Pneumonia Workshop
advertisement
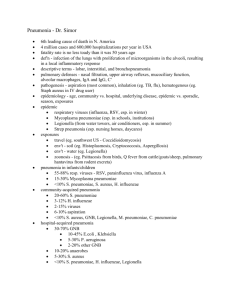
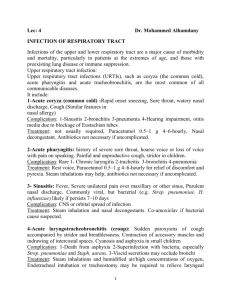
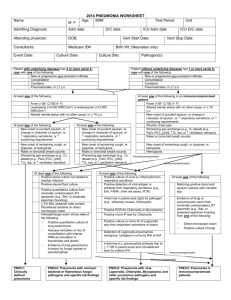
Pneumonia Workshop Bacterial Etiology Streptococcus pneumonia is Gm+ lancet shaped diplocci that can grow in chains. Alpha hemolytic on BAP. Optochin-sensitive. Strict human respiratory pathogen carried in the nasopharynx. Lots of colonization, most common in children or adults around children. Serotype-specific immunity exists, but lots of serotypes. Higher carriage in winter. Disease comes from new serotype exposure. Bacteria grow in edema fluid in alveolar spaces. Erythrocytes accumulate in alveoli, creating a bloody cough. Neutrophils and macrophage then accumulate. Rapid onset, shaking chill, sustained fever, productive bloody cough, chest pain. Typically localized to a single lower lobe. Can also cause otitis media, bacteremia, and meningitis. Pneumolysin is a toxin that autolysis, promoting virulence and induces monocytes to produce TNF, enhancing IS response. Encapsulated bacteria are virulent. Require choline nutritionally. Use choline-binding protein to sequester choline. IgA protease cleases IgA so they can’t bind Ag. Neuraminidase removes sialic acids from host cell surfaces, exposing cells for pneumococcal adherence. Dx. By Gm stain of sputum culture. Culture on BAP for optichin sensitivity and hemolysis. Ag detection is also possible.Tx. with beta-lactam (1st), macrolide (2nd), and vancomycin (3rd). Vaccine contains capsular antigen from common strains. Haemophilus influenzae can cause pneumonia. Often accompanies S. pneumonia. Colonizes respiratory tract. Dx. Culture. Tx. Cephalosporins, macrolides, and fluoroquinolones. Vaccine linked to capsule polysaccharide linked to tetanus toxoid. Mycoplasma pneumonia is prokaryote with no cell wall. Contains sterols, aerobic, fastidious. “Walking pneumonia” is where pathogen attaches to the ciliated respiratory epithelial cells. Mycoplasma matches TLR2 on respiratory epithelial cells and erythrocytes. This stops ciliary action-> desquamate. Leads to immune response. