every day in may need to know
advertisement
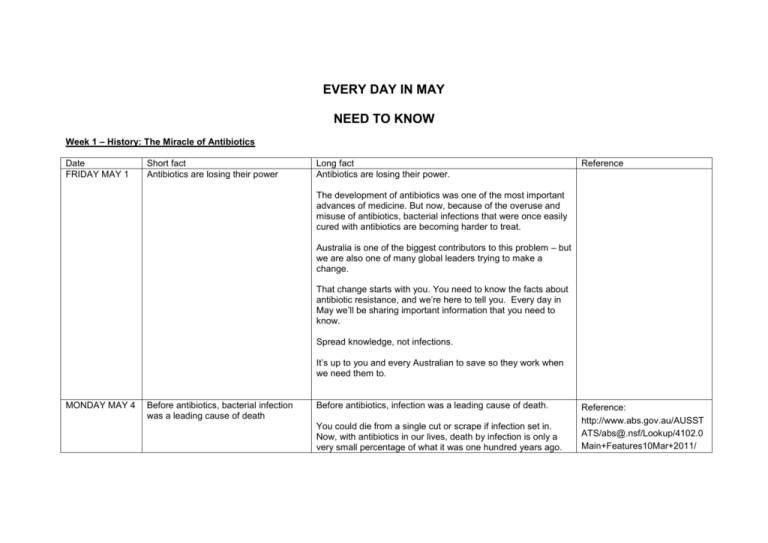
EVERY DAY IN MAY
NEED TO KNOW
Week 1 – History: The Miracle of Antibiotics
Date
FRIDAY MAY 1
Short fact
Antibiotics are losing their power
Long fact
Antibiotics are losing their power.
Reference
The development of antibiotics was one of the most important
advances of medicine. But now, because of the overuse and
misuse of antibiotics, bacterial infections that were once easily
cured with antibiotics are becoming harder to treat.
Australia is one of the biggest contributors to this problem – but
we are also one of many global leaders trying to make a
change.
That change starts with you. You need to know the facts about
antibiotic resistance, and we’re here to tell you. Every day in
May we’ll be sharing important information that you need to
know.
Spread knowledge, not infections.
It’s up to you and every Australian to save so they work when
we need them to.
MONDAY MAY 4
Before antibiotics, bacterial infection
was a leading cause of death
Before antibiotics, infection was a leading cause of death.
You could die from a single cut or scrape if infection set in.
Now, with antibiotics in our lives, death by infection is only a
very small percentage of what it was one hundred years ago.
Reference:
http://www.abs.gov.au/AUSST
ATS/abs@.nsf/Lookup/4102.0
Main+Features10Mar+2011/
TUESDAY MAY
5
The discovery of penicillin was so
important, it was awarded a Nobel
Prize
What would happen now if we lost the miracle of antibiotics?
General Record of Incidence
Mortality (GRIM) books
The ‘wonder drug’: the discovery of penicillin was so significant
it was awarded the Nobel Prize in Physiology or Medicine in
1945.
Ref: Nobel Prize website
http://www.google.com.au/url?
sa=t&rct=j&q=&esrc=s&frm=1
&source=web&cd=1&ved=0CB
4QFjAA&url=http%3A%2F%2F
www.nobelprize.org%2Fnobel
_prizes%2Fmedicine%2Flaure
ates%2F1945%2F&ei=ZP8tVd
rOoHXmAWBwID4Cw&usg=AF
QjCNGtxXAbEhlwhhDMo8nRj
Du_Fhuk5Q&sig2=YSlMHzrsu
11tqny_h5LVlQ&bvm=bv.9079
0515,d.dGY
In 1945, Alexander Fleming, Howard Florey and Ernst Chain
were awarded the Nobel Prize in Medicine for having
contributed to discovering penicillin. Now, 70 years later the
‘precious resource’ of antibiotics is losing its power because of
the common misuse of antibiotics.
WEDNESDAY
MAY 6
100 years ago there was no effective
cure for common bacterial infections
100 years ago, before the widespread use of antibiotics, there
was no effective cure for common bacterial infections.
Between 1922 and 1924, infectious and parasitic diseases
caused 15% of all deaths in Australia. By 1966, they caused
less than 1% of all deaths. This reduction is generally believed
to be the result of medical advances including the availability of
antibiotics from the 1940s.
What would happen now if we lost the miracle of antibiotics?
