IPS Press Release
advertisement
INDIANA PAIN SOCIETY PRESS RELEASE 10/6/12
QUESTIONS ABOUT EPIDURAL STEROID INJECTIONS
Recently Indiana became one of the many states involved in a large-scale series of
meningitis infections occurring due to epidural steroid injections using
contaminated vials of methylprednisolone acetate obtained from a Massachusetts
compounding pharmacy. As of today, there are 91 confirmed infections and 7
deaths in 9 states. Also as of today, 8 people in Indiana have confirmed fungal
infections out of the 1,409 calculated to be at risk in the state. The incubation
time may require weeks to months therefore many more may develop meningitis,
stroke, or death due to the contaminated vials. In Indiana, only 6 clinics and one
hospital received vials of potentially infectious material from the New England
Compounding Center (NECC) also known as New England Compounding
Pharmacy. This pharmacy is located in Framingham Massachusetts and since
Friday 10/5/12 has recalled all products in all classes, having effectively ceased
operations on 10/3/12 by surrendering its pharmacy license to the Massachusetts
Board of Registration in Pharmacy. The recall of methylprednisolone acetate
alone includes over 17,686 vials from 23 states. Each vial may have be used in
several patients as was the case with Wellspring Pain Clinic in Columbus Indiana.
Epidural injections in Indiana were administered by 5 clinics and one hospital.
An additional Indiana clinic used the potentially contaminated vials for joint
injections only. The CDC recently warned that joint injections with
contaminated aspergillus fungus containing vials may have the potential to
develop infections.
All the clinics and hospitals involved nationwide and in Indiana are attempting to
contact patients to warn them of potential symptoms that may be a prelude to the
development of a severe or fatal infection.
The institutions involved in Indiana and physicians performing epidural
injections working at these institutions include:
1. Wellspring Pain Clinic and associated internal surgery center, Columbus
Indiana Drs. R. Andrew Robertson and Arman Borhan, 309 patients
2. Midwest Surgery Center and Union Hospital, Terre Haute, Indiana, Dr
Thomas Pendergast, 90 patients
3. St Mary’s Surgicare Cross Point, Evansville, Indiana, 560 patients
4. South Bend Clinic, South Bend, Indiana Kathryn Park, MD, 50 patients
5. OSMC, SouthBend, Indiana Drs. Christopher Annis, David Beatty, Gene
Grove, and Jonathan Schrock, 400 patients
6. Fort Wayne Physical Medicine, Dr Mark Reecer, did not perform epidural
injections but instead used the medication for joint injections. Unknown
number at risk since these are joint injections only.
The website www.cdc.gov has the most up to date nationwide information
about the meningitis outbreak.
ARE EPIDURAL STEROID INJECTIONS SAFE NOW? Answer: Yes, as safe
as in the past, as long as commercially manufactured steroids are used.
Compounding pharmacies steroids that are preservative free and
manufactured in bulk quantities should not be used for epidural steroid
injections given recent and past outbreaks of meningitis using compounded
products. There are 140 hospitals and over 200+ physicians everyday in
Indiana potentially administering commercially available epidural steroids
that were unaffected by the recall and meningitis. To ensure maximum safety,
ask your physician to use only name brand “DEPOMEDROL” or the generic
equivalent and to exclude using any preservative free epidural steroid
obtained from compounding pharmacies.
QUESTIONS AND ANSWERS ABOUT STEROID INJECTIONS AND
COMPOUNDING PHARMACIES
1. What are the most commonly used steroids used for epidural steroid
injections? Methylprednisolone acetate, dexamethasone, betamethasone, and
triamcinolone
2. Are these approved for epidural injections? Answer: No. No steroid
medications have approval by the FDA for epidural injection at this time. None
of these were ever submitted to the manufacturers for approval by the FDA for
epidural usage, even though they have been used in the spine since the 1950s.
Their use was accepted long before the FDA required medications be submitted
for approval. They are commonly used “off label”, an accepted use, as are many
other medications.
3. What is methylprednisolone acetate? Answer: It is a corticosteroid, originally
made in 1958 by chemically modifying hydrocortisone (cortisol). Hydrocortisone
is a naturally occurring substance in the adrenal glands of man and animals, but
may also be synthesized from modifying cholesterol and other bile salts, although
there are many ways to obtain the substance through chemical synthesis,
including using yeasts and through a strain of aspergillus (not the one causing the
current outbreak). Methylprednisolone acetate has powerful anti-inflammatory
properties and is used as an injection for many purposes including joint
injections, intramuscular injections, and epidural injections.
4. Where is the raw material methylprednisolone manufactured? Answer:
Effectively all supplies (similar to many medications in this country) come from
China where pharmaceutical oversight is far less than in the US. It is supplied to
US pharmacies and manufacturers as an off white powder via one of seven
Chinese suppliers.
5. How is the methylprednisolone sterilized? Answer: Since it is a powder, prior
to mixing with any other chemicals or medications it is autoclaved at a high
enough pressure and temperature to sterilize the drug. Methylprednisolone does
not dissolve in liquids, therefore is marketed to doctors as a “suspension” of
particles. Suspensions, unlike solutions of drugs, cannot be sterilized by filtration
via a 0.2micron pore filter since the particle size of the suspension is too large for
the filter. Autoclaving must be done at appropriate temperatures and pressures
so as not to destroy the methylprednisolone, which melts at 192 degrees Celsius.
6. Is it possible for the raw material methylprednisolone supplied by the Chinese
manufacturers be contaminated by aspergillus or bacteria? Answer: Yes. This is
why sterilization must be performed before combining the raw product with any
other materials.
7. What are some of the reasons aspergillus could have contaminated the lots
distributed? Answer: Inadequate sterilization (use of less than 121 degrees
Celsius for less than 15 min time or failure to use much longer autoclave times for
larger quantities of bulk material), contamination during transfer to another
container, contamination of the water and other chemicals used in the final
product.
8. What are the sources of the Aspergillus fumigatus that is causing the
meningitis outbreak? Answer: Aspergillus fumigatus is a common fungus found
in the environment. The spores of the fungus are breathed in by the hundreds
everyday by all of us without causing pathology. However, those with immune
compromise (cancer, leukemia, HIV, etc) or with sinus/asthma issues may
harbor the fungus in tissues and secretions. The vials three lots of
methylprednisolone acetate from the New England Compounding Center have
been recalled with growth of fungi found in at least one of the lots. These lots
were produced and distributed between July 1 and September 26, 2012. It is
probable (based on current information) that the outbreaks were due to vials of
methylprednisolone contaminated with Aspergillus fumigatus.
9. What is a compounding pharmacy and what do they do? Answer: A
compounding pharmacy is an outgrowth of the art and science of pharmacy in
which drug combinations are mixed specifically for a single patient. This is
contrary to manufacturing of a drug in which a non-tailored, drug is produced in
large quantities for sale to the general public or to physicians. It is also different
than wholesale distribution of a drug. Compounding pharmacies link a specific
compounded drug to a specific patient via a prescription. Compounding
pharmacies may not create an identical replication of a commercially available
drug. If the drug is not commercially available due to unavailability due to
manufacture backorder, discontinuation, or supply issues, then the compounding
pharmacy may create a replica of the erstwhile available commercial drug. There
are now up to 7,500 specialty compounding pharmacies in the US. The FDA has
raised questions about the accuracy of compounding pharmacies in a 2006 study
conducted by the Center for Drug Evaluation Research Office of Compliance in
which assays were made of drugs obtained through compounding pharmacies.
The FDA found potency varied between 68 and 268% of the amount labeled by
the compounding pharmacy
http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Pharm
acyCompounding/ucm204237.htm
10. Was the New England Compounding Center creating specifically
compounded drugs via a prescription for each patient? Answer: No. The
pharmacy was making massive quantities of the medication, not linked to specific
patients, and not tailored for a specific patient needs. They were engaged in
manufacturing of a commercial drug in large scale quantities as may be seen via
the recall of more than 17,000 vials of methylprednisolone acetate preservative
free nationwide. According to the Boston Globe in a story published October 6,
2012, the company has been investigated more than once for complaints. “New
England Compounding has been investigated by state and federal regulators
several times, in some cases for overstepping its bounds as a compounding
pharmacy and venturing into manufacturing. The FDA received three complaints
about the company in 2002 and 2003 involving its preparation of
methylprednisolone acetate, one of the complaints concerned lapses in sterile
procedures, leading to investigations by the state and the FDA, said
Massachusetts health officials.” A 2006 warning letter about NECC
compounding practices is included in Appendix D.
On 10/5/12, the Massachusetts Department of Public Health released a statement
that said pharmacists and pharmacies are “only permitted to dispense and
compound medication pursuant to a prescription from a registered practitioner
for an individual patient.” New England Compounding Center is located in
Framingham, Massachusetts. Appendix C contains other FDA warning letters to
compounding pharmacies engaged in manufacturing.
