, pharyngeal dysfunction or paresis, neonatal maladjustment syndrome, white muscle disease, hypothyroidism, hypocalcemia, HYPP, EHV-1, botulism, meningitis, pharyngitis or laryngitis, or toxins such as polyacrylamide and potentially heavy metals. Based on the endoscopic examination, physical abnormalities including cleft palate, fourth branchial arch defects and 6 laryngeal abnormalities were ruled out. The history, physical exam, and bloodwork also did not support inflammatory or infectious causes such as EHV-1, Botulism, meningitis, or certain metabolic issues including HYPP and hypocalcemia. The differentials that seemed most likely for this foal were White Muscle Disease, Neonatal Maladjustment Syndrome, hypothyroidism and pharyngeal dysfunction or paresis. White Muscle Disease White Muscle Disease, also known as Nutritional Myodegeneration, is the result of a diet deficient in Selenium and/or Vitamin E. Selenium and Vitamin E function together to protect and stabilize cell membranes by decreasing the formation of and destroying peroxides that may disrupt cell metabolism and cause cell destruction. (Bernard & Barr, 2012). Foals that present with White Muscle Disease are typically from geographical areas where the soil is selenium deficient and the mare has not been receiving adequate vitamin and mineral supplementation. Clinical signs are usually seen at birth or during the first year of life and present as abnormalities in muscular function. These abnormalities may include recumbency, difficulty or inability to stand, stiff and stilted gait, difficulty nursing or masticating resulting in dysphagia, often with milk coming from the mouth or nares while nursing, and respiratory stridor secondary to pharyngeal paresis (Bernard & Barr, 2012). A diagnosis of White Muscle Disease is based on geographical location, physical examination findings suggestive of neuromuscular disease, decreased blood selenium and glutathione peroxidase activity, muscle inflammation, an increase in AST or CK levels, electrolyte imbalances such as hyperkalemia with moderate hyponatremia and hypochloremia, and response to treatment (Bernard & Barr, 2012). The treatment includes correcting the deficiency with Vitamin E and Selenium supplementation (potentially long term), correcting any electrolyte imbalances, anti-inflammatories to help with muscle pain, and 7 additional nursing care such as exercise restriction and entereal feeding if dysphagia is part of the clinical picture. Neonatal Maladjustment Syndrome A second differential for dysphagia in the neonate is Neonatal Maladjustment Syndrome, also known as Hypoxic Ischemic Encephalopathy or, more commonly, Dummy Foal Syndrome. This syndrome describes neonates that are exhibiting behavioral or neurological abnormalities that cannot be attributed to infectious or toxic conditions, congenital or developmental abnormalities, or metabolic disorders (Bernard & Barr, 2012). It is attributed to either intranatal or postnatal asphyxia causing a deficiency in oxygen reaching the foal’s brain, resulting in encephalopathy. This asphyxia may be due to placentitis, a long Stage II labor, cord compression, birth apnea, or cardio-pulmonary failure (Palmer, 2008). Signs may be present at birth or may manifest after several days, and can range from almost imperceptible behavior abnormalites to tonic clonic seizures. The signs often manifest as neurological behaviors that may include a loss of affinity for the mare, a change in the suckle response exhibited by a loss of tongue curl, loss of tongue coordination, and disorientation to the udder, a change in muscle tone, intermittent depression, stargazing, abnormal facial expressions such as spams, lip curling and chomping or grimacing, and a change in respiratory function (Palmer, 2008). There are no specific serology or hematology components to the syndrome, so the diagnosis is based on the foal’s signalment, history, and the exclusion of other neurologic diseases. The treatment is supportive care and varies based on the severity of the syndrome. It may include enteral feeding, anticonvulsants, antimicrobial therapy to prevent secondary infections, and intravenous fluid therapy. Prognosis is also based on the severity of clinical signs, but if seizures are controlled, good nursing care is provided, and secondary complications are avoided or treated, the prognosis 8 tends to be good and these foals often go on with no long-term effects on growth or development (Bernard & Barr, 2012). Hypothyroidism A third differential that can result in dysphagia in the neonate is hypothyroidism. Healthy foals are born with markedly elevated T3 and T4 levels that decrease to adult levels over the first few weeks of life (Breuhas, 2011). Hypothyroid foals, however, will have levels at half of that of their healthy counterparts. Thyroid hormones are important