{1)Reference:
http://www.healthychildren.org/
English/healthissues/conditions/treatments/P
ages/The-History-ofAntibiotics.aspx
Source:
http://www.abs.gov.au/AUSST
ATS/abs@.nsf/Lookup/4102.0
Main+Features10Mar+2011#1
0
Australian Institute of Health
and Welfare, 2000, Australia's
Health 2000, AIHW cat. no. 19,
viewed 24 February 2011,
<www.aihw.gov.au>.
THURSDAY
MAY 7
Doctors used to be powerless against
serious bacterial infections
Before antibiotics, doctors used to be powerless against
serious bacterial infections.
The only option for severe bacterial infections was to hope that
a person’s own immune system would overpower the infection.
But, for millions each year this never happened.
(Reference:
Penicillin:Medicine's Wartime
Wonder Drug and Its
Production at Peoria, Illinois
John S. Mailer, Jr., and
Barbara Mason Historical
Research and Narrative)
What would happen now if we lost the miracle of antibiotics?
http://www.lib.niu.edu/2001/iht
810139.html
FRIDAY MAY 8
*WEEKEND
SUPER FACT*
Before antibiotics, simple bacterial
infections could kill
The world before antibiotics
Before the first antibiotics were prescribed in the 1940s,
bacteria was a killer.
A small cut could become fatal if it became infected, and
routine surgery and childbirth were fraught with the risk of
infection.
What would happen now if we lost the miracle of antibiotics?
amr-review.org
http://amrreview.org/sites/default/files/A
MR%20Review%20Paper%20
%20Tackling%20a%20crisis%
20for%20the%20health%20an
d%20wealth%20of%20nations
_1.pdf
(see page 3)
Try going to amr-review.org
and opening the December
2014 document. This
reference is on page 3.
Week 2 – Current affairs: The super bug
Date
MONDAY MAY 11
Short fact
Antibiotic resistance is not
coming – it is here right now
Long fact
Antibiotic resistance is not coming – it is here now
Antibiotic resistance happens when bacteria mutate in
response to antibiotic use .
Antibiotic resistance is a global issue and affecting
Australians today. You may have already heard of
resistant strains, sometimes referred to as ‘superbugs’,
like MRSA - Methicillin-resistant Staphylococcus
aureus
Multi-drug resistant E. coli in urinary tract infections is
present in Australia. Failure of the last resort antibiotic
treatment for the sexually transmitted infection
gonorrhoea has even occurred in Australia.
In April 2014, the World Health Organization (WHO)
released the first global report on antibiotic resistance.
Reference
Ref: taken from our AAW ‘Fact Sheet’
http://www.nps.org.au/medicines/infections
-and-infestations/antibiotics/forindividuals/what-is-antibiotic-resistance
http://www.nps.org.au/publications/healthprofessional/health-newsevidence/2014/antimicrobial-resistance
E coli reference:
‘antibiotic resistance remains a serious
health threat despite discovery’ media
release from 13 Jan, 2015
Gonorrhoea reference: AAW 2014 fact
sheet.
The report confirmed high rates of antibiotic resistance
in bacteria that cause common community and hospital
infections (eg, pneumonia, urinary tract infections)
around the world.
TUESDAY MAY 12
Don’t ask for antibiotics when
you don’t need them
Antibiotics are a dying breed.
Don’t be part of the problem: don’t ask for antibiotics
when you don’t need them.
1 in 5 Australians expect antibiotics for viruses like a
Reference: from Evaluation of the RAR
Program Summary Report, September,
2014, National Consumer Survey
cold or flu, and 17% would ask a doctor to prescribe
antibiotics, even though they won’t work on a viral
infection.
WEDNESDAY MAY
13
Australians take a lot of
antibiotics
Australians take A LOT of antibiotics.
Australia has one of the higher rates of antibiotic use in
the OECD. 24 million antibiotic prescriptions are written
in Australia each year. Put in perspective, that’s
enough for one prescription for every Australian.