11. Who had regulatory authority over the New England Compounding Center?
Answer: Ostensibly the state of Massachusetts was responsible for their licensure
and oversight, however the FDA is also responsible for “outsourced” sales (sales
to doctors offices). It is unclear if the FDA was involved in any monitoring or
enforcement activity regarding compounding pharmacy outsourcing. The FDA
has struggled to regulate compounding pharmacies in part to their resistance to
regulation but also because federal court cases such as Franck’s in Florida, the
FDA has been told it may not have the authority to regulate compounding
pharmacies. That case is currently on appeal. It is also unclear how the
Massachusetts board of pharmacy would rubber stamp the manufacturing role of
New England Compounding Center and permitted massive sales of medications
nationwide not tied to a specific patient. The International Academy of
Compounding Pharmacists lists New England Compounding Rx as one of its
members. However, the compounding pharmacy never applied for accreditation
to the Pharmacy Compounding Accreditation Board that has established
standards for compounding according to a story in the New York Times 10/4/12.
12. What role do Indiana laws have in determining sales from out of state
pharmacies or compounding pharmacies? Answer: Indiana laws are very sparse
on non resident pharmacies. According to IC 25-26-17, the out of state
pharmacy must register with the board of pharmacy in Indiana, must show
verification they meet the licensure requirements in their own state, must answer
questions posed to the pharmacy by the board, must keep records of
prescriptions given to patients (but not physicians or clinics), and must have an
800 number for patients to access the pharmacy. Effectively, these are the only
rules non-resident pharmacies must follow. Unless they do 25% or more of their
business via the internet, then there are no accreditation requirements via the
National Association of Boards of Pharmacy's Verified Internet Pharmacy
Practice Sites and National Association of Boards of Pharmacy. NECC is not
listed as a member of the former group.
Furthermore, all registration requirements may be waived by the Indiana Board
of Pharmacy for out of state pharmacies that “only dispenses drugs to Indiana in
limited transactions”. There are no Indiana requirements for site visits, detailed
report of operations, reports of citations or actions taken against the out of state
pharmacy, or that there be any standards followed that are equivalent to those
required by our own state pharmacist and pharmacies. Indiana is completely
dependent on the non-resident state pharmacy board to adequately regulate nonresident (out of state) pharmacies with a small internet presence compared to
total sales.
13. Was the New England Compounding Center or New England Compounding
Pharmacy registered with the pharmacy board to do business in Indiana?
Answer: Yes. They hold license # 64000484A and show no actions taken against
them.
14. Are compounding pharmacies subject to oversight by the FDA? Answer:
There is limited oversight of compounding pharmacies at the federal level.
Compounding pharmacies sometimes state in their literature they are not subject
to FDA regulation. For a 2003 Congressional testimony by the FDA on the
difficulties of regulating compounding pharmacies see
http://www.fda.gov/NewsEvents/Testimony/ucm115010.htm
15. Why do doctors order from compounding pharmacies? Answer:
Compounding pharmacies are supposed to create a compound specific to that
patient and when used legitimately for that purpose, doctors order for
compounding pharmacies when a. there is not an equivalent commercial
product available due to shortages or discontinuation, or b. due to unique
combinations of medications that may benefit a patient. Other reasons include
less regulation of product, ability to compound non-FDA approved medications
into the final product, cost savings, and removal of specific objectionable
components of commercial products.
16. Were there shortage of commercially available methylprednisolone during the
time the NECC manufactured the contaminated vials? Answer: No shortages for
methylprednisolone were reported by the FDA site tracking drug shortages. Our
office noted shortage in supply from one distributor of 40mg methylprednisolone
at that time, but the medication was readily obtained from other distributors.
17. Have there been other infections noted when compounding pharmacies made
injectable corticosteroids? Answer: Yes. Well publicized in the pain medicine
literature were reports in California in 2001 in which there were 3 deaths and 11
infections of a bacteria, serratia marcesens, from a steroid produced by a
compounding pharmacy. There was also a report in 2002 of a fungal injection
leading to death and four patients developed meningitis when a South Carolina
compounding pharmacy manufactured en masse injectable methylprednisolone
acetate that was subsequently distributed throughout 11 states. More
information is included in Appendix B.
18. Have there been other recalls of injectable methylprednisolone acetate?
Answer: Yes. Franck’s Compounding Pharmacy was ordered by the FDA Aug 22,
2012 to recall 8 vials manufactured between 11/21/2011 and 05/21/2012 due to
bacteria and fungi found in the compounding room. In September 2002, Urgent
Care Pharmacy, a compounding pharmacy in Spartansburg, SC, recalled all lots
of one of its injectable drugs, methylprednisolone acetate, after four patients
treated with this product developed a rare fungal meningitis.
19. Since there were no major drug shortages of methylprednisolone in 2012 and
given that compounding pharmacies were known to have risks of mass infection
of the population from steroids, then why were Indiana physicians ordering
medications from compounding pharmacies? Answer: Partially due to fear of
litigation promulgated by those in the past that received injections of epidural
steroids then later claimed arachnoiditis (permanent inflammation and spinal
damage). The steroid injections were frequently followed by spine surgery that is
a much higher likelihood of causing spinal injury compared to epidural steroid
injections. Some of these unfortunate individuals make claims about epidural
steroids causing long term pain and weakness (arachnoiditis) stating incorrectly
that the steroids contain “antifreeze” or “brake fluid” (they do not). Some doctors
have been lulled into believing this argument. The arachnoiditis patients claim
injury, at least in part, due to the preservatives contained in vials of
methylprednisolone. Some have developed websites to assist other patients who
want to bring litigation against their physicians. Compounding pharmacies are
the only way to eradicate the preservatives since there is no preservative free
commercial preparation. However, by removing the
preservatives/antimicrobials, the potential for infection increases. There exists
only very circumstantial and limited medical evidence for any long term harm
acquired due to preservative/antimicrobial containing epidural steroids.
20. Are there other reasons doctors use compounding pharmacies for injectable
steroids? Answer: Yes. Costs for the steroid per patient may be lower when using
a compounding pharmacy compared to a commercial pharmacy. Heavy
advertising by compounding pharmacies in pain journals and at pain conferences
may sway doctors into believing compounding pharmacies are just as safe as
commercial pharmacies or that their products are actually safer than the
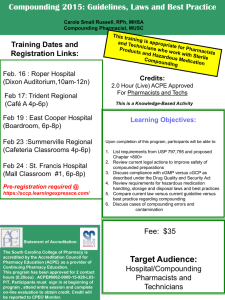
commercial product. An example of such advertising is included in Appendix A.
21. What preservatives are contained in commercial preparations of
methylprednisolone? Answer: It depends on the product. There are
fundamentally two commercial products available: multidose vials for injection
containing the following ingredients:
Depomedrol with preservative content: Each ml containsMethylprednisolone acetate..................................20 mg
40 mg
80 mg
Polyethylene glycol 3350....................................29.5 mg
29.1 mg 28.2 mg
Polysorbate 80 ....................................................1.97 mg
1.94 mg 1.88 mg
Monobasic sodium phosphate ..............................6.9 mg
6.8 mg 6.59 mg
Dibasic sodium phosphate USP..........................1.44 mg
1.42 mg 1.37 mg
Benzyl alcohol added as a preservative................9.3 mg
9.16 mg 8.88 mg
Saline is added to bring the volume to 1 ml.
And Depomedrol single dose vials
Depomedrol singe dose contains:
Methylprednisolone acetate
40 mg
80 mg
Polyethylene glycol 3350
29 mg
28 mg
Myristyl-gamma-picolinium chloride
0.195 mg 0.189 mg
Most physicians use the commercially available (non-compounded) single dose
vials for epidural injections and the multidose vials for joint injections. The
single dose vial contains the antimicrobial Myristyl-gamma-picolinium chloride
that is present only in very small amounts. It is toxic to rabbit retina and reduce
some of the knee reparative chemistry but does not seem to bother normal joints.
It may extremely rarely cause hypersensitivity reactions in humans. The
polyethylene glycol is a stabilizing agent for the suspension of
methylprednisolone. The multidose vials do have a variety of potentially toxic
elements to nerve tissue such as benzyl alcohol, but are not present in large
amounts.
22. How does the compounded medication differ from the commercial single
dose? Answer: The elimination of Myristyl-gamma-picolinium chloride is seen
in some preparations.
23. Can infections occur in the epidural space and can meningitis develop
without having contaminated vials? Answer: Yes, however these are rare
occurrences noted more with patient specific risk factors (obesity, diabetes,
immune system compromise) or contamination of the needle or solution injected
at the time of preparation. Outbreaks of series of infections in a clinic is usually
due to a break in sterile technique of the physician. Outbreaks simultaneously in
several clinics or hospitals is more likely due to contamination of mass
manufactured equipment or medications.
