Case study IPPB part I indications
advertisement
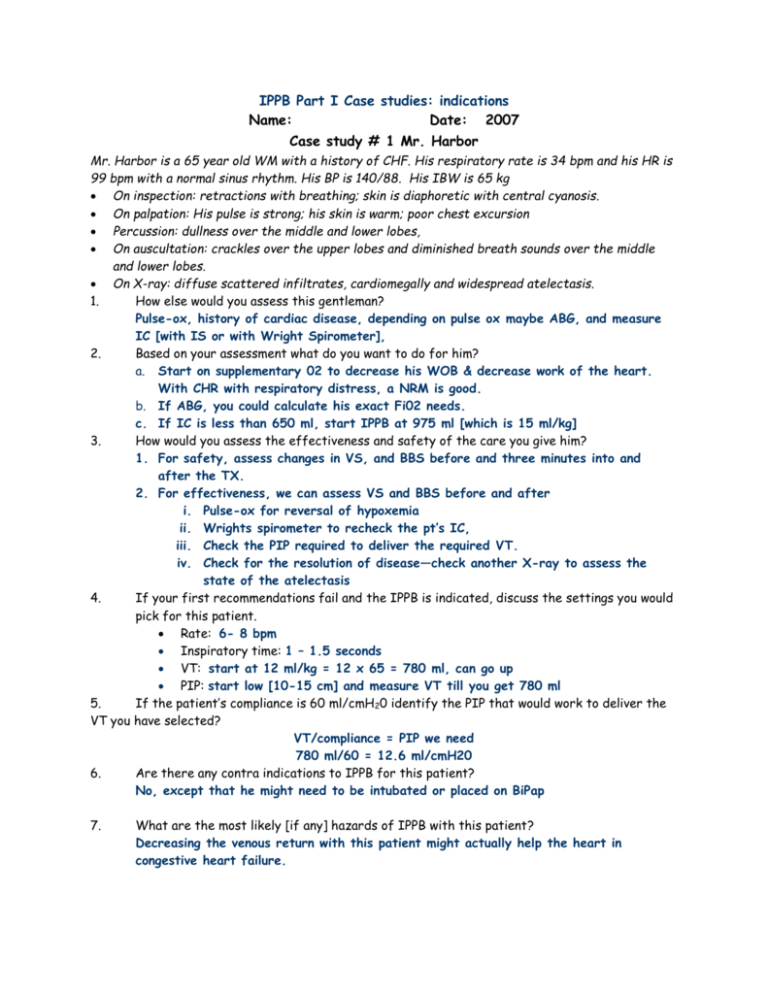
IPPB Part I Case studies: indications Name: Date: 2007 Case study # 1 Mr. Harbor Mr. Harbor is a 65 year old WM with a history of CHF. His respiratory rate is 34 bpm and his HR is 99 bpm with a normal sinus rhythm. His BP is 140/88. His IBW is 65 kg On inspection: retractions with breathing; skin is diaphoretic with central cyanosis. On palpation: His pulse is strong; his skin is warm; poor chest excursion Percussion: dullness over the middle and lower lobes, On auscultation: crackles over the upper lobes and diminished breath sounds over the middle and lower lobes. On X-ray: diffuse scattered infiltrates, cardiomegally and widespread atelectasis. 1. How else would you assess this gentleman? Pulse-ox, history of cardiac disease, depending on pulse ox maybe ABG, and measure IC [with IS or with Wright Spirometer], 2. Based on your assessment what do you want to do for him? a. Start on supplementary 02 to decrease his WOB & decrease work of the heart. With CHR with respiratory distress, a NRM is good. b. If ABG, you could calculate his exact Fi02 needs. c. If IC is less than 650 ml, start IPPB at 975 ml [which is 15 ml/kg] 3. How would you assess the effectiveness and safety of the care you give him? 1. For safety, assess changes in VS, and BBS before and three minutes into and after the TX. 2. For effectiveness, we can assess VS and BBS before and after i. Pulse-ox for reversal of hypoxemia ii. Wrights spirometer to recheck the pt’s IC, iii. Check the PIP required to deliver the required VT. iv. Check for the resolution of disease—check another X-ray to assess the state of the atelectasis 4. If your first recommendations fail and the IPPB is indicated, discuss the settings you would pick for this patient. Rate: 6- 8 bpm Inspiratory time: 1 – 1.5 seconds VT: start at 12 ml/kg = 12 x 65 = 780 ml, can go up PIP: start low [10-15 cm] and measure VT till you get 780 ml 5. If the patient’s compliance is 60 ml/cmH20 identify the PIP that would work to deliver the VT you have selected? VT/compliance = PIP we need 780 ml/60 = 12.6 ml/cmH20 6. Are there any contra indications to IPPB for this patient? No, except that he might need to be intubated or placed on BiPap 7. What are the most likely [if any] hazards of IPPB with this patient? Decreasing the venous return with this patient might actually help the heart in congestive heart failure. 8. If the IPPB is successful what do you expect: to see on inspection immediately after the treatment? Decreased WOB, improved VS, better colour. Less sweating and working so hard To hear on auscultation immediately after the treatment? BBS should have decreased crackles, increased air movement into the lower lobes To see on the X-ray about 24-48 hours later? Atelectasis resolving, better air movement into the lower lobes Case study # 2 Miss. Barter Miss Barter is a 35 year old BF with a history of asthma. Her respiratory rate is 34 bpm and her HR is 100 bpm with a normal sinus rhythm. Her BP is 128/76. IBW is 58 kg. Her Sp02 is 93% on 4 lpm nasal cannula. On inspection: increased AP diameter, use of accessory muscles of inspiration and of exhalation; her skin is diaphoretic with central cyanosis. On palpation: Her