Reference and graph: graph:
http://www.oecdilibrary.org/sites/health_glance-2011en/04/11/index.html;jsessionid=1m9l6pqjd3
gpn.x-oecd-live03?itemId=/content/chapter/health_glance2011-39en&_csp_=db5be54dd412d545669fd5afad
63b56d
http://www.nps.org.au/media-centre/mediareleases/repository/antibiotic-resistanceremains-a-serious-health-threat-despitediscovery
http://www.oecd-ilibrary.org/social-issuesmigration-health/health-at-a-glance2013/overall-volume-of-antibioticsprescribed-2010-or-nearestyear_health_glance-2013-graph99-en
THURSDAY MAY
14
The pipeline of new antibiotics is
drying up
“They’ll just make new, stronger antibiotics…”:
A common misconception is that when we run out of
effective antibiotics for common infections, we’ll just
develop more. In fact, new antibiotics are rare, and the
once large number of pharmaceutical companies
investing in antibiotic research has dwindled. The most
recent discovery, teixobactin, still needs to undergo
further studies and testing in humans, which will take
Reference http://www.nps.org.au/mediacentre/media-releases/repository/antibioticresistance-remains-a-serious-health-threatdespite-discovery)
Antibiotic development is dwindling graph
http://www.cdc.gov/getsmart/week/downloa
ds/gsw-factsheet-future.pdf)
many years, but even then it won’t be effective on all
bacterial infections.
FRIDAY MAY 15–
*WEEKEND
SUPER FACT*
Antibiotic resistance is one of
the greatest threats to human
health today
Antibiotic resistance is one of the greatest threats to
human health today.
The World Health Organization has identified antibiotic
resistance as “one of the greatest threats to human
health today … no longer a prediction for the future, it
is happening right now in every region of the world and
has the potential to affect anyone, of any age, in any
country”.
reference:
http://www.cdc.gov/drugresistance/p
df/ar-threats-2013-508.pdf
http://www.who.int/mediacentre/news/relea
ses/2014/amr-report/en/
A 2013 report estimated that in the United States every
year, two million people fall ill and 23,000 people die
from antibiotic-resistant infections.
The problem is growing. Preserve the miracle of
antibiotics.
Week 3 – What if: Imagine a world without antibiotics
Date
MONDAY MAY 18
Short fact
Imagine a world without
antibiotics
Long fact
POST ANTIBIOTIC-ERA
The World Health Organization is warning us that we
may be heading towards a “post-antibiotic era” – in
which common infections and minor injuries can kill.
Can you imagine a world without antibiotics? According
to the White House’s National Strategy for Combating
Reference
Ref:
http://www.who.int/mediacentre/news/rele
ases/2014/amr-report/en/
http://www.cdc.gov/drugresistance/pdf/car
b_national_strategy.pdf
Antibiotic Resistant Bacteria, “in a world with few
effective antibiotics, modern medical advances such as
surgery, transplants, and chemotherapy may no longer
be viable due to the threat of infection.”
TUESDAY MAY
19
What if you develop an infection
that is resistant to antibiotics?
What if you develop an infection that is resistant to
antibiotics?
If you or a memberof your family develop an antibioticresistant infection, you will have the infection for longer,
you may be more likely to have complications from the
infection, you could remain infectious for longer and
pass your infection to other people. And some antibiotic
resistant infections could in fact become untreatable.
WEDNESDAY
MAY 20
Antibiotic resistance knows no
geographical bounds
Superbug stowaways can hitch a ride with travellers
Travellers can return to Australia infected with multidrug-resistant organisms, particularly ones that cause
tuberculosis, gonorrhoea or hospital-acquired
infections. Patients with resistant bacteria faced
extended hospital stays of 1 to 4 months.
Ref: AAW 2014 fact sheet
http://www.nps.org.au/medicines/infection
s-and-infestations/antibiotics/forindividuals/what-is-antibiotic-resistance
Ref:
http://www.nps.org.au/publications/healthprofessional/health-newsevidence/2014/superbug-stowaways
Such complications could become commonplace if
antibiotic resistance continues its uncontrolled
geographical spread.
THURSDAY MAY
21
A precious resource is losing its
power
“A precious resource” is losing its power.
According to the White House’s National Strategy for
Combating Antibiotic Resistance, “antibiotics are a
precious resource” and “preserving its usefulness will
require cooperation and collaboration.”
Everyone has a part to play in the fight against antibiotic
http://www.cdc.gov/drugresistance/pdf/car
b_national_strategy.pdf
resistance.
FRIDAY MAY 22–
*WEEKEND
SUPER FACT*
Antibiotic resistance in 2050: 10
million deaths a year?
Where will you be in 2050?