APPENDIX A
Example of the Type of Advertising Used by Compounding
Pharmacies (MasterPharm Taken Directly from their Website
10/5/12):
Preservative Free Steroid Injectables
Many patients cannot tolerate the preservatives, dyes, and allergens that are unfortunately present in many
commercially available medications. Patients who are sensitive to these irritating agents can experience adverse
side effects or reactions.
MasterPharm solves this problem effectively by preparing the medications they need without the use of any
irritating substances including the following:
Additives and fillers
Artificial colorings
Artificial flavorings
Casein
Chemicals
Dyes
Gluten
Preservatives
Milk derivates
Soy
Sweeteners
Wheat
Sterile, preservative-free preparation is helpful to many medications, including steroid injectables that are
commonly used by surgeons, hospital staff, and physicians to treat pain and inflammation in patients. Preservativefree steroid injections can be compounded using a variety of steroids including the following:
Triamcinolone Diacete
Methylprednisolone acetate
Depo Medrol
Matching the dosage forms, formulation, and strength of customized compounds to patient needs is advantageous
for the treatment of pain and inflammation. More importantly, our compounding services enable us to produce
medications that soothe inflammation without introducing the risk of adverse side effects and reactions to
substances in the medication.
APPENDIX B
2002 FUNGAL INFECTION AND DEATH FROM
COMPOUNDED STEROIDS
http://archives.thepilot.com/PilotLight/October2002/100702SteroidCame.
html
Steroid Came From Alternative Supplier
{5 states involved, agent was Exophiala dermatitidis
according to MMWR 51 from the CDC}
BY MATTHEW MORIARTY: Staff Writer
Officials at FirstHealth of the Carolinas say a shortage of a drug used to treat pain
forced the hospital to find an alternative supplier.
The Pain Clinic at FirstHealth Moore Regional Hospital was one of three centers in
North Carolina that received a batch of contaminated steroids from a South Carolina
compounding pharmacy, according to state health officials.
A 77-year-old Pinehurst woman who received an injection of the steroid in May died
Aug. 25 at Duke Medical Center from fungal meningitis.
At least two other people, including another patient of the Moore Regional pain clinic,
were diagnosed with meningitis and are being treated. According to the state, the
common thread appears to be the drug, methylprednisolone, which was made by
Urgent Care Pharmacy in Spartanburg.
“Due to a shortage of Depo-Medrol supplied by Upjohn Pharmaceuticals, we were
forced to find an alternative supplier of methylprednisolone,” said Tom Smith,
director of pharmacy and oncology for FirstHealth. “We contacted the supplier in
South Carolina after they were recommended to us by a colleague at another pain
clinic that had been using this supplier.
“As is our practice, we met with a representative from the pharmacy and discussed
their procedures with regard to everything from compounding of this drug to
ordering and shipping procedures. We verified that their license was in good standing
with South Carolina Board of Pharmacy since 1988. We also verified that North
Carolina Board of Pharmacy had the pharmacy listed as being registered with our
state as a mail order pharmacy.
“With this routine research completed, we placed our order in May and again in June
2002. Methylprednisolone is the only drug we have purchased from the Spartanburg
supplier.”
About 500 patients could have been injected with the steroid between May 6 and
July 15. The hospital sent letters to those patients. The drug was not used elsewhere
in the hospital.
According to the state, the drug was contaminated by a fungus. This case has raised
concerns about the safety of medications made by compounding pharmacies.
Local Company Responds
But the owner of a Southern Pines compounding pharmacy says there is no way that
mold could contaminate her company’s medicine.
Constance Anderson of Health Innovations Pharmacy said her pharmacy takes
special care to make sure all of its medicines are safe.
Compounding pharmacies make smaller batches of medicines on site. They are often
called up to make medications that are in short supply or no longer made by the
large pharmaceutical companies. The smaller batches of medicine can be
personalized. For example, if someone is allergic to a dye in a drug, a compounding
pharmacy can make the drug without the allergen.
Urgent Care Pharmacy made large quantities of the steroid and shipped it to
hospitals in five states. The steroid is injected into the spine or joints to treat pain.
Anderson’s pharmacy doesn’t make that type of compound.
“We chose not to compound those types of products,” Anderson said.
Anderson is interested in finding out how this medicine became contaminated. “It’s
important we find out what caused the contamination,” Anderson said.
It’s important for those already exposed to the medicine and for the safety of
Anderson’s future customers, she said.
Health Innovation pharmacists always test for sterility when making a drug,
Anderson said. Also, Health Innovations Pharmacy has a policy of making only small
amounts of compounds that are prescribed by doctors that the pharmacists know
and have a relationship with on a regular basis.
‘You Have to Be Careful’
Ray Burns, the founder of Urgent Care Pharmacy, denied that the drug from his
pharmacy was tainted.
A team of doctors and state health officials are investigating the cause of the
contamination. Anderson said buying from respected chemical companies is a good
way to ensure drugs won’t be contaminated.
“You have to be careful who you buy from,” she said. “We deal with reputable
chemical companies that do testing. They can even offer us analytical reports on the
tests.”
Individual states regulate compounding pharmacies. Every state has different rules,
Anderson said.
“They’ll come in and they’ll inspect you,” she said. Health Innovations Pharmacy is
routinely inspected, Anderson said.
Anderson also said there are pharmacies closer to FirstHealth Moore Regional
Hospital that can provide methylprednisolone. She said being in close proximity to
the doctors the pharmacists work with is important to her pharmacy.
“If we can’t drive it (the medicine) down the road and take it to them,” she said,
“then we don’t need to be doing it.”
2001 California Outbreak of Serracea Marcesens
Infections (11, with 3 deaths) from community
compounding pharmacy bethamethasone due to drug
shortage nationwide
http://cid.oxfordjournals.org/content/43/7/831.full.pdf
APPENDIX C
WARNING LETTER TO COMPOUNDING PHARMACY FROM
FDA 2001 FOR PRACTICES THAT WERE IDENTICAL TO
NECC:
Unique Pharmaceuticals, Ltd. 10-Oct-01
DEPARTMENT OF HEALTH & HUMAN SERVICES
Food and Drug Administration
Dallas District
4040 North Central Expressway
Dallas, Texas 75204-3145
October 10, 2001
Ref: 2002-DAL-WL-02
WARNING LETTER
CERTIFIED MAIL
RETURN RECEIPT REQUESTED
Mr. Daniel F. Volney, President
Unique Pharmaceuticals, Ltd.
5920 S. General Bruce Drive, #500
Temple, TX 76505
An inspection of your firm conducted by the Food and Drug Administration (FDA), the Texas Department of
Health, and the Texas State Board of Pharmacy, on August 2/4 & 16, and September 5, 2000, revealed
serious violations of the Federal Food, Drug, and Cosmetic Act (the Act).
While your firm purports to be a compounding pharmacy (as noted in your September 27, 2000, letter to the
FDA Investigator), the inspection disclosed that in the case of numerous drug products, your firm is not
preparing the drugs pursuant to valid prescription orders from licensed practitioners for individual patients.
Rather, Unique Pharmaceuticals, Ltd., an entity not registered with FDA, is manufacturing and distributing
drug products in large quantities, including drugs appearing to be copies of commercially available drug
products, to wholesale drug distributors for their subsequent distribution to hospitals, pharmacies, and
physicians. Eighty percent of the drugs prepared by your firm are not dispensed or sold directly to individual
patients.
During a three-month period, your firm prepared and distributed inordinate quantities of drug products
appearing to be copies of commercially available drugs, including, but not limited to, the following:
Dexamethasone Acetate for Injection 8mg/mL -38,650 vials
Triamcinolone Acetonide for Injection 40mg/mL -38,400 vials
Methylprednisolone Acetate for Injection 80mg/ml -18,400 vials
Methylprednisolone Acetate for Injection 40mg/mL -10,750 vials
Promethazine for Injection 50mg/mL -5000 vials
Estradiol Valerate for Injection 40mg/mL -2000 vials
Triamcinolone Diacetate for Injection 40mg/mL -2000 vials
Estradiol Cypionate for Injection 5mg/mL -1250 vials
Diphenhydramine for Injection 50mg/mL -1000 vials
Dicyclomine for Injection 10mg/mL -650 vials.
These activities plainly exceed the scope of the regular course of business of a pharmacy dispensing or
selling drugs at retail. Our findings are consistent with the Texas Department of Health Warning Letter dated
September 29, 2000, which indicates that your firm is manufacturing and distributing drugs to wholesalers in
Texas and other states and not exclusively to practitioners.
