G:\respcare\IPPB_ lect_ part i
advertisement
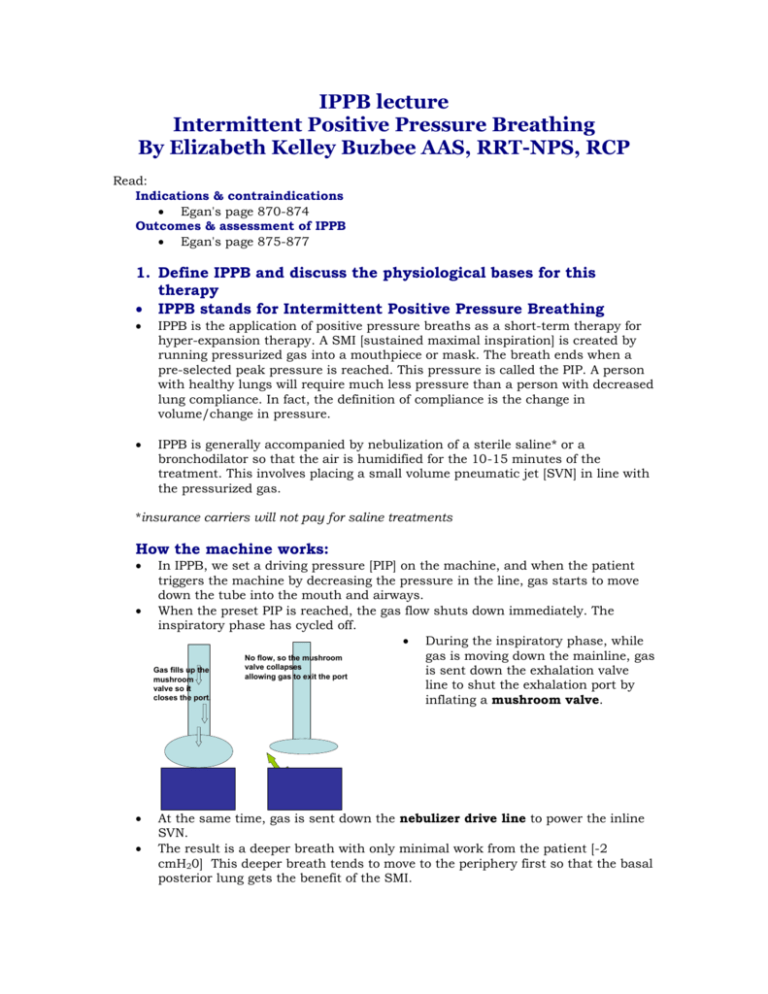
IPPB lecture Intermittent Positive Pressure Breathing By Elizabeth Kelley Buzbee AAS, RRT-NPS, RCP Read: Indications & contraindications Egan's page 870-874 Outcomes & assessment of IPPB Egan's page 875-877 1. Define IPPB and discuss the physiological bases for this therapy IPPB stands for Intermittent Positive Pressure Breathing IPPB is the application of positive pressure breaths as a short-term therapy for hyper-expansion therapy. A SMI [sustained maximal inspiration] is created by running pressurized gas into a mouthpiece or mask. The breath ends when a pre-selected peak pressure is reached. This pressure is called the PIP. A person with healthy lungs will require much less pressure than a person with decreased lung compliance. In fact, the definition of compliance is the change in volume/change in pressure. IPPB is generally accompanied by nebulization of a sterile saline* or a bronchodilator so that the air is humidified for the 10-15 minutes of the treatment. This involves placing a small volume pneumatic jet [SVN] in line with the pressurized gas. *insurance carriers will not pay for saline treatments How the machine works: In IPPB, we set a driving pressure [PIP] on the machine, and when the patient triggers the machine by decreasing the pressure in the line, gas starts to move down the tube into the mouth and airways. When the preset PIP is reached, the gas flow shuts down immediately. The inspiratory phase has cycled off. During the inspiratory phase, while gas is moving down the mainline, gas No flow, so the mushroom valve collapses Gas fills up the is sent down the exhalation valve allowing gas to exit the port mushroom line to shut the exhalation port by valve so it closes the port. inflating a mushroom valve. At the same time, gas is sent down the nebulizer drive line to power the inline SVN. The result is a deeper breath with only minimal work from the patient [-2 cmH20] This deeper breath tends to move to the periphery first so that the basal posterior lung gets the benefit of the SMI. Unfortunately this breath also transmits positive pressure into the thorax. That is responsible for a lot of side effects. In both IPPB and normal breathing exhalation is passive and takes a bit longer. Because this is a SMI, we will limit the respiratory rate of IPPB to 6-8 bpm 2. Discuss the role of normal breathing in the regulation of the blood pressure in the heart and brain. In normal breathing, one creates negative [subatmospheric] intrathoracic pressure by increasing the chest volume. In a normal deep breath, one holds this negative pressure for a longer time so that more air moves down the airway into the lung. Generally, these pressures are tiny. [-5 to –10 cmH20] because the normal lung had good compliance and the driving pressures required to move a volume into the lungs are low [normal lung C =100-150 ml/cmH20]. A normal –5 creates a driving pressure of 5 cmH20 that moves about 500-750 ml Vt. When one breathes normally, there is negative pressure created in the thorax. This suction helps suck blood back into the right side of the heart. Just as coughing or sneezing will decrease this venous return, IPPB with its high thoracic pressures will hamper venous return to the right side of the heart. Just as with a cough, blood from the head will back up due to these positive pressures. If there is high pressure in the head, this pressure will only increase 3. List the indications for IPPB. Clinically diagnosed atelectasis not responsive to other therapies [cough deep breath, and IS] Inability to clear airways due to inability to take deep breaths Short-term none-invasive ventilatory support