R_-_Anti-inflammatory__Immunosuppressive_Rx
advertisement
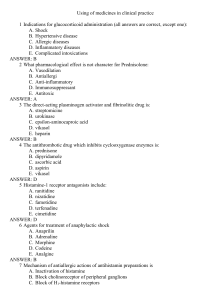
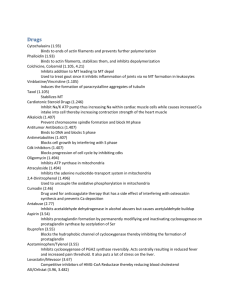
Strategies of Anti-Inflammatory Therapy: Target a single mediator – antihistamines and leukotriene modifiers i. Antihistamines: H1 – inverse agonists / comp antagonists 1. H1 – Old: Diphenhydramine & Chlorpheniramine 2. H1 – New: Cetrizine / Loratadine / Fexofenadine ii. Leukotriene antagonists to CysLTR1 : 1. Zafirlukast 2. Montelukast – better b/c no meal restrictions Target multiple mediators – anti-inflammatory steroids, NSAIDs (shot-gun approach) i. COX pathway 1. Aspirin – irreversibly inhibits COX 2. tNSAIDs – non-selective COX inhibitor a. Ibuprofen – less GI SE than Aspirin b. Naproxen c. Diflunisal d. Ketoprofen e. Indomethacin – MOST POTENT f. Sulindac g. Piroxicam bad GI bleed 3. Selective COX2 inhibitors – Celecoxib 4. Acetominophen – Tylenol – FEVER AND PAIN! Stop mediator production – synthesis inhibitors i. LTs – 5-LO inhibitor: Zileuton Stop mediator release Stop mediator action – antagonists or inverse agonists i. Kinin receptor antagonist: Icatibant – for C1 inhibitor def Cortisol is an anti-inflammatory! Synthetic steroids: bethamethasone, dexamethasone, methylprednisone, predinisone Calcineurin inibs – post organ transplant – both block DEPHOSPHORYLATION needed for cytokine GENE EXPRESSION & T cell activation o Cyclosporine to cyclphilin o Tacroliums to FKBP Antiproliverative/antimetabolic drugs o Sirolimus: INHIBITS ENZYME NEEDED FOR CELL PROLIFERATION of T cell. – cell cycle o M. mofetil: INHIBITS IMPDH needed for de novo guanine synthesis o Other anticancer drugs: azatioprine, methotrexate, cyclophosphamide Abs: o Muromonab-CD3 – blocks CD3 on TCR o Daclizumab or Basiliximab bind to IL-2 receptor Anti-inflammatory & Immunosuppressive Drugs (Regal) INFLAMMATION overview: (1) Inflammation is a process: Sublethal injury Mediators Inflammation (redness, swelling, heat, pain) Injury d/t: heat, mechanical, chemical, bacteria, virus, Ab-Ag reactions Mediators: endogenous substances (autacoids/local hormones) that are stored or rapidly synthesized, intended to act only at the site of injury. Lots of redundancy! Fever Pain (either causes pain or reduces pain threshold) PGEs (2) (3) Redness & heat (vasodilation) Swelling ( permeability) PGE₂ Histamine PGE₂ Histamine Peptidoleukotrienes (LTC₄, LTD₄, LTE₄) PGI₂ - prostacyclin PGI₂ - prostacyclin Kinins Kinins Kinins Chemotaxis Peptidoleukotrienes (eosinohpils) LTB₄ (neutrophils) Airway constriction Hypotension Histamine Peptidoleukotrienes (LTC₄, LTD₄, LTE₄) PGD₂ Histamine Kinins Kinins Acute inflammation review: Changes in blood vessel caliber & flow : arteriolar dilation, increased blood flow, slowing of flow to stasis. This causes redness & heat. Increased vascular permeability : post capillary venules leak large molecules, contraction of endothelium w/ spaces in bxt. This causes swelling which can lead to pain. Leukocytic infiltration : post capillary venules, pavementing of leukocytes, mvmt into extravascular space, chemotaxis Mediators that will cause all this to occur: Histamine, Prostaglandins, Leukotrienes, Platelet Activating Factor (PAF), kinins, products of complement system activation, cytokines, chemokines, interleukins, adhesion molecules. i. Mediators in any given situation will differ depending on: nature and extent of injury, location of injury, type of Ag-Ab rxn Airway constriction (bronchoconstriction) is relevant in asthma (immune mediated lung disease) Hypotension is relevant in shock (systemic release of inflammatory mediators). Can be d/t widespread vasodilation, increased capillary permeability & fluid loss from circulation! Strategies of Anti-Inflammatory Therapy: Target a single mediator – antihistamines and leukotriene modifiers Target multiple mediators – anti-inflammatory steroids, NSAIDs (shot-gun approach) Stop mediator production – synthesis inhibitors Stop mediator release Stop mediator action – antagonists or inverse agonists IMMUNOSUPPRESSION: (1) (2) (3) Immunosuppressive drugs are used to dampen the immune system in organ transplantation, autoimmune disease & hypersensitivity. Works best on primary immune response. Will work better if therapy starts before exposure to immunogen. Want to do this so you don’t get immune mediated tissue damage which thereby means you don’t have an inflammatory response related to the tissue damage. Limitations include: risk of all infections and lymphomas & related malignancies Major classes of immunosuppressive drugs: Glucocoriticoids = Anti-inflammatory steroids. Made by adrenal cortex. Cortisol turns off immune system as a negative feedback inhibitor = natural anti-inflammatory system. i. Corticosteroids (21C) are released in response to stimulation by ACTH. 1. Mineralocorticoids (electrolyte balance) 2. Glucocotriocoids (carbohydrate metabolism) Activity: Prototype Compound Sodium Retention (can the steroid Na excretion by kidney?) Mineralocorticoids Glucocorticoids Aldosterone Cortisol + - Liver Glycogen Deposition (can the steroid cause hepatic deposition of glycogen?) + Anti-Inflammatory + ii. Androgens (19C) 1. NOT body building iii. Why do we use anti-inflammatory steroid drugs?? When immune system is too active, the addition of exogenous glucocorticoids can turn it off (endogenous ones are doing their job). Want to minimize drug action on the mineralocorticoid receptor. 