As you are aware, section 127 of the FDA Modernization Act of 1997 (FDAMA) amended the Federal Food,
Drug, and Cosmetic Act, adding section 503A. This provision became effective on November 21, 1998, and
sets forth the requirements that compounded products must meet to qualify for exemption from the new drug
(Section 505), certain adulteration (501 (a)(2)(B)), and misbranding (502(f)(l)) provisions of the Act. On
February 6, 2001, the United States Court of Appeals for the Ninth Circuit declared Section 503A of the Act
to be invalid in its entirety (Western States Medical Center v. Shalala, 238 F.3d 1090 (9th Cir. 2001)). On
August 24, 2001, the United States
Department of Justice appealed this decision to the U.S. Supreme Court. During the time that the appeal is
pending it is FDA?s position that section 503A is valid outside of the Ninth Circuit.
The drug products prepared by your firm do not qualify for exemptions from section 505, 502(f)(l), and 501
(a)(2)(B) provided under section 503A of the Act in that:
(1)Drug products including, but not limited to, the following:
Dexamethasone Acetate for Injection 8mg/mL
Triamcinolone Acetonide for Injection 40mg/mL
Methylprednisolone Acetate for Injection 80mg/ml
Methylprednisolone Acetate for Injection 40mg/mL
Promethazine for Injection 50mg/mL
Estradiol Valerate for Injection 40mg/mL
Triamcinolone Diacetate for Injection 40mg/mL
Estradiol Cypionate for Injection 5mg/mL
Diphenhydramine for Injection 50mg/mL
Dicyclomine for Injection 10mg/mL
are not being compounded for identified, individual patients based on prescription orders from licensed
practitioners as required by section 503A(a) of the Act. Instead, they are being distributed to wholesale drug
distributors for further sale to hospitals, pharmacies, and physicians; and
(2)Drug products including, but not limited to, the following:
Boron PF 2mg/mL for Injection
Cesium CL 100mg/mL for Injection
Co-Enzyme Q 20mg/mL for Injection
DHEA 10mg/mL for Injection
Echinacea 2% for Injection
Germanium Sesq 132 for Injection
Glucosamine 200rng/mL for Injection
Glycerrhizic Acid PF 8mg/mL for Injection
Lipoic Acid PF 25mg/mL for Injection
Melatonin 2.5mg/mL for Injection
Molybdenum 200mcg/mL for Injection
Pangamic Acid 250mg/mL for Injection
Rubidium 200mcg/mL for Injection
Strontium 1mg/mL PF for Injection
Vanadium 200mcg/mL PF for Injection
are being prepared using bulk drug substances that do not meet the requirements of section 503A(b)(l)(A) of
the Act; and
(3) A drug product that you prepare, Adenosine M.P. 250mg/mL for Injection, appears on the Withdrawn or
Removed Drug Product List" that was published in the Federal Register as a final rule and became effective
on April 7, 1999, and, therefore, does not comply with section 503A(b)(l)(C) of the Act; and
(4) Drug products, including, but not limited to, the following:
Dexamethasone Acetate for Injection 8mg/mL
Triamcinolone Acetonide for Injection 40mg/mL
Methylprednisolone Acetate for Injection 80mg/ml
Methylprednisolone Acetate for Injection 40mg/mL
Promethazine for Injection 50mg/mL
Estradiol Valerate for Injection 40mg/mL
Triamcinolone Diacetate for Injection 40mg/mL
Estradiol Cypionate for Injection 5mg/mL
Diphenhydramine for Injection 50mg/mL
Dicyclomine for Injection 10mg/mL
appear to be copies of commercially available drugs, are being prepared regularly or in inordinate quantities,
and therefore, do not comply with section 503A(b)(l)(D) of the Act The drug products that your firm prepares,
as noted above, are in violation of the Federal Food, Drug, and Cosmetic Act as follows:
Section 505
The referenced products are drugs within the meaning of section 201(g) of the Act which may not be
introduced or delivered for introduction into interstate commerce under section 505(a), since they are new
drugs within the meaning of section 201(p) and no approvals of any applications filed pursuant to section
505(b) or (j) are in effect for such drugs.
Section 502(f)(l)
The referenced drug products are misbranded within the meaning of section 502(f)(l) because they are
prescription drugs and their labeling fails to bear adequate directions for use under which a practitioner
licensed by law can use the drugs safely and for the purposes for which they are intended.
Section 502(o)
The referenced drug products are misbranded within the meaning of section 502(O) in that they were
manufactured in an establishment not duly registered under section 510 of the Act; and, they have not been
listed as required by section 510(j).
Section 502(a)
The referenced drug products are misbranded within the meaning of section 502(a) because they bear an
NDC number that is false and misleading in that the drugs are manufactured by your firm but the NDC
numbers present on the label are those that identify other firms (21 CFR 207.35). For example, the NDC
number used on your drug product, Dexamethasone Acetate, is the NDC number assigned to [redacted]
Section 501 (a)(2)(B)
The drug products are adulterated within the meaning of section 501(a)(2)(B) in that the controls and
procedures used in their manufacture, processing, packing, and holding do not conform to current good
manufacturing practice regulations, 21 CFR, Parts 210 and 211. Deviations from these regulations include,
but are not limited to, the following:
1. Failure to establish a stability testing program that demonstrates that all products are stable and will retain
their identity, strength, quality, and purity they purport at the end of 1 year and 2 year expiry assigned to the
drug products (21 CFR 211.137 and 211.166).
2. Failure to establish complete master production and control records to ensure drug product uniformity
from batch to batch (21 CFR211.186).
3. Failure to establish complete batch production and control records for each batch of drug products (21
CFR 211.188 (b) (1l)). For example, batch production records lack identification of the person supervising or
checking each step in the manufacturing of a drug.
4. Failure to establish written procedures to assure that correct labels, labeling, and packaging materials are
used for drug products (21 CFR 211.130).
5. Failure to validate the Pressure Vessel Cleaning system (21 CFR 211.67).
In addition, based upon the documentation that you have supplied to FDA to date, there is no evidence that
you have established:
(a) adequate written procedures for production and process control designed to assure that the drug
products have the identity, strength, quality, and purity they purport or are represented to possess (21 CFR
211.100); and
(b) validation procedures and data to support the adequacy of sterilization of the drug products purporting to
be sterile (21 CFR 211.113 (b)). For example, there is no documentation of equipment qualification or
validation of sterilization processes; and
(c) adequate control over design and construction features for the manufacturing facility (21 CFR 211.42).
For example, there is no documentation of the validation of the air handling system or the water system
used in production.
We acknowledge receipt of your September 27, 2000, letter responding to the form FDA- 483, Inspectional
Observations. As noted above, your firm must comply with current good manufacturing practice regulations
for those drug products that your firm manufactures. You also indicate in your letter your plan to restructure
your operations and to ship compounded drugs directly to physicians, without the use of third party
distributors. Your plan does not appear to comply with sections 503A(a)(2)(A) and 503A(a)(2)(B) of the Act
because: (1) from the nature and scope of your firm?s operations, it does not appear that it would involve
preparing limited quantities of compounded drug products before receipt of valid prescription orders for
identified individual patients (503A(a)(2)(A)); and (2) such preparation of compounded drug products before
the receipt of valid prescription orders for individual patients, would not appear to be based on a history of
receiving valid prescription orders for compounded drug products where such orders have been generated
solely within established relationships between the pharmacist-physician-patient as contemplated by section
503A(a)(2)(B).
We note that some of the products prepared by your firm may have reportedly been in short supply for brief
periods of time. However, the large quantities of products prepared by your firm exceed the limited quantities
that may be needed to meet temporary inventory shortages. As discussed above, your products are not
being prepared for identified, individual patients based on prescription orders from licensed practitioners
within an established relationship. Instead, they have been distributed to wholesale drug distributors for
further sale to hospitals, pharmacies and physicians, which goes beyond the regular course of selling or
dispensing drugs at retail.
The above violations are not intended to be an all-inclusive list of deficiencies at your facility. It is your
responsibility to assure that all drug products manufactured and processed at Unique Pharmaceuticals, Ltd.,
are in compliance with federal laws and regulations. Failure to promptly correct these violations and prevent
future violations may result in regulatory action, such as seizure and/or injunction, without further notice.
Please notify this office within 15 working days of receipt of this letter of the specific steps you have taken to
correct these violations, including an explanation of each step being taken to prevent the recurrence of the
violations.
In addition to responding to the above violations, you should provide us with the assurance you have that
the bulk drug substance used in the preparation of Dexamethasone Acetate for Injection 8mg/mL is not
derived from cattle born, raised, or slaughtered in countries where bovine spongiform encephalopathy (BSE)
is known to exist.
You should address your reply to this letter to the U. S. Food and Drug Administration, Attention: Jim Lahar,
Compliance Officer, at the above address.
