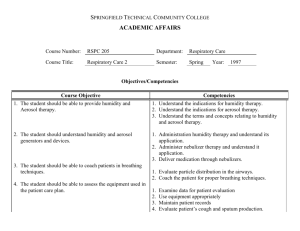
Intermittent Positive Pressure Breathing (IPPB)
advertisement
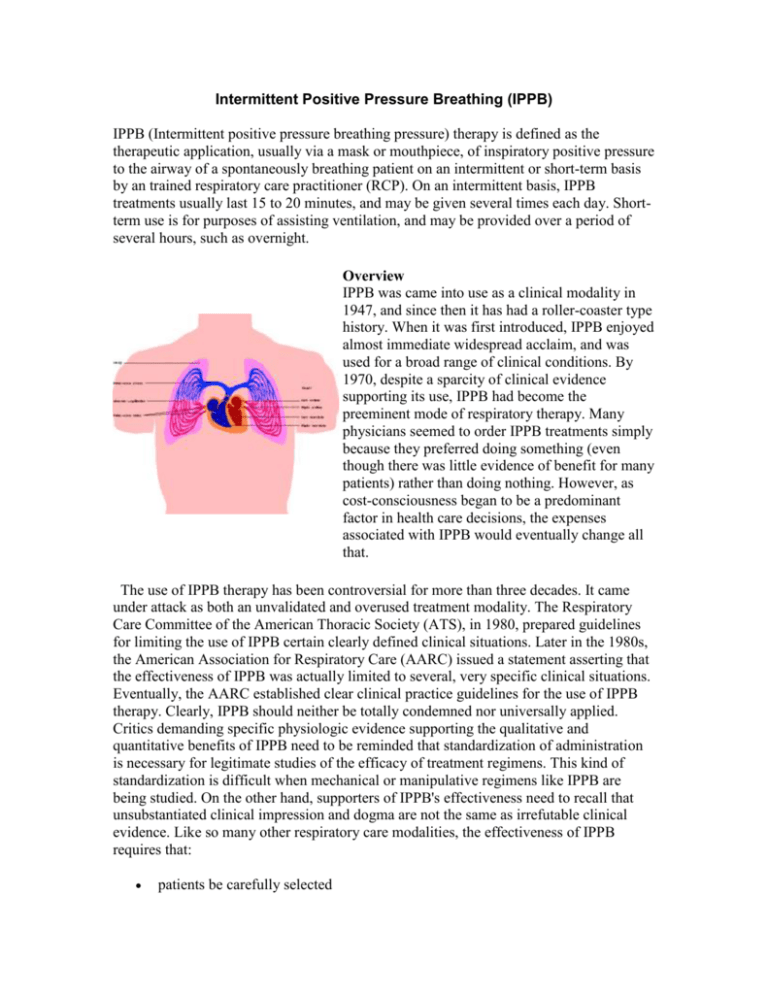
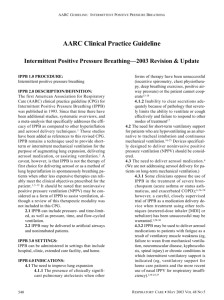
Intermittent Positive Pressure Breathing (IPPB) IPPB (Intermittent positive pressure breathing pressure) therapy is defined as the therapeutic application, usually via a mask or mouthpiece, of inspiratory positive pressure to the airway of a spontaneously breathing patient on an intermittent or short-term basis by an trained respiratory care practitioner (RCP). On an intermittent basis, IPPB treatments usually last 15 to 20 minutes, and may be given several times each day. Shortterm use is for purposes of assisting ventilation, and may be provided over a period of several hours, such as overnight. Overview IPPB was came into use as a clinical modality in 1947, and since then it has had a roller-coaster type history. When it was first introduced, IPPB enjoyed almost immediate widespread acclaim, and was used for a broad range of clinical conditions. By 1970, despite a sparcity of clinical evidence supporting its use, IPPB had become the preeminent mode of respiratory therapy. Many physicians seemed to order IPPB treatments simply because they preferred doing something (even though there was little evidence of benefit for many patients) rather than doing nothing. However, as cost-consciousness began to be a predominant factor in health care decisions, the expenses associated with IPPB would eventually change all that. The use of IPPB therapy has been controversial for more than three decades. It came under attack as both an unvalidated and overused treatment modality. The Respiratory Care Committee of the American Thoracic Society (ATS), in 1980, prepared guidelines for limiting the use of IPPB certain clearly defined clinical situations. Later in the 1980s, the American Association for Respiratory Care (AARC) issued a statement asserting that the effectiveness of IPPB was actually limited to several, very specific clinical situations. Eventually, the AARC established clear clinical practice guidelines for the use of IPPB therapy. Clearly, IPPB should neither be totally condemned nor universally applied. Critics demanding specific physiologic evidence supporting the qualitative and quantitative benefits of IPPB need to be reminded that standardization of administration is necessary for legitimate studies of the efficacy of treatment regimens. This kind of standardization is difficult when mechanical or manipulative regimens like IPPB are being studied. On the other hand, supporters of IPPB's effectiveness need to recall that unsubstantiated clinical impression and dogma are not the same as irrefutable clinical evidence. Like so many other respiratory care modalities, the effectiveness of IPPB requires that: patients be carefully selected the indications for therapy be specifically defined the goals of therapy be clearly understood the treatment be properly administered by a trained RCP The key to being able to accurately assess a treatment modality's efficacy is to evaluate how well it accomplishes its goals, and to review the goals of IPPB it is necessary to first understand the physiological basis and impact of IPPB. Physiologic Principles If IPPB is to be successful, it must increase alveolar distending pressure. This is accomplished by increasing alveolar pressure so that the difference between alveolar and pleural pressure also is increased. IPPB reverses the normal spontaneous pressure gradients. Instead of negative alveolar pressure causing gas flow into the lungs, positive pressure at the airway opening creates the needed gradient. The rise in alveolar pressure increases PL and expands the alveoli. When alveolar distending pressures are increased, a large volume of gas exists within the airway. Gas flows from the airway into the lungs, and alveolar pressures rise during the inspiratory phase of IPPB. As a result of these pressure changes, four physiologic effects can be attributed to IPPB: An increase in mean airway pressure A decrease in the work of breathing (WOB) Manipulation of the inspiratory-expiratory ratio Increase in tidal volume (VT) Appropriate application of IPPB may result in a stressed patient accepting and being comfortable with ventilatory patterns they could not tolerate during spontaneous breathing. When an increased WOB exists, intermittent positive pressure may allow the same degree of physiologic ventilation with far less expenditure of muscular energy. Examples Description Bird Mark - 7 Pneumatically powered assist/controller pressure ventilator for delivery of IPPB therapy. Requires gas source of 50 pounds per square inch. Bird Mark - 8 Same features as Mark-7 plus adjustable expiratory flow rate providing positive (PEEP)/negative (NEEP) end expiratory pressure. Bird Mark - 10 Leak compensating IPPB ventilator with Mark-7 features. Bird Mark - 14 Leak compensating IPPB ventilator with Mark-7 features plus extended range of flow and pressure. Electrically powered IPPB with AP-5 features plus cover Puritan Bennett APand handle modifications for storage and transport. 4 Convenient for homecare or hospital use. Puritan Bennett AP- Electrically powered IPPB therapy unit with internal 5 motor/compressor. Ideal for homecare or hospital use.