23C / 88– Incidence of complicated pneumonia in Belgian children
advertisement

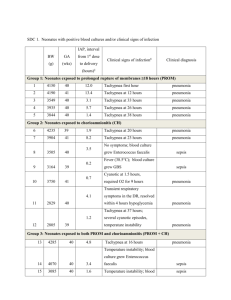
23C / 88– INCIDENCE OF COMPLICATED PNEUMONIA IN BELGIAN CHILDREN AND CLINICAL EVOLUTION UNDER CONSERVATIVE MANAGEMENT. P Van De Wijdeven, B Gijsen, F Vermeulen, K De Boeck, M Proesmans. UZ Gasthuisberg Pediatric Pulmonology – Leuven, Belgium Introduction The incidence and outcome of complicated pneumonia (CP) in our institution were studied In a previous retrospective study from 1993 until 2005. Disease characteristics and treatment modalities were also reported (Van Ackere et al 2009). Aim prospective follow-up of children with CP treated according to a standardized treatment plan. Methods Since may 2006, children admitted with CP in the University Hospital of Leuven, Belgium are registered prospectively and treatment decisions are taken according to a standardized algorithm (Proesmans M et al EJP): antibiotics, chest drain (Seldinger technique) with intrapleural Urokinase® if empyema; surgical treatment if medical treatment fails. CP was defined as at least one of the following 1) loculated effusion on US or CT, 2) analysis of pleural fluid compatible with empyema or 3) need for drain, VATS or thoracotomy. Necrotizing pneumonia was defined as signs of liquefaction and cavitation on chest X ray and/or CT. Results Forty nine patients were registered over a period of 2.5 years. The number of patients treated per year was 19-20 from 1-10-2007 to to 30-09-2009 compared to 11-12/year in the years 2003 to 2005. The median patient age was 3.6 years (IQR 2.7-4.8), 34 male/15 female . Only 4 patients had additional medical problems (2 asthma, 1 VSD and lobectomy, 1 mental retardation) and 34 patient were referred after a median admission of 6 days (IQR 3-8.75). The median duration of fever before first hospital admission was 4 days(IQR 2-6). A causative agent was detected by blood culture in 11/43 sampled patients (all S pneumonia) and in 0/31 by pleural culture. All but 4 patients had been treated with antibiotics before referral. Twenty six of 49 patients were treated with antibiotics only. For 21 patients a chest drain was placed, of which 14 were treated with Urokinase©. VATS was performed in 3 (1 primary, 1 failure of drain, 1 failure of drain +UK) and 3 patients had a thoracotomy (1 primary and 2 after drain +UK). Twelve patients developed a necrotizing pneumonia (2 with lung abscess, 2 with bronchopleural fistula and 6 with pneumatocele), of which only 1 patient underwent a lung resection (segmentectomy). The median hospital stay in our center was 10 days (IQR 5-16) with a total hospital duration of 17 (IQR 13-24). Conclusion Since 2003-2005 the incidence of CP in our center increased further. Following a treatment algorithm with medical treatment as first step, failure rate and need for surgical intervention was low. Even in case of necrotizing pneumonia, prognosis is good; lung resection only had to be performed in 1 patient. Total hospital stay had decreased compared to our previous report.