Sincerely,
Michael A. Chappell
Director, Dallas District
WARNING LETTER TO MIDSOUTH COMPOUNDING
PHARMACY FROM THE FDA 2007 FOR MASS
MANUFACTURING COMPOUNDED PRODUCTS
September 28, 2007
WARNING LETTER NO. 2007-NOL-16
FEDERAL EXPRESS
OVERNIGHT DELIVERY
Patrick Willingham, President and CEO
Med-South Pharmacy, Inc., dba Partners In Care
25819 Canal Road
Orange Beach, Alabama 36561
Dear Mr. Willingham:
On December 20-21, 2006, a U.S. Food and Drug Administration (FDA) investigator conducted an
investigation at your facility, located at 206A Oak Mountain Circle, Pelham, Alabama. This investigation was
initiated in response to reports of injuries relating to betamethasone acetate/betamethasone sodium
phosphate multi-dose injectable drug product, made by your firm. Additionally, on February 21-23, and
March 2, 2007, a follow-up inspection was conducted at your firm. During both instances, our investigators
documented serious violations of the Federal Food, Drug, and Cosmetic Act (FDCA).
A. Compounded Drugs Under the FDCA and FDA's Regulatory Approach to Compounding
FDA's position is the FDCA establishes Agency jurisdiction over "new drugs," including compounded drugs.
FDA's view is compounded drugs are "new drugs" within the meaning of 21 United States Code (USC)
321(p), because they are not "generally recognized, among experts . . . as safe and effective" for their
labeled uses . [See Weinberger v. Hynson, Westcott & Dunning, 412 U.S. 609, 619, 629-30 ( 1973)
(explaining the definition of "new drug").] There is substantial judicial authority supporting FDA's position of
which compounded drugs are not exempt from the new drug definition. [See Prof'Is & Patients for
Customized Care v. Shalala, 56 F.3d 592, 593 n.3 (5th Cir. 1995) ("Although the [FDCA] does not expressly
exempt 'pharmacies' or 'compounded drugs' from the new drug . . . provisions, the FDA as a matter of policy
has not historically brought enforcement actions against pharmacies engaged in traditional
compounding."); In the Matter of Establishment Inspection of Wedgewood Village Pharmacy, 270 F. Supp.
2d 525, 543-44 (D.N.J. 2003), aff'd, Wedgewood Village Pharmacy v. United States, 421 F.3d 263, 269 (3d
Cir . 2005) ("The FDCA contains provisions with explicit exemptions from the new drug .. . provisions.
Neither pharmacies nor compounded drugs are expressly exempted.").] FDA maintains because they are
"new drugs" under the FDCA, compounded drugs may not be introduced into interstate commerce without
FDA approval.[1]
The drugs pharmacists' compound are rarely FDA-approved and thus lack an FDA finding of safety and
efficacy. However, FDA has long recognized the important public health function served by traditional
pharmacy compounding. FDA regards traditional compounding as the extemporaneous combining, mixing,
or altering of ingredients by a pharmacist in response to a physician's prescription to create a medication
tailored to the specialized needs of an individual patient. [See Thompson v. Western States Medical
Center, 535 U.S. 357, 360-61 (2002).] Traditional compounding typically is used to prepare medications
which are not available commercially, such as a drug for a patient who is allergic to an ingredient in a massproduced drug, or diluted dosages for children.
Through the exercise of enforcement discretion, FDA historically has not taken enforcement actions against
pharmacies engaged in traditional pharmacy compounding. Rather, FDA has directed its enforcement
resources against establishments whose activities raise the kinds of concerns normally associated with a
drug manufacturer and whose compounding practices result in significant violations of the new drug,
adulteration, or misbranding provisions of the FDCA.
FDA's current enforcement policy, with respect to the compounding of human drugs, is articulated in
Compliance Policy Guide (CPG) Section 460.200 ["Pharmacy Compounding"], issued by FDA on May 29,
2002 [See Notice of Availability, 67 Fed. Reg. 39,409 (June 7, 2002)] [2]. The CPG identifies factors FDA
considers in deciding whether to initiate enforcement action with respect to compounding. These factors
help differentiate the traditional practice of pharmacy compounding from the manufacture of unapproved
new drugs . They further address compounding practices which result in significant violations of the new
drug, adulteration, or misbranding provisions of the FDCA. As stated in the CPG,"[t]he . . . list of factors is
not intended to be exhaustive."
B. Factual Background
On December 15, 2006, Consumer Complaint number 39633 was filed with the FDA involving an adverse
event associated with the administration of betamethasone acetate/betamethasone sodium phosphate
6mg/ml injectable suspension made by your firm. The injection was given to the patient by a physician on
December 7, 2006. On December 20-21, 2006, an FDA investigator conducted a follow-up investigation to
the consumer complaint at Partners In Care, Pelham, Alabama. The investigation revealed your firm
received at least 70 complaints associated with the use of betamethasone acetate/betamethasone sodium
phosphate 6mg/ml injectable suspension made by Partners In Care. The complaints included redness, large
swollen areas, bruising at the injection site, rash, fever, and cellulitis, with some patients requiring
intravenous antibiotics. On December 22, 2006, Partners In Care initiated a voluntary recall of two lots
(11272006@13 and 12042006@9) of betamethasone acetate/betamethasone sodium phosphate 6mg/ml for
injection in 10ml multi-dose vials. Your firm later revealed a new formulation had been implemented to
"improve workflow", and an incorrect amount of benzalkonium chloride (BZK), used as a preservative, had
been added to the product. Your master formulation called for [redacted] and your analysis
showed [redacted] per [redacted] times the intended amount) was added to the affected lots.
Your firm produces large volumes of injectable products which are copies or essentially copies of FDAapproved, commercially available products, including, but not limited to:
• betamethasone acetate/betamethasone sodium phosphate 6 mg/ml ([redacted]) and 7 mg/ml ([redacted])
[3];
• methylprednisolone acetate 40 mg/ml ([redacted]) and 80 mg/ml ([redacted]);
• triamcinolone acetonide 40 mg/ml (([redacted]);
• dexamethasone acetate 8 mg/ml ([redacted]);
• testosterone cypionate 200 mg/ml ([redacted]);
• promethazine hydrochloride 50 mg/ml ([redacted]);
• brompheniramine maleate 10 mg/ml ([redacted]);
• sodium carboxymethylcellulose1% ([redacted]);
• triamcinolone diacetate 40 mg/ml ([redacted]);
• medroxyprogesterone 150 mg/ml ([redacted]);
• testosterone cypionate 200 mg/ml ([redacted]); and
• triamcinolone diacetate 40 mg/ml ([redacted])
FDA is seriously concerned about the public health risks associated with the large-scale production of
injectable drugs which are copies or essentially copies of FDA-approved, commercially available products
manufactured by firms not meeting the laws and regulations applicable to drug manufacturing. Your firm's
typical batch sizes for these injectable drug products range from, [redacted] which equates to as many
as[redacted] per batch, with an average of [redacted] batches of sterile injectable drugs manufactured
daily. From January 1 to December 31, 2006, your firm produced a total of [redacted] batches of sterile
injectable drug products yielding approximately [redacted]. The production of this volume of FDA-approved,
commercially available products is inconsistent with traditional pharmacy compounding, which involves
compounding medications not commercially available, based on specific needs of individually identified
patients.
Your firm purports to be a compounding pharmacy, but your firm's operation exceeds the scope of traditional
pharmacy practice. During the inspection, the pharmacist in charge stated approximately [redacted] of all
finished injectable drug products are distributed into interstate commerce. You also utilize a team
of [redacted]sales representatives to obtain "orders" for your injectable drug products from physicians'
offices. The large volume of your firm's injectable drug products which are copies or essentially copies of
FDA-approved, commercially available products, and your firm's dispensing practices for these products
exceed the scope of traditional pharmacy compounding and are akin to a pharmaceutical manufacturer. As
such, the FDA will not exercise enforcement discretion with respect to your firm's production of these drugs.
C. Violations of the FDCA
Unapproved New Drug Products
The injectable products made by your firm are drugs within the meaning of Section 201(g) of the FDCA [21
USC 321(g)]. These products are new drugs as defined by Section 201(p) of the FDCA [21 USC 321(p)],
because they are not generally recognized by qualified experts as safe and effective for their labeled uses.
No approved application pursuant to Section 505 of the FDCA [21 USC 355] is in effect for these products.
Accordingly, their introduction or delivery for introduction into interstate commerce violates Sections 505(a)
and 301(d) of the FDCA [21 USC 355(a) and 331(d)].
Misbranded Drug Products
Your firm's injectable drug products are misbranded under Section 502(f)(1) of the FDCA [21 USC 352(f)(1)]
because their labeling fails to bear adequate directions for use and they are not exempt from this
requirement under Title 21, Code of Federal Regulations, Part 201, Section 115 (21 CFR 201.115).
Your firm's injectable drug products are misbranded under Section 502(o) of the FDCA [21 USC 352(o)]
because they are manufactured in an establishment not duly registered under Section 510 of the FDCA [21
USC 360], an d the articles have not been listed as required by Section 510(j) of the FDCA [21 USC 360(j)].
Your facility is not exempt from registration and drug listing requirements under 21 CFR 207.10 or Section
510(g) of the FDCA [21 USC 360(g)].