for hypercapnic patients [IPPB has been replaced by BiPap these days—but if you don't have a BiPap machine handy, it still works] Delivery of aerosolized drugs when SVN has failed Delivery of aerosolized drugs when patient cannot take a deep breath [less than 10 ml/cmH20] 4. List the goals of IPPB: Improve the Vt by 25%--- which should increase the IC [hopefully the patient's respiratory rate returns to normal after the treatment] Increased PEFR & FEV1 [assuming patient got a Beta II bronchodilator with IPPB Improve cough by accomplishing the first two Improve chest film. Reduce atelectasis Improve breath sounds: increased BBS in the basal areas Improve oxygenation: check pulse oximeter before and after TX Favorable patient response. [subjective] 5. List & discuss the contraindications for IPPB: Tension pneumothorax. Any untreated pneumothorax can become a tension pneumothorax as positive pressure pushes more air into the chest wall from the airway. Conditions that predispose a patient to pneumothorax Air trapping/ asthma, COPD, emphysema Excessive pressure set on the control which will deliver excessive Vt. [max 45 mL/kg IBW] Please note, setting the Vt at 15 ml/kg should be enough to increase the IC so that the patient can cough. ICP over 15 mmHg. High intercranial pressure can be made worse by positive pressure in the chest that will hamper drainage from blood from the head. Hemodynamically instability. Because the positive pressure in the chest hampers return of venous blood to the heart, it will decrease the stroke volume of the heart. To compensate the patients heart rate may have to increase Active hemoptysis: application of positive pressure on the airways can make bleeding worse, so if the patient is already coughing up blood, stop IPPB. Report to the doctor. Suggest SVN to deliver drugs, or IS to expand the chest Conditions that predispose a patient to hemoptysis: Active untreated TB: Tuberculosis is a necrotic infection that can lead to holes in the lung thus bleeding and pneumothorax Lung cancer: cancer can lead to delicate [friable] tissues Cystic fibrosis: air-trapping. Bleeding is common with these kids--- particularly those with blebs on their X-rays Recent surgery to the lung such as a lobectomy, wedge section or a lung reduction Tracheo-esophageal fistula: hole between the esophagus and the tracheal. In a newborn this can be congenital, in an adult it can be the result of trauma to the chest. Air will leave the airway and go into the chest or into the esophagus. Recent esophageal surgery: Because so many folks on IPPB swallow a lot of air this can hamper healing of the esophagus can lead to bleeding Recent facial, oral or skull surgery: see the problems with ICP Singulation: hiccups. This is a spasm of the diaphragm and will trigger breaths so that the patient will get frustrated. [Although this isn't in the literature, my personal experience hints that IPPB triggers hiccups in some folks] Nausea: because of swallowing air, IPPB can rapidly inflate the belly and cause vomiting. Pressures over 20 cmH20 are particularly associated with gastric distension Wheezing: give IPPB with bronchodilator if patient is wheezing or has history. IPPB with normal saline can trigger wheezing 6. List and discuss the hazards of IPPB: Increased RAW in persons who are sensitive to cooling airways Baratrauma: in persons who are getting excessive volumes and pressures or who air trap. The IPPB forces in more air than they can exhale. If they have blebs, these weak spots can burst Nosocomial infection: just as it sends medication deep into the lungs, it sends bacteria deep into the lung. Use filters on the mainline and on the nebulizer driveline. Hyperventilation: because the VT are