Lay-language_summary
advertisement
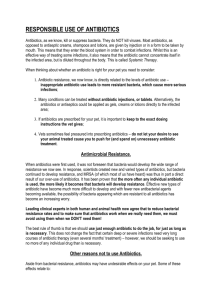
Lay-language summary of talk Microbes, particularly bacteria, have in-built mechanisms to develop resistance to medicines designed to kill them – resulting in “survival of the fittest”. This is known as antimicrobial/antibiotic resistance and was predicted by the discoverer of penicillin, Sir Alexander Fleming, in 1945 when he accepted his Nobel Prize. Initially, when bacteria developed resistance to an antibiotic, we doctors (and vets) reached for another, often newer, antibiotic. Sadly though, the golden era of new antibiotic discovery finished in the late 1980s, since when we have had very few new antibiotics. We now have a picture across the world of people dying because they have infections that do not respond to antibiotics: some 25,000 each year in Europe, with a conservative estimate of 23,000 deaths each year in the United States and one child aged under five years every five minutes in South East Asia. This has a terrible cost to society, both in suffering and loss, and economically impacts on the health service and broader economy. If AMR continues to rise at the rate it is, and we do not have new antibiotics, then our modern medical system is threatened. We use antibiotics to protect people from infection when they have major surgery, for instance replacement joints and caesarian sections. Antibiotics are the cornerstone of modern cancer therapy, and transplant surgery would be impossible without antibiotics. Indeed, we can envisage a post-antibiotic era where people die from infections caught from a scratch or even from simple bacterial pneumonias. The conditions that promote antibiotic resistance are clear: over use of antibiotics; inappropriate use of antibiotics; the wrong dose or time period of antibiotic use; and false and counterfeit medicines. We all have a role to play in protecting the antibiotics we have, including not using antibiotics for viral infections such as colds, only using antibiotics when they should be used and then changing to the correct antibiotic as bacterial culture results become available, as well as ensuring proper prescribing, dispensing and use. This requires healthcare workers, including nurse prescribers, dentists and their equivalents in the veterinary field, to understand the issues, practise responsible prescribing using appropriate diagnostics as well as adhering to obsessional infection control in healthcare facilities and at home. We also need to ensure that antibiotics used in animals for growth promotion in the place of proper hygiene is phased out and focus development activity on producing vaccines to protect animals and aquaculture from infection. But, there is also the problem of market failure in that insufficient funding is available to produce enough basic research to find new targets and develop new antibiotics. Meanwhile, once a new antibiotic is available, there is a public health need to restrict use in order to protect from the development of resistance in bacteria, yet that reduces any potential profit for the pharma companies. We need innovative funding solutions to this problem. By working together globally we can start to solve this problem and one of the first important moves is the World Health Organization’s Global Action Plan, which should be agreed at the World Health Assembly in May 2015 and tasks every country to develop a national action plan and report back on progress.