Insulin Infusion Protocol - UT Health : The University of Toledo
advertisement

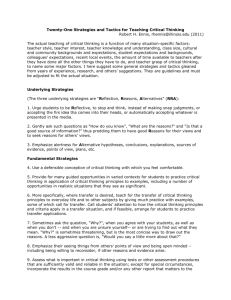
Insulin Infusion Protocol Doctor’s Orders Initiating the Insulin Infusion Blood Glucose (BG) Monitoring Changing the Insulin Infusion Rate INSULIN (Regular) INFUSION PROTOCOL Mixed as standard concentration (100 units in 100mL 0.9%NaCL) Priming: Flush 50 ml of infusion through all IV tubing before infusion begins (to saturate the insulin binding sites in the tubing) May be infused through central line or peripheral IV Use of this scale is based on HOURLY Blood Glucose (BG) Monitoring. If monitoring > than hourly, refer to calculating of drip in “Changing the Insulin Infusion Rate” section below. Target blood glucose range 120-180 mg/dL Blood glucose (BG) samples may be obtained through indwelling vascular device or by finger stick. Physicians are determining the starting rate of insulin infusions. Refer to the order in Care Organizer for the specific rate to begin the insulin infusion. Round to the nearest 0.5 unit for the initial infusion rate. 1. Check BG hourly until stable (defined as 3 consecutive values within target range), with adjustment of infusion rate as indicated) 2. Once stable, change BG monitoring to every 2 hours, with adjustment of infusion rate as indicated. 3. Once stable with every 2 hour BG checks for 12 to 24 hours, change monitoring to every 4 hours, with adjustment of infusion rate as indicated, only if: No significant changes in clinical condition, AND No significant change in nutritional intake. 4. Check BG more frequently, as indicated, for all BG </= 70mg/dL. 5. If any of the following occur, resume hourly BG monitoring until BG is again stable (3 consecutive BG values within target range): Any significant change in insulin infusion rate (i.e. BG out of target range) Significant changes in clinical condition Initiation or cessation of pressor or steroid therapy Initiation or cessation of renal replacement therapy (hemodialysis, CVVHD, etc.) Initiation, cessation or rate change of nutritional support (TPN, tube feeds, etc.) Note: Follow the treatment across from the blood glucose result range BG <120 mg/dl STOP INSULIN INFUSION 1. First calculate the change in the BG per hour (Current BG subtracted from previous BG then divided by hour(s), depending upon when the last blood glucose was taken.) Example: BG at 2PM is 150 mg/dL and it is now 4PM with BG 120 mg/dL. (150-120=30mg/dL difference divided by 2 hours equals a 15 mg/dL/hr decrease. 2. Take the calculation to determine which column (2, 3 or 4) to follow based on Page 1 of 2 the current BG. 3. When calculating a rate change, round to the nearest 0.5 unit. Example: Round 4.78 to nearest 0.5 unit = 5 units/hr Round 2.35 to nearest 0.5 unit = 2.5 units/hr Current Blood Glucose (CBG >250 181-250 120-180 Column 2 OR If CBG decreased by <50 mg/dl/hr or it is higher than previous CBG check then: Increase infusion rate by 50% (1.5 x current rate) Increase infusion rate by 25% (1.25 x rate) No Change Column 3 Column 4 If CBG decreases by 5070 mg/dl/hr then: If CBG decreases by >70 mg/dl/hr then: No Change No Change Decrease infusion rate by 10% (0.9 x rate) No Change Decrease infusion rate by 20% (0.8 x rate) Decrease infusion rate by 25% (0.75 x rate) STOP infusion <120 STOP infusion STOP infusion If infusion has been stopped and BG >180 mg/dl, restart infusion at 50% (0.5 x rate) of previous rate and recheck BG in 60 minutes Page 2 of 2