increased, if the patient breaths fast, he can blow off his C02 and suffer fingers tingling and lightheadedness as intracranial blood vessels constrict. The blood ph becomes alkalotic. Worst case: the increased pH of the blood can trigger cardiac arrhythmias. Respiratory depression in the chronic hypercapnic patient. Because the Air/mix mode has Fi02 of 40-60%, this can depress ventilation in a person with chronic hypercapnia. You can offer the IPPB to the patient with compressed air. Psychological dependence: this can happen to folks with long term lung disease. They might need to be weaned from the IPPB to SVN or one might considered BiPap [maybe they really need extra help all the time] 7. Discuss the assessment of the patient on IPPB. How do we assess for safe effective therapy? Pre-IPPB Assess need for therapy/ expected outcomes determined 1. outcomes should be measurable 2. consider alternative means of hyperinflation such as IS, or SMI or ez-PAP read chart: look for contraindications in history or X-ray report Assess baseline vital signs: 1. HR can increase from the baseline due to the pressure along. If the HR increases and returns to normal within a few minutes, it is pressure not medication increasing the heart…slow down the IPPB and wait more between each breath 2. respiratory rate should decrease after Tx if all is well. If it triggered bronchospasm or baratrauma increased rapid shallow breathing might result. During Tx the patient's retractions should be diminished as WOB has decreased 3. check sensorium. If patient has chronic hypercapnia, this additional Fi02 will cause him to get sleepy & confused. Suggest monitoring the patient with a pulse-ox to watch for Sp02 rising as Pa02 rise. Assess breath sounds & breathing pattern 1. As WOB decreases during the Tx, the patient should respond favorably by decreasing retractions, flaring and other S/S of respiratory distress 2. Hopefully this will persist for a while after the treatment is over 3. measure the return Vt [see below] to make sure the IC is between 15 ml/kg and 45 ml/Kg After 5 minutes: repeat VS to make sure the HR isn’t increased. If it has, wait for a minute or two & recheck. If the HR increased 20 over the baseline give it a few minutes to return to normal. If it does, it is Positive pressure, if it doesn't the tachycardia was due to the medication. Re-check sensorium Recheck the return Vt Post Tx: recheck the return Vt after getting the patient to cough, repeat breath sounds, VS and breathing pattern to assess safety & effectiveness of the therapy 8. How do we measure exhaled volumes using: Wright's Spirometer: place the spirometer on the exhalation valve and read the volume Venti-comp bag: place the bag on the exhalation valve and count the number of breaths it takes to inflate the bag, remove it and read the volume. 9. How do we give an IPPB treatment? a. We give adequate VT [by setting the PIP] The VT is dependent on the PIP the RCP selected and the actual lung compliance or the RAW of the patient lung. We need to give at least 12 ml/kg IBW, but could go higher. Stop well below 45 ml/kg IBW As the PIP is raised at a given lung compliance and RAW, the VT will rise. To decrease the VT we would decrease the PIP. As atelectasis is resolved over a few days, we would hope to see the PIP going down. Always measure the return VT at the exhalation port, by venti-comp bag or by Wrights b. We give adequate flow rate [by setting the flow so that inspiratory time is 1-1.5 seconds long] To decrease the inspiratory time we need to increase the flow rate To increase the inspiratory time, we need to decrease the flow rate If we increase the PIP to increase the VT, sometimes the inspiratory time is too long and we have to