in the development and maturation of the nervous, respiratory and musculoskeletal systems during the pre- and post-natal period (Himler, Hurcombe, & Griffin, 2012). A decrease in these hormones can result in weakness, poor suckling ability and dysphagia, hypothermia, tendon contracture or rupture, delayed bone development and goiter. A decrease in T3 and T4 levels in the neonate can be correlated to prematurity, respiratory distress and asphyxia, the type of parturition (spontaneous, induced, difficult), critical illness, and septicemia (Panzani, Comin, & Galeati, 2012). Hypothyroidism can also be due to congenital goiter, which is often attributed to too much or too little iodine in the mare’s diet, or from her ingesting goitrogenic plants such as mustard, kelp, horseradish or cabbage (Breuhas, 2011). When treating hypothyroidism in the neonate, it is important to determine whether the foal is actually hypothyroid, or if the decreased hormone levels are due to nonthyroidal illness syndrome or secondary to certain drug administration such as glucocorticoids or NSAIDS. If the foal truly is hypothyroid, then treatment includes supportive care, correcting the mare’s diet if that is the cause, and thyroid supplementation with Levothyroxine at 20-50 ug/kg/d PO. (Breuhas, 2011). Pharyngeal Dysfunction 9 The fourth differential that was considered in this case was pharyngeal dysfunction and/or paresis. Pharyngeal dysfunction may be due to weakness, incoordination or a combination of motor and sensory underdevelopment. The dysfunction may originate in the central or peripheral nervous system (Holcombe, Hurcombe, & Barr, 2012). Unfortunately, while this is the most commonly diagnosed cause for dysphagia in the neonate, there is very little information about why it happens. It may be secondary to the differentials already discussed, or due to dysfunction at the level of the nervous system level which has not yet been studied. It occurs in both human and equine neonates. In humans, these infants generally improve with time and their swallowing becomes normal in 2-3 weeks (Holcombe, Hurcombe, & Barr, 2012). The outcome is similar in foals. Treatment involves supportive care that may include entereal feeding and antibiotics to treat aspiration pneumonia, and the foal is often able to nurse again after a week or two. Diagnosis In this foal, the dam’s Vitamin E and Selenium levels were measured just prior to his presentation and were normal, ruling out White Muscle Disease as a likely cause. The foal’s history and physical exam were not supportive of Neonatal Maladjustment Syndrome. Bloodwork at the time of the foal’s birth could have given some insight into if there was mild stress or hypoxia during foaling, but without this information, and considering how well the foal stood, nursed, and his activity level since birth, Neonatal Maladjustment Syndrome was ruled down as a likely cause. The foal’s thyroid levels were not measured at birth, but at 10 days of age his T4 level was 17.29 ug/dL and his T3 level was 2.03 ng/dL, both within the normal ranges for a foal of that age. While it is possible the thyroid hormones were decreased at birth, and had normalized by this time, the foal showed none of the other signs of weakness that can be 10 attributed to hypothyroidism. Based on this information and no evidence of other neurological abnormalities being present, the foal’s dysphagia was attributed to pharyngeal dysfunction. TREATMENT and OUTCOME During his two-week hospitalization, the foal was treated with a course of IV antibiotics and then switched to oral chloramphenicol to treat the aspiration pneumonia. He was also given oral water soluble Vitamin E, as well as sucralfate. Every two to three days during his hospitalization, the foal was allowed to nurse and an endoscopic examination was performed immediately after. Milk was visualized in the trachea at every examination. He was taught how to pan feed and endoscopic examination after pan feeding revealed that he was able to drink from the pan without aspirating, so the feeding tube was removed and he was put on a schedule of pan feeding every two hours during the day and every four hours at night. After the foal was successfully pan feeding, the only abnormality noted was that when he would drink, and also when he would attempt to eat hay, he was repeatedly observed with his tongue sticking out to the left side of his mouth. This never seemed to cause any complications with his prehension or swallowing, and no cause was ever determined, but it was a consistent behavior. Since the foal was still aspirating when nursing at the time of discharge, it was decided that the mare would be dried off so the foal could remain with her and that he would be pan fed milk replacer until he was successfully eating solid food. The foal was reportedly slower to grow