Further, your firm's betamethasone acetate/betamethasone sodium phosphate 6mg/ml injectable
suspension product (lot numbers 11272006@13 and 12042006@9) are misbranded within the meaning of
Section 502(j) of the FDCA [21 USC 352(j)] because they are dangerous to health when used in the manner
suggested by their labeling. Specifically, the affected lots contained [redacted] times the concentration of
preservative than what was intended according to your new formulation.
Adulterated Drug Products
Your firm's injectable drug products are adulterated under Section 501(a)(2)(B) of the FDCA [21 USC
351(a)(2)(B)] because the controls and procedures used in the manufacture, processing, packing, and
holding of the drug products do not conform to Current Good Manufacturing Practice (CGMP) regulations
set forth in 21 CFR 210 and 211. On March 2, 2007, our investigator documented significant violations of
CGMP regulations including, but not limited to, the following:
1. Failure to establish and follow written procedures to prevent microbiological contamination of injectable
drug products purporting to be sterile, as required by 21 CFR 211.113(b). Specifically, your firm's
manufacturing process has not been validated for your injectable drug products. In addition, the filters used
to sterilize injectable drug products have not been tested for integrity; smoke studies have not been
conducted in the critical areas; and, particulate matter is not being monitored. The autoclave cycles used to
terminally sterilize injectable suspension drug products have not been validated and there is no verification
of their effectiveness with biological indicators [Reference: Form FDA 483, Observations 3 and 4].
2. Failure to test each batch of injectable drug product purporting to be sterile and/or pyrogen-free to
determine conformance to such requirements, as required by 21 CFR. 211.167(a). Specifically, your firm
tests finished injectable drug products for sterility on a monthly basis only [Reference: Form FDA 483,
Observation 1].
3. Failure to ensure all components and injectable drug product containers and closures are, at all times,
handled and stored in a manner to prevent contamination, as required by 21 CFR 211.80(b). Specifically, on
February 21 and 22, 2007, our investigator documented empty, open, sterilized glass vials, which were
exposed to environmental contamination in your Class 10,000 (ISO 7) room and Class 100,000 (ISO 8) ante
room [Reference: Form FDA 483, Observation 16].
4. Failure to test each batch of injectable drug product to determine conformance to final specifications,
including identity and strength of each active ingredient, before release and distribution, as required by 21
CFR 211.165(a). Specifically, your firm does not conduct product testing on all batches of injectable drug
product prior to release. Currently, your firm conducts testing on the concentration of the active ingredient for
injectable drug products on a monthly basis only [Reference: Form FDA 483, Observation 2].
5. Failure to reject injectable drug product which failed to meet established standards or specifications and
any other relevant quality control criteria, as required by 21 CFR 211.165(f). Specifically, your firm
distributed methylprednisolone acetate 80mg/ml, Lot number 09182006@2 of 1, which failed to meet the
established assay specifications. The lot was distributed without conducting any reprocessing or any other
further action. The concentration of methylprednisolone acetate in this lot was 92.02
mg/ml [redacted] percent of the expected amount) [Reference: Form FDA 483, Observation 5].
6. Failure to establish and follow written procedures for production and process controls to assure your
injectable drug products have the identity, strength, quality, and purity they are purported to have, as
required by 21 CFR 211.100(a) and (b). Specifically, your firm has not established complete written
procedures for the methods used to manufacture injectable drug products. The PCCA-provided "Logged
Formula Worksheets" used by your firm for formulation of the sterile injectable products do not include
complete manufacturing instructions and the instruction to use Sterile Water for Injection is not followed
[Reference: Form FDA 483, Observations 19 and 20].
7. Failure to establish laboratory controls, including scientifically sound and appropriate specifications,
standards, sampling plans and test procedures designed to assure the drug products conform to appropriate
standards of identity, strength, quality and purity, as required by 21 CFR 211 .160(b). Specifically, your firm
has not established written specifications for finished injectable drug products [Reference: Form FDA-483,
Observation 20].
8. Failure to establish a quality control unit which has the responsibility and authority to approve or reject all
components, drug product containers, closures, in-process materials, packaging material, labeling, and drug
products, and the authority to review production records to assure no errors have occurred or, if errors have
occurred, they have been fully investigated, as required by 21 CFR 211.22(a). Specifically, your firm has no
designated quality control unit [Reference: Form FDA 483, Observation 7].
9. Failure to verify the identity of each component of injectable drug product and its conformance with all
appropriate written specifications for purity, strength, and quality, as required by 21 CFR 211.84(d)(2).
Specifically, your firm does not conduct any testing on injectable drug components upon receipt, nor does
your firm obtain a certificate of analysis for each component received [Reference: Form FDA 483,
Observation 18].
10. Failure to conduct and document a thorough investigation of any unexplained discrepancy or failure of a
drug product to meet its specifications or to extend the investigation to other batches which may have been
associated with the particular failure or discrepancy, as required by 21 CFR 211.192. Specifically, your firm
failed to conduct complete root cause investigations for three complaints involving injectable drug products
which could not be drawn into the syringe or discharged from the syringe. The complaints involved:
dexamethasone acetate LA 8 mg/ml, Lot number [redacted] (dated October 23, 2006); triamcinolone
diacetate 40 mg/ml, Lot number [redacted] (dated November 15, 2006); and, methylprednisolone acetate
40 mg/ml, Lot number [redacted] (dated January 27, 2007). In addition, none of the investigations were
extended to other lots of product potentially impacted. [Reference: Form FDA 483, Observation 8].
11. Failure to assure all injectable drug products meet applicable standards of identity, strength, quality, and
purity at the time of use by establishing an expiration date determined by appropriate stability testing, as
required by 21 CFR 211.137(a). Specifically, your firm failed to conduct stability testing on your finished
injectable drug products to support your assigned six-month expiration date [Reference: Form FDA 483,
Observation 25].
12. Failure to establish a written testing program designed to assess the stability of your injectable drug
products, as required by 21 CFR 211.166(a). Specifically, your firm lacked a program for, and failed to
conduct stability testing on, your injectable drug products [Reference: Form FDA 483, Observation 23].
13. Failure to ensure all injectable drug products, set aside and held in unlabeled conditions, are sufficiently
identified to preclude mislabeling, as required by 21 CFR 211.130(b). Specifically, on February 22, 2007, our
investigator documented four trays of unidentified glass vials containing drug products on two different
occasions in the compounding room [Reference: Form FDA 483, Observation 9].
14. Failure to prepare batch production and control records for each batch of drug product containing
complete information relating to the production and control of each batch, including documentation where
each significant step in the manufacturing, processing, packing, or holding of your injectable drug products
was accomplished, as required by 21 CFR 211.188(b). Specifically, mixing and sonicator times, heating
temperatures, and drug product pH prior to filling are not recorded. In addition, batch records for sterile
injectable drug products lack both specific identification, such as lot codes, for the drug product containers
and closures used and specimens of finished product labeling [Reference: Form FDA 483, Observations 15,
19 and 24].
15. Failure to establish written procedures for cleaning and maintenance of equipment used in the
manufacture, processing, packing, or holding of a drug product, as required by 21 CFR 211.67(b).
Specifically, your firm does not have any written cleaning procedures [Reference: Form FDA 483,
Observation 14].
16. Failure to establish written procedures describing in sufficient detail the receipt, identification, storage,
handling, sampling, testing, and approval or rejection of components and drug product containers and
closures, as required by 21 CFR 211.80(a). Specifically, your firm has no written procedures to describe in
detail the receipt, identification, storage, handling, sampling, testing, approval, and rejection of components,
injectable drug product containers, and closures [Reference: Form FDA 483, Observation 17].
17. Failure to routinely calibrate automatic, mechanical, or electronic equipment according to a written
program designed to assure proper equipment performance, as required by 21 CFR 211.68(a). Specifically,
your firm routinely does not calibrate scales, the autoclave, or sonicators used to manufacture injectable
drug products. In addition, your firm does not have any written procedures addressing equipment calibration
[Reference: Form FDA 483, Observation 13].
18. Failure to calibrate instruments at suitable intervals in accordance with an established written program,
as required by 21 CFR 21.160(b)(4). Specifically, your firm routinely does not calibrate pH meters. In
addition, your firm does not have any written procedures addressing instrument calibration [Reference: Form
FDA-483, Observation 13].
19. Failure to establish written procedures describing in sufficient detail the control procedures employed for
the issuance of labeling, as required by 21 CFR 211.125(f). Specifically, your firm does not have any written
procedures describing labeling processes [Reference: Form FDA 483, Observation 21].
20. Failure to retain and store, under conditions consistent with product labeling, reserve samples which are
representative of each lot or batch of finished injectable drug product, as required by 21 CFR 211.170(b).
Specifically, your firm does not maintain finished injectable drug product reserve samples [Reference: Form
FDA 483, Observation 22].