pulse is shows pulsus paradoxes & warm damp skin On percussion: hyper resonance over the upper lobes, On auscultation: diffuse inspiratory and expiratory wheezes, prolonged exhalation On X-ray: RML atelectasis with wide-spread signs of air trapping 1. How would you assess this lady? VS, pulse ox, because history + for asthma, PEFR for bronchospasm and possible IC for IPPB, ABG to assess her C02, because if her C02 rises she might need to be ventilated 2. Based on your assessment what do you want to do for her? a. Give supplementary 02 to get Sp02 above 95% b. Try SVN with albuterol 2.5 mg & atrovent with saline c. Start steroids iv or inhaled d. If IC was lower than 10 ml /cmH20 – 580 ml less we need to consider IPPB with the beta II 3. How would you assess the effectiveness and safety of the care you give her? To assess the effectives of TX, we assess the VS & BBS and pulse ox To assess the safety of the TX, we assess the VS, BBS and pulse ox 4. If the doctor decides to order IPPB, are there any absolute contraindications for this patient? Wheezing can cause air-trapping; give IPPB with a Beta II 5. If the doctor decides to order IPPB, identify any adverse hazards that this patient is at particular risk for getting? Air trapping and barotrauma such as pneumothorax 6. Identify the VT you would pick for this patient. 12 ml/Kg = 12 x 58 = 696 ml VT 7. do? If the patient started breathing at a rate of 20 bpm on the IPPB, what would you have to Get him to breath off the IPPB, then every 8-10 seconds take an IPPB breath. 6- 8 bpm on IPPB 8. Explain your answer. We want a SMI, so we need slow deep breaths with inspiratory holds. He doesn’t need to breath so fast because we will decrease venous return to the heart and we can blow off the C02 so he will get dizzy from hyperventilation Case study # 3 Mr. Reed Mr. Reed is a 19 year old WM with a history of a neuromuscular disorder. His respiratory rate is 33 bpm and his HR is 105 bpm with a normal sinus rhythm. His BP is 118/69. His IBW is 65 kg On inspection: paradoxical breathing, sweaty and central cyanosis. On palpation: His pulse is strong; with his skin is hot. You note poor chest excursion, particularly over the lower part of his chest wall Percussion: you note dullness over the middle and lower lobes, On auscultation: you hear crackles over the upper lobes, rhonchi and diminished breath sounds over the middle and lower lobes. On X-ray: low volume lung; diffuse scattered infiltrates, and widespread atelectasis in the LLL and the RML. 1. How would you assess this gentleman? Pulse ox, history of recent and old history, ABG to r/o chronic hypercapnia IC to r/o decreased ability to deep breathe and cough effectively. Sputum production 2. Based on your assessment what do you want to do for him? IPPB if the IC is less than 10 ml/kg--- less 650 ml –assess his cough with IPPB and if he needs help suction Low flow [1-2 lpm nasal cannula] 02 to get Sp02 above 90% keep at 92% is reasonable 2.5 mg Albuterol and normal saline with IPPB 3. How would you assess the effectiveness and safety of the care you give him? For effectiveness of IPPB: Monitor IC after IPPB, x-ray after IPPB, monitor his ability to cough, & his sputum production, For safety, VS [monitor BP if HR rises] BS, Sp02, monitor VT on IPPB 4. 