initially and smaller than the other foals his age, but by 8 months of age he had caught up in size and since then has continued to do well. He has not shown any other signs of dysphagia since he was discharged from the hospital. DISCUSSION: 11 Dysphagia is a relatively common disorder equine practitioners encounter in horses of all ages. In the neonatal foal, dysphagia can present in various ways and with different levels of severity. In some cases there may be milk present in the nares after nursing with little to no aspiration, in other cases such as this foal, there was no milk present in the nares but the foal clearly aspirates when nursing. Many foals are able to nurse without aspirating after a few days of supportive care, while some foals are never able to nurse successfully. While there are many differentials for what causes the dysphagia, in most cases it is attributed to pharyngeal dysfunction and no physiological cause is ever determined. No matter what the cause, if the foal is given proper supportive care until they could successfully nurse or pan feed, as well as antimicrobials to treat aspiration pneumonia, then in most cases the foals are able to become healthy, grow, and have successful athletic careers (Holcombe, Hurcombe, & Barr, 2012). In human infants with dysphagia, certain treatments are used to help facilitate the development of oral motor skills and lessen the swallowing dysfunction (Kakodkar, 2013). Modifications such as pacing the feedings so they are short and frequent are used both to keep the infant from getting too much milk at once as well as to help strengthen the pharyngeal muscles. In this foal, the mare was milked prior to him nursing so she would not let down and overwhelm him with the volume of milk being produced. Unfortunately, even when she was milked out, he would still aspirate. Allowing him to nurse in short and frequent amounts was not attempted. While this approach may have helped, it would require a great deal of time and man power to make sure the foal was getting a sufficient amount of milk, as well as frequent endoscopy examinations to confirm that the foal was not aspirating after nursing. Changing the viscosity of the milk or texture of the food is another treatment option in infants. Thin liquid causes a lack of coordination among sucking, breathing and swallowing (Almeida & Alemeida, 12 2011). Increasing the viscosity of a liquid to a more honey-like consistency has been successful at improving swallowing and reducing aspiration in dysphagic humans. While changing the viscosity of mare’s milk from the udder could prove to be difficult to impossible, this concept could be helpful with neonates who are dysphagic when being bottle-fed or pan fed. A pacifier is often used in dysphagic human infants to help strengthen the pharyngeal muscles. Since foals can be stimulated to suck on fingers or inanimate objects, it may be possible to utilize a similar technique to help strengthen the foal’s pharyngeal muscles and suckling reflex. In human infants, positional adaptations, such as changing the angle at which the child is held when fed, is one of the first treatment changes that is often implemented (Kakodkar, 2013). For foals who continue to aspirate after an extended period of supportive care and enteral feedings, and whose dysphagia is not due to treatable causes such as White Muscle Disease or hypothyroidism, the most successful treatment seems to be teaching the foal to pan feed. When pan feeding, the foal is standing, his nose is pointed down and his head is lowered. While it is unclear how this change in position changes the mechanics of the foal’s ability to swallow, they are able to better protect their airway and drink successfully without aspirating. 13 WORKS CITED 1) Kakodkar, K. (2013). Pediatric Dysphagia. The Pediatric Clinics of North America, 60, 969977. 2) Holcombe, S., Hurcombe, S., & Barr, B. e. (2012). Dysphagia Associate with Presumed Pharyngeal Dysfunction in 16 Neonatal Foals. Equine Veterinary Journal, 44, 105-108. 3) Bernard, W., & Barr, B. S. (2012). Equine Pediatric Medicine. London: Manson. 4) Palmer, J. (2008). Neonatal Encephalopathy. 5th Havemeyer Septicemia Workshop. Salem. 5) Breuhas, B. A. (2011). Disorders of the Equine Thyroid Gland. Veterinary Clinics of North America: Equine Practice, 27, 115-128. 6) Himler, M., Hurcombe, S., & Griffin, A. e. (2012). Presumptive Nonthyroidal Illness Syndrome in Critically Ill Foals. Equine Veterinary Journal, 44 (41), 43-47. 7) Panzani, S., Comin, A., & Galeati, G. e. (2012). How Type of Parturition and Health Status Influence Hormonal and Metabolic Profiles in Newborn Foals. Theriogenology, 77, 1167-1177. 8) Almeida, M., & Alemeida, J. M. (2011). Adequacy of Human Milk Viscostiy to Respond to Infants with Dysphagia: Experimental Study. Journal of Applied Oral Science, 9, 554-559.