Supplemental Data: Survey information The survey was conducted
advertisement
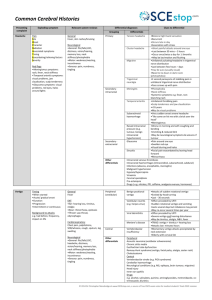
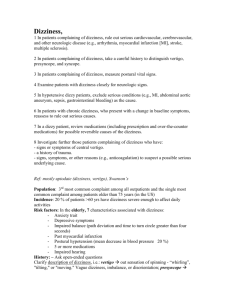
Supplemental Data: Survey information The survey was conducted from September 16, 2013 to February 2 nd, 2014. The study was designed by neurologists, a psychologist and a physicist who developed a videooculography device to perform quantitative HIT. All of the developers have longstanding experience in examining patients with vertigo and dizziness (vertigo outpatient centers). Pilot testing was performed for 3 months before distribution engaging several experienced and naive neurologists (neurological departments, practitioner). It contained 14 questions with either single or multiple-choice answer format; see original survey on supplemental data. Question #2 required multiple answers in %. Forward was not possible unless the sum added up to 100%. The average duration participants took to answer the survey was 336±197 sec (median 286 sec), i.e. about 4.7 minutes. The link to the survey was posted on the homepage of the German Neurological Society (DGN) and the survey was also announced in official quarterly email letters of the DGN to their members. The survey was not sponsored by any company. There were no financial incentives to participation or non-material benefits offered. Anonymity was guaranteed since participants were not asked for names or personal data allowing any identification. Repetitive participation was largely excluded by setting a cookie on the computer used. Response to each question was mandatory to proceed. The demographics and clinical training history obtained on participants is given in the text. More than 50% of respondents indicated that from all their everyday patients less than 25% present with vertigo; in 42% of respondents 26-50% present with vertigo. The survey was developed using LimeSurvey (www.limesurvey.org, version 2.00+, build 130802), an open-source tool (GNU, general public license), running on a server in the Department of Neurology, Luebeck. Statistics Statistical calculations were performed using SPSS (IBM SPSS Inc., Armonk, NY; version 22.0.0.1). The examinations to differentiate peripheral vestibular from central cause (Fig. 1A) differed between specialists and residents in the categories “medical history” (Mann-Whitney U-Test, z = 3.2, p = 0.002), “normal cMRI” (z = -2.3, p = 0.023) and “normal cCT” (z = -3.5, p = 0.001). The relative importance of specific ocular motor and other neurologic signs for diagnosis differed significantly between the categories (Friedman-Test, Chi²=29.9, df=3, p < 0.001, Fig. 1B). Post-hoc Wilcoxon tests showed significant differences between “Head impulse test” and “no skew deviation” (z = -3.5, p < 0.001) as well as “horizontal-torsional nystagmus” (z = -3.0, p = 0.003). Furthermore “No additional neurologic signs” differed significantly to “horizontal-torsional nystagmus” (z=-4.0, p < 0.001) and “no skew deviation” (z = -4.3, p < 0.001). Limitations of the study The study design bears some inherent confounds. Five percent is an expected and reasonable yet not representative number of participants in this kind of internet based survey. Although the survey comprised a fairly large number of neurologists it represents the diagnostic approach of only a minority of neurologists in Germany. Participating neurologists were probably more interested and experienced in dizziness than non-participants. Therefore the high frequency of clinically applied HIT indicated by the respondents may not be representative. The study can also not answer whether participants' responses are based on clinical or theoretical grounds (e.g., published literature, lectures at meetings, local subspecialist neuro-otology consultants or practical experience with vertigo patients). There were no uncued or multiple choice questions asked that might have assessed the knowledge of those individuals who stated they frequently relied on bedside skills. Accordingly, it remains unknown whether the specific skills are correctly and consistently performed at the bedside (i.e., whether confidence matches competence), since these two may be dissociated [1]. But this was not the primary goal of this survey. We consider it likely that non-participants were less aware of the HIT and that their self-confidence in taking patient's history and HIT is even much smaller. Thus, even the participants interested in diagnosing vertigo lack selfconfidence in their own clinical skills. 1. Friedman CP, Gatti GG, Franz TM, Murphy GC, Wolf FM, Heckerling PS, Fine PL, Miller TM, Elstein AS (2005) Do physicians know when their diagnoses are correct? Implications for decision support and error reduction. J Gen Intern Med 20:334-339