A UK report has estimated that a continued rise in
antibiotic resistance by 2050 would lead to 10 million
people dying every year with a financial cost to the
world of up to US$100 trillion.
Reference: review on Antimicrobial
Resistance, Amr-review.org
Full reference
http://www.jpiamr.eu/wpcontent/uploads/2014/12/AMR-ReviewPaper-Tackling-a-crisis-for-the-health-andwealth-of-nations_1-2.pdf
We need to act now to stop the spread of antibiotic
resistant bacteria.
Week 4 – Here and now: Colds and flu — what you can do
Date
MONDAY MAY 25
TUESDAY MAY 26
Short fact
Antibiotic-resistant bacteria can
develop in your body after a
course of antibiotics
Long fact
Think of your body as a human Petri dish
Reference
Reference: AAW 2014 fact sheet
If you have recently taken antibiotics, you can have
antibiotic resistant bacteria develop then persist in
your body for as long as twelve months. They can
multiply and become strong enough to resist
antibiotics in the future. These antibiotic-resistant
bacteria can then be passed on to family members or
other people in the community.
http://www.nps.org.au/medicines/infectionsand-infestations/antibiotics/forindividuals/what-is-antibiotic-resistance
Antibiotics don’t work for all
infections
Antibiotics do not work for all infections. They don’t
treat viral colds and flu; and most coughs, earaches,
sinus congestion and sore throats will get better
without antibiotics.
Reference: NPS website
http://www.nps.org.au/medicines/infectionsand-infestations/antibiotics/forindividuals/antibiotics-for-respiratory-tract-
If you are usually healthy and well, your immune
system will take care of most respiratory tract
infections— including viral and some bacterial
infections — by itself. Be part of the solution: don’t
demand antibiotics; tell your doctor that you only want
antibiotics if they are truly necessary.
WEDNESDAY
MAY 27
THURSDAY MAY
28
Green snot doesn’t mean a lot
Simple steps to avoid infections
infections/for-individuals/overview
Green snot doesn’t mean a lot.
Reference: AAW 2014 fact sheet
Coloured mucous or ‘snot’ isn’t always a sign of a
bacterial infection. Green or yellow coloured snot can
in fact be a sign that your immune system is fighting
your infection, and not that your illness is getting
worse. That also goes for other symptoms including
cough, sore throat, earaches and fever. While some
people with these symptoms will need antibiotics,
most people won’t and will get better without
antibiotics. Of course, if your symptoms continue to
get worse, see your doctor.
http://www.nps.org.au/conditions/respiratoryproblems/respiratory-tract-infections/forindividuals/conditions/common-cold/forindividuals/symptoms
Be part of the solution: simple steps to avoid
infections.
Reference: NPS website
It’s easy to take simple steps to avoid infections and
to stop them from spreading. You can do this by
washing your hands, coughing and sneezing into a
tissue and throwing it away, and staying home when
you are sick. Staying home when you are sick will
help you get over the infection faster, and it will also
mean that you won’t spread your infection. Having a
flu vaccination every year before winter can help to
protect you from getting the flu.
http://www.nps.org.au/conditions/respiratoryproblems/respiratory-tract-infections/forindividuals/prevention
FRIDAY MAY 29
*WEEKEND
SUPER FACT*
Antibiotics won’t make your
cold or flu better faster.
We know what needs to be done to solve the crisis…
we’re just not doing it.
Think before you ask. Antibiotics WILL NOT:
Backup fact
Sharing antibiotics can
contribute to antibiotic
resistance
Reference: NPS website
http://www.nps.org.au/medicines/infectionsand-infestations/antibiotics/forindividuals/antibiotics-dont-kill-viruses
help a cold or flu get better faster
stop a cold or flu from getting worse
stop a cold or flu from spreading to other people.
Never share antibiotics with another person.
Each antibiotic treats specific bacteria. Using the
wrong antibiotic can cause resistant bacteria to grow,
and may lead to a longer and more serious infection
by delaying correct treatment. Properly dispose of any
leftover antibiotics—don’t save them for future use.
:
Our cold messaging on website http://www.nps.org.au/conditions/respiratory-problems/respiratory-tract-infections/forindividuals/conditions/common-cold/for-individuals/medicines-and-treatments
Cold prevention messaging on website http://www.nps.org.au/conditions/respiratory-problems/respiratory-tract-infections/forindividuals/conditions/common-cold/for-individuals/prevention