21. Failure to establish a written record of major equipment cleaning, maintenance, and use, as required by
21 CFR 211.182. Specifically, your firm failed to maintain individual equipment logs documenting the date,
time, product, and lot number of each batch of finished injectable drug product processed [Reference: Form
FDA 483, Observation 26].
22. Failure to ensure employees engaged in manufacturing, processing, packing, or holding of a drug
product shall have education, training, including training in CGMPs, and experience, or any combination
thereof, to enable the person to perform the assigned functions. Employees involved in the manufacturing of
your injectable drug products have not been trained in CGMP, as required by 21 CFR 211.25(a) [Reference:
Form FDA 483, Observation 10].
23. Failure to reject components which fail to meet required specifications, as required by 21 CFR 211.84(e).
Specifically, although your formula worksheets require the use of sterile water for injection in your sterile
injectable drug products, your firm uses a component labeled as "Sterile Water for Irrigation USP" and "Not
for Injection" to manufacture these drug products. Your firm does not have documentation certifying each lot
of the component labeled "Sterile Water for Irrigation USP" meets specifications for sterile water for injection
[Reference: Form FDA 483, Observation 6].
24. Failure to calculate actual yields and percentages of theoretical yield at the conclusion of each
appropriate phase of manufacturing, processing, packaging, or holding of your injectable drug products, as
required by 21 CFR 211.103 [Reference: Form FDA 483, Observation 11].
Your firm's injectable drug products are in violation of Section 301(a) of the FDCA [21 USC 331(a)] because
introduction or delivery for introduction into interstate commerce of adulterated or misbranded drug products
is a prohibited act. FDA will not exercise enforcement discretion with regard to these and the other violations
cited in this letter.
It is our understanding, your firm is also compounding non-injectable products which may be copies or
essentially copies of FDA-approved, commercially available products, including, but not limited to,
lorazepam 2 mg/ml solution, progesterone 200 mg capsules, promethazine 25mg suppositories,
promethazine 25 mg capsules, carbidopa/levodopa 25/100 mg suspension, hydromorphone 8mg capsules,
and fentanyl 400 mcg troches. Because these products are copies of FDA-approved, commercially available
products, FDA will not exercise enforcement discretion. For the remaining products, which are essentially
copies of FDA-approved, commercially available products, FDA will not exercise enforcement discretion
unless your firm can demonstrate a patient-specific medical need for the variation, as determined by the
prescribing healthcare provider.
The above deficiencies should not be construed as an all-inclusive list of violations that may exist at your
facility, and they may not be limited to the above-cited drug products. It is your responsibility to ensure your
facility is operating in full compliance with all applicable requirements of the FDCA and the implementing
regulations.
You should take prompt action to correct these violations, and you should establish procedures whereby
such violations do not recur. Failure to do so may result in regulatory action without further notice, including
seizure and/or injunction.
You should notify this office in writing, within 15 working days from receipt of this letter, of the specific steps
you have taken to correct the noted violations, including an explanation of each step taken to prevent
recurrence. You should include in your response documentation, such as procedures or other useful
information, to assist us in evaluating your corrections. If corrective actions cannot be completed within 15
working days, state the reason for the delay and the time within which corrections will be completed. You
can find guidance and information regarding regulations through links at FDA's Internet website
at http://www.fda.gov/oc/industry.
Please address your reply to Rebecca A. Asente, Compliance Officer, at the address above. If you have
questions regarding the contents of this letter, please contact Ms. Asente at (504) 219-8818, extension 104.
Sincerely,
/S/
H. Tyler Thornburg
District Director
New Orleans District
__________________
1. In August 2006, the U.S. District Court for the Western District of Texas issued a ruling in Medical Center
Pharmacy v. Gonzales interpreting, among other things, the application of the "new drug" provisions of the
FDCA to compounded drugs. See Medical Center Pharmacy v . Gonzales, MO-04-CV-130, (W.D. Tex, Aug .
30, 2006). The government has appealed this decisionto the U.S. Court of Appeals for the Fifth Circuit.
Pending resolution of this appeal, FDA is abiding by the district court's decision in the Western District of
Texas and with respect to the plaintiffs covered by the decision.
2. Although Section 503A of the FDCA (21 U.S.C. § 353a) addresses pharmacy compounding, this provision
was invalidated bythe Ninth Circuit's ruling in Western States Medical Center v. Shalala. 238 F.3d 1090 (9th
Cir. 2001), because Section 503A included unconstitutional restrictions on commercial speech and those
restrictions could not be severed from the rest of 503A. In Thompson v. Western States Medical Center, 535
U.S. 357 (2002), the Supreme Court affirmed the Ninth Circuit ruling in which the provisions in question
violated the First Amendment.
3. The parentheses in this and the following entries indicate the number of [redacted] produced in 2006,
according to your records.
Enclosure: Form FDA 483, dated March 2, 2007
cc: [redacted]
Med-South Pharmacy, Inc., dba Partners In Care
206A Oak Mountain Circle
Pelham, Alabama 35124
APPENDIX D
WARNING LETTER
NWE-06-07W
VIA FEDERAL EXPRESS
December 4, 2006
Barry J. Cadden, Director of Pharmacy and Owner
New England Compounding Center
697 Waverly Street
Framingham, MA 01702
Dear Mr. Cadden:
On September 23, 2004, investigators from the U.S. Food and Drug Administration (FDA) and the
Massachusetts Board of Pharmacy inspected your firm, located at 697 Waverly Street, Framingham,
Massachusetts. On January 19, 2005, the inspection was completed. This inspection revealed that your firm
compounds human prescription drugs in various dosage forms and strengths.
We acknowledge the receipt of your October 1, 2004, letter addressed to FDA's New England District Office,
concerning questions presented during the referenced inspection.
FDA's position is that the Federal Food, Drug, and Cosmetic Act (FDCA) establishes agency jurisdiction
over "new drugs," including compounded drugs. FDA's view that compounded drugs are "new drugs" within
the meaning of 21 U.S.C. § 321(p), because they are not "generally recognized, among experts . . . as safe
and effective," is supported by substantial judicial authority. See Weinberger v. Hynson, Westcott &
Dunning, 412 U.S. 609, 619, 629-30 (1973) (explaining the definition of "new drug"); Prof'ls & Patients for
Customized Care v. Shalala, 56 F.3d 592, 593 n.3 (5th Cir. 1995) (the FDCA does not expressly exempt
pharmacies or compounded drugs from its new drug provisions); In the Matter of Establishment Inspection
of: Wedgewood Village Pharmacy, 270 F. Supp. 2d 525, 543-44 (D.N.J. 2003), aff'd, Wedgewood Village
Pharmacy v. United States, 421 F.3d 263, 269 (3d Cir. 2005) ("The FDCA contains provisions with explicit
exemptions from the new drug . . . provisions. Neither pharmacies nor compounded drugs are expressly
exempted."). FDA maintains that, because they are "new drugs" under the FDCA, compounded drugs may
not be introduced into interstate commerce without FDA approval.
The drugs that pharmacists compound are not FDA-approved and lack an FDA finding of safety and
efficacy. However, FDA has long recognized the important public health function served by traditional
pharmacy compounding. FDA regards traditional compounding as the extemporaneous combining, mixing,
or altering of ingredients by a pharmacist in response to a physician's prescription to create a medication
tailored to the specialized needs of an individual patient . See Thompson v. Western States Medical Center,
535 U.S. 357, 360-61 (2002). Traditional compounding typically is used to prepare medications that are not
available commercially, such as a drug for a patient who is allergic to an ingredient in a mass-produced
product, or diluted dosages for children.
Through the exercise of enforcement discretion, FDA historically has not taken enforcement actions against
pharmacies engaged in traditional pharmacy compounding. Rather, FDA has directed its enforcement
resources against establishments whose activities raise the kinds of concerns normally associated with a
drug manufacturer and whose compounding practices result in significant violations of the new drug,
adulteration, or misbranding provisions of the FDCA.
FDA's current enforcement policy with respect to pharmacy compounding is articulated in Compliance Policy
Guide (CPG), section 460.200 ["Pharmacy Compounding"], issued by FDA on May 29, 2002 (see Notice of
Availability, 67 Fed. Reg. 39,409 (June 7, 2002)).1 The CPG identifies factors that the Agency considers in
deciding whether to initiate enforcement action with respect to compounding. These factors help differentiate
the traditional practice of pharmacy compounding from the manufacture of unapproved new drugs. They
further address compounding practices that result in significant violations of the new drug, adulteration, or
misbranding provisions of the FDCA. These factors include considering whether a firm compounds drugs
that are copies or essentially copies of commercially available FDA-approved drug products without an FDA
sanctioned investigational new drug application (IND). The factors in the CPG are not intended to be
exhaustive and other factors may also be appropriate for consideration.