5. 6. 7. If the doctor orders IPPB, what setting do you pick? Rate: 6-8 bpm Inspiratory time: 1 – 1.5 seconds VT: 12 ml/kg = 12 x 65 = 780ml VT If this patient’s lung compliance is 55 ml/cmH20, what PIP might you need to start with? VT/compliance = pressure needed 780 ml/55 ml/cm = 14.18 cm PIP needed Are there any contra indications to IPPB for this patient? None that I can see What are the most likely [if any] hazards of IPPB with this patient? 1. Persons with neuromuscular problems or quadriplegic are at increased risk of hypotension, watch the IPPB rate so that his venous return is not affected. 2. There is a good chance that this patient might have chronic hypercapnia- give his IPPB with compressed air so we don’t trigger 02 induced apnea Case study # 4 Mrs. Rojas Mrs. Rojas is a 45 year old LAF with a history of acute bacterial pneumonia. Her respiratory rate is 30 bpm and her HR is 115 bpm with a normal sinus rhythm. Her BP is 128/76. IBW 48 kg On inspection: you see someone who is breathing is rapid & shallow, with retractions ; central cyanosis. On palpation: Her pulse is rapid and thready; her skin is hot and diaphoretic poor chest excursion On percussion: you note hyper-resonance over the upper lobes, and dullness over the lower lobes, On auscultation: you hear diffuse rhonchi, inspiratory and expiratory wheezes and crackles over the RML. The lower lobes are distant On X-ray you see: atelectasis in the bilateral lower lobes and in the RML. 1. How would you assess this lady? Pulse ox , recent history, IC VS, PEFR 2. Based on your assessment what do you want to do for her? 1. Give supplementary 02 to get Sp02 above 92% 2. Beta II drug- SVN if IC is above 10 ml/kg 3. If IC is below 10 then IPPB 4. Broad spectrum Antibiotic after culture sensitivity of sputum 3. How would you assess the effectiveness and safety of the care you give her? Assessment of effectiveness: VS, X-ray, sputum, pulse ox, IC and PEFR, BS Assessment of safety: VS, If IPPB VS, return Vt. Pt’s subjective response to IPPB 4. If the doctor orders IPPB, what setting do you pick? Rate: 6-8 bpm Inspiratory time: 1 – 1.5 seconds VT: 12 ml/kg = 12 x 48 = 576 ml VT 5. If you started IPPB with PIP of 15 and you measured a VT of 300ml, what would you have to do to give the proscribed VT? Compliance is the ΔV/ ΔP = 300/15 = 20 ml/cmH20 We need 576 ml VT so VT/compliance = PIP 576/20 = 28.8 cmH20 Usually increasing the PIP to 24 and above can increase chances of swallowing air, and we worry about barotrauma at such high pressures, so we would limit this to about 18 -20 6. What effect would the IPPB breath have on the gas distribution into her lungs? During IPPB, the gas flow will move toward the distal basal areas of the lung that have atelectasis because of the pressure gradient between those alveoli and the airway 7. Are there any contraindications for IPPB for this lady? IPPB with saline is contraindicated, we must use a Beta II This patient is at high risk of barotrauma, air trapping and pneumothorax. I really would not want to suggest IPPB, she might need to be intubated for respiratory failure rather than IPPB 8. If you lack enough information to make a decision, what extra data might you need? We need serial ABG to watch the progression of her PaCo2