increase the flow rate. Remember that really fast flow rates will only cause increased RAW, so keep the inspiratory time between 1-1.5 seconds for adults. Remember that the air mix mode involves air entrainment so the flow rate will be changed by changing the Fi02 c. We give an appropriate rate by having the patient count between IPPB breaths. Remember, this is not ventilation. IPPB is a sustained maximal inspiration just like IS, so we do not need to breathe much faster than 68 bpm. The patient may breathe faster, but he can do so off the IPPB. Rapid RR on the IPPB will increase chances of impeding venous return to the heart, reducing the amount of blood in the heart which would cause the patient to become tachycardiac in order the keep the same cardiac output. d. Rapid RR will encourage air trapping, particularly in persons with increased RAW and wheezing—we need plenty of time to exhalation We need to allow for a 3-5 second inspiratory hold. Remember this is a SMI, that includes a slow deep breath and inspiratory hold to get the gas and the medications deep into the periphery of the lung. The patient can take his mouth off the IPPB mouthpiece to do this breath hold—unless we need to measure the VT. Troubleshooting the machine: If you checked your PIP by watching the monometer while you occlude the patient connector, you will find most problems before attaching the machine to the patient. The pressure should go right to the PIP and stop immediately. The machine should not start just because you jiggle the tube. Is the machine set for appropriate Fi02? Is the sensitivity set for -2? Check the PIP by monometer—not just the number on the dial Is the circuit on nice and tight-do a tactile exam, not just looking at it. If the SVN is set separately, is it set correctly? If you do all of this first, you may not have these problems then you can concentrate on teaching the patient correct technique. problem solution Breath will not come on 1. attach the high pressure line to the gas 2. turn on the flow rate 3. check the sensitivity; set the machine to trigger by itself [auto-cycling] then turn back a bit. 4. does the patient have a tight seal? Mouth closed? Lips tight, nose closed or nose clips? Breath starts too easily 1. sensitivity is set too low. Auto-cycling is when the machine triggers itself just by jiggling the tube. Breath will not end 1. check the flow rate; too slow 2. does the patient have a tight seal? Mouth closed? Lips tight, nose closed or nose clips? 3. check the mushroom valve, the nebulizer line, the nebulizer cup and the mainline for leaks. Inhalation goes on past 1-1.5 seconds 1. flow rate is too slow for this patient 2. check for small leaks that prevent the pressure from rising. Look at the pressure on the monometer, there should be a steady rise in pressure 3. if the pressure is wavering just lower than the PIP, the patient is ‘leading the machine.’ Ask him to relax & let the machine do the work. He is inhaling too fast—also increase the flow rate per his comfort level 4. if you moved from air mix to 100% Fi02, you lost the entrainment so the flow rate needs to be increased again Troubleshoot the patient Never reaches the PIP Reaches the PIP, but breath is a little too quick and the chest did not rise Goes past the PIP Patient gagging with each breath Leak around mouth, nor nose [you did check the machine first right?] Patient inspiratory demand is too fast for the current flow rate—increase it Is the patient sticking tongue into the mouth piece, or closing the glottis? Tell patient to stop blowing back into the machine. Decrease the flow or the PIP for comfort – once they cooperate, increase the settings Angle the mouthpiece off the uvula Replace mouthpiece with mask