1. Copies of Commercially Available Druo Products;
It has come to our attention that you are compounding trypan blue ophthalmic products. During the
inspection at your firm, you advised an investigator from FDA's New England District Office that the trypan
blue products that your firm compounds are devices. FDA classifies trypan blue products as drugs, not
devices. Further, on December 16, 2004, trypan blue ophthalmic solution was approved by FDA and it is
commercially available. As stated in the CPG, FDA will not exercise its enforcement discretion for the
compounding of copies of commercially available FDA-approved products, including this one.
We have also learned that your firm may be compounding 20% aminolevulinic acid solution (ALA). Please
note that there is a commercially available, FDA-approved aminolevulinic acid solution 20% . Like
compounded trypan blue, FDA regards compounded 20% aminolevulinic acid solution as a copy of
commercially available drug.
Although Section 503A of the FDCA (21 U.S.C. § 353a) addresses pharmacy compounding, this provision
was invalidated by the Supreme Court's ruling in Thompson v. Western States Medical Center, 535 U.S. 357
(2002), that Section 503A included unconstitutional restrictions on commercial speech . And those
restrictions could not be severed from the rest of 503A. In Thompson v. Western States Medical Center, 535
U.S. 357 (20020), the Supreme Court affirmed the Ninth Circuit ruling that the provisions in question violated
the First Amendment.
FDA does not sanction the compounding of copies of FDA-approved, commercially available drugs and the
agency will not exercise its enforcement discretion regarding the trypan blue and ALA products compounded
by your firm.
All products compounded by your firm containing trypan blue or ALA are drugs within the meaning of section
201(g) of the FDCA (21 U.S.C. § 321(g)). These products are misbranded under section 502(f)(1) of the
FDCA (21 U.S.C. § 352(f)(1)) in that their labeling fails to bear adequate directions for their use. They are
not exempt from this requirement under 21 CFR § 201 .115 because they are new drugs within the meaning
of section 201(p) of the FDCA and they lack approved applications filed pursuant to section 505 of the FDCA
(21 U.S.C. § 355).
2. Anesthetic Drug Products
Equally serious, your firm's promotional materials reveal that it offers to compound "Extra Strength Triple
Anesthetic Cream" which contains 20% benzocaine, 6% lidocaine, and 4% tetracaine. Like a manufacturer,
you have developed a standardized anesthetic drug product that you sell under the name "Extra Strength
Triple Anesthetic cream," Further, you generate sales by giving physicians "courtesy prescriptions" (i.e., free
samples). These actions are not consistent with the traditional practice of pharmacy compounding, in which
pharmacists extemporaneously compound reasonable quantities of drugs upon receipt of valid prescriptions
from licensed practitioners to meet the unique medical needs of individual patients.
Moreover, the agency is concerned with the public health risks associated with the compounding of "Extra
Strength Triple Anesthetic Cream." There have been at least two nonfatal reactions and two deaths
attributed to the use of compounded topical local anesthetic creams containing high doses of local
anesthetics. Local anesthetics, like "Extra Strength Triple Anesthetic Cream," may be toxic at high dosages,
and this toxicity can be additive. Further, there is a narrow difference between the optimal therapeutic dose
of these products and the doses at which they become toxic, i.e. they have low therapeutic index.
Adverse events consistent with high systemic exposures to these products include seizures and cardiac
arrhythmias. Specifically, risk of systemic adverse events from tetracaine products includes (1) a systemic
allergic response to p-aminobenzoic acid (PABA) which, at worst, could lead to cardiac arrest; or (2)
excessive systemic absorption following repetitive or extensive application, especially for a 4%a product,
which could ultimately lead to convulsions. Tetracaine is associated with a higher incidence of allergic
reactions than other anesthetics, such as Iidocaine. The risk of systemic toxicity is greatest in small children
and in patients with preexisting heart disease. Factors that may increase systemic exposure are time and
surface area of the exposure, particularly when the area of application is covered by an occlusive dressing.
Benzocaine has an additional toxicity not seen with (idocaine, methemoglobinemia, an acquired decrease in
the oxygen-carrying capacity of the red blood cells. Further, patients with severe hepatic disease are at
greater risk of developing toxic plasma concentrations of local anesthetics because of their inability to
metabolize them.
The Extra Strength Triple Anesthetic Cream compounded by your firm is a drug within the meaning of
section 201(g) of the FDCA (21 U.S.C. § 321(g)). This product is misbranded under section 502(f)(1) of the
FDCA (21 U.S.C. § 352(f)(1)) in that its labeling fails to bear adequate directions for its use. It is not exempt
from this requirement under 21 CFR § 201.115, because it is a new drug within the meaning of section
201(p) of the FDCA that lacks an approved application filed pursuant to section 505 of the FDCA (21 U.S.C.
§ 355).
Depending on its labeling, this product may also violate section 502(a) of the FDCA (21 U.S.C. § 352(a)). A
drug or device is misbranded under section 502(a) if its labeling is false and misleading in any particular
(e.g., if the labeling for your local anesthetic products fails to reveal the consequences that may result from
the use of the product as a local anesthetic).
3. Repackaging;
Additionally, we are in receipt of a complaint alleging that you are repackaging the approved injectable drug,
Avastin, into syringes for subsequent promotion and sale to health professionals . Avastin is unpreserved
and is packaged and labeled in 4 and 16 ml single-use glass vials. The labeled precautions include "discard
any unused portion left in a vial . . . ." Each step in the manufacture and processing of a new drug or
antibiotic, from handling of raw ingredients to final packaging, must be approved by FDA, whether carried
out by the original manufacturer or by some subsequent handler or repacker of the product. Pharmacists are
not exempt from these statutory requirements. Generally, the agency regards mixing, packaging, and other
manipulations of approved drugs by licensed pharmacists, consistent with the approved labeling of the
product, as an approved use of the product if conducted within the practice of pharmacy, i.e., filling
prescriptions for identified patients. However, processing and repacking (including repackaging) of approved
drugs is beyond the practice of pharmacy and is thus subject to the Act's premarket approval requirements.
The agency has an established policy, articulated in Compliance Policy Guide Sec. 446.100, Regulatory
Action Regarding Approved New Drugs and Antibiotic Drug Products Subjected to Additional Processing or
other Manipulations (CPG 7132c.06) (copy enclosed), concerning the manipulation of approved sterile drug
products outside the scope of the FDA-approval. FDA is particularly concerned about the manipulation of
sterile products when a sterile container is opened or otherwise entered to conduct manipulations. The
moment a sterile container is opened and manipulated, a quality standard (sterility) is destroyed and
previous studies supporting the standard are compromised and are no longer valid. We are especially
concerned with the potential microbial contamination associated with splitting Avastin - a single-use,
preservative-free, vial -- into multiple doses. When used intravitreaily, microbes could cause
endophthalmitis, which has a high probability for significant vision loss. The absence of control over storage,
and delays before use after repackaging, only exacerbate these concerns.
Avastin is approved for use in the treatment of colorectal cancers. The text of your alleged promotional
material offers this drug to ophthalmologists . Avastin has no approved indications for use in the eye. As
such, your firm is distributing an unapproved new drug in violation of section 505 of the FDCA. Because the
product lacks adequate labeling for its intended use (see 21 CFR § 201.128) your firm is also distributing a
misbranded drug in violation of section 502(f)(1) of the FDCA (21 U.S.C. § 352(f)(1)). Also, please note that,
under section 301(a) of the FDCA (21 U.S.C. § 331(a)), the introduction or delivery for introduction into
interstate commerce of any drug that is misbranded is prohibited.
Under section 301(d) of the FDCA (21 U.S.C. § 331(d)), the introduction or delivery for introduction into
interstate commerce of a new drug that has not been approved under section 505 is also prohibited.
Further, we have been informed that, although your firm advises physicians that a prescription for an
individually identified patient is necessary to receive compounded drugs, your firm has reportedly also told
physicians' offices that using a staff member's name on the prescription would suffice. Drugs compounded in
this manner are not compounded consistent with the CPG, and FDA will not exercise its enforcement
discretion regarding those drugs.
The above violations are not intended to be an all-inclusive list of deficiencies. You should take prompt
action to correct these deviations. Failure to promptly correct these deviations may result in additional
regulatory action without further notice, including seizure or injunction against you and your firm. Federal
agencies are routinely advised of the issuance of warning letters so that they may take this information into
account when considering the award of government contracts.
Please notify this office in writing within 15 working days of receipt of this letter of any steps that you will take
to correct the noted violations, including an explanation of the steps taken to prevent the recurrence of
similar violatJons. If corrective action cannot be completed within 15 working days, please state the reason
for the delay and the time within which the correction will be complete.
You should address your reply to this letter to the U.S. Food and Drug Administration, New England District
Office, One Montvale Ave., 411 Floor, Stoneham, MA 02180, Attn: Ann Simoneau, Compliance Officer. If
you have any further questions, please feel free to contact Ms. Simoneau at (781) 596-7732.
Sincerely,
/s/
Gail Costello
Disrict Director
New England District Office