1. Synthetic steroids: Betamethasone, Dexamethasone, Methylprednisone, Prednisone 2. Oral, parenteral & topical administration. Some systemic absorption always occurs. Metabolized by liver & excreted by kidney. 3. Inhaled glucocorticoids are designed for uptake & prolonged tissue binding in airway. 4. How do steroids work?? Time lag in steroid action. There are a number of protein products responsible for immunosuppressive effects. Steroid GR complex interacts w/ TFs which can repress gene expression. iv. Effects of glucocorticoids on ppl: 1. Effects on cell mvmt a. Neutrophils – more of them, release from BM , in circulation longer, blockage of migration to inflammatory sites by adherence b. Lymphocytes – lymphopenia, cells not lysed, but move to extravascular compartments c. Monocytes & eosinohpils are decreased in peripheral blood 2. Effects on synthesis &/or release of inflammatory mediators a. Reduced expression of COX2 b. Inhibits release of arachidonic acid from PLs = PG & LT production c. Inhibits degranulation of mast cells and basophils d. Inhibits synthesis & release of TNF, IL1, IL2 and IFN v. Therapy: 1. W/ systemic admin SE can be life threatening 2. Cortisol & analogs prevent / suppress R, S, H P…but underlying cause of disease remains 3. Lowers host resistance to microbial and fungal infection. vi. Therapeutic principles: 1. Dosing often by trial & error 2. Single dose OK; a few days OK as long as not high dose…prolonged = BAD! a. also…don’t just take someone off a long dose, need to TAPER vii. Uses: 1. Arthritis 2. Rheumatic carditis 3. Renal diseases - SLE nephrotic syndrome 4. Collagen diseases - systemic lupus 5. Allergic diseases - not acute anaphylaxis 6. Bronchial asthma - inhalation, systemically 7. Ocular diseases - in bacterial, fungal or viral infection, glucocorticoids can mask the progression of the disease 8. Skin diseases – eczema 9. Diseases of the intestinal tract - chronic ulcerative colitis 10. Malignancies 11. Diseases of the liver 12. Shock - use is controversial Calcinerin inhibitors – in immunosuppression after organ transplantation i. Cyclosporine: binds to cytoplasmic receptor protein called cyclophilin inhibiting caclineurin activity. Blocks dephosphorylation events needed for cytokine gene expression & T cell activation. 1. Met in liver 2. Lots of drug interactions 3. Long term tx for transplantation 4. Renal toxicity – BAD SE ii. Tacrolimus (FK506): binds to cytoplasmic receptor called FKBP inhibition of calcineurin. Blocks same stuff 1. 100 times more potent than cyclosporine 2. Toxicity similar nephrotoxicity Antiproliferative/antimetabolic drugs – prevent clonal expansion of both B & T cells i. Sirolimus (rapamycin): binds to FKBP to inhibit enzyme needed for cell cycle proliferation – blocks G1 S in IL driven T cell proliferation. 1. Toxicity: WORSE than Aspirin! ii. Mycophenolate mofetil: a metabolite is an inhibitor of inosine monophosphate dehydrogenase (IMPDH), an imp enzyme in the de novo pathway of guanine nt syn. B & T cells are highly dependent on de novo synthesis of purines for cell proliferation, while other cells can use salvage pathways. iii. Other anticancer drugs like azathioprine, methotrexate & cyclophosphamide 1. Immune cells prolif in response to a specific Ag, Ca cells just go nuts. Low doses block immunoproliferation & high dose will kill cancer cells. DOSING Antibodies i. Eliminate lymphocytes 1. Anti-thymocyte globulin: purified Igs. Will bind to thymocytes in circulation lymphopenia & impaired T cell immune response a. Toxicity: Ig being seen as foreign serum sickness & nephritis ii. Affect T cell function 1. Muromonab-CD3 (for kidney, liver and heart transplants) a. Ab binds to CD3, TCR can’t work. Can cause cytokine release syndrome: i. Flu-like sx life-threatening shock. Crosslinking = cytokine release 2. Daclizumab or Basiliximab (organ transplantation) a. Mouse Ab to IL-2 receptor b. Bind to IL-2 receptor on activated but not resting T cells and block IL-2 mediated T cell activation c. Anaphylaxis can occur. No cytokine release syndrome Site of Action of Selected Immunosuppressive Agents on T Cell Activation DRUG SITE OF ACTION Glucocorticoids Glucocorticoid response elements in DNA (regulate gene transcription) Cyclosporine Calcineurin (inhibits phosphatase activity) Tacrolimus Calcineurin (inhibits phosphatase activity) Sirolimus Protein kinase involved in cell-cycle progression (mTOR) (inhibits activity) Mycophenolate mofetil Inosine monophosphate dehydrogenase (inhibits activity) Muromonab-CD3 (Ab) T-cell receptor complex (blocks antigen recognition) Daclizumab, Basiliximab (Ab) IL-2 receptor (block IL-2-mediated T-cell activation)


![Shark Electrosense: physiology and circuit model []](http://s2.studylib.net/store/data/005306781_1-34d5e86294a52e9275a69716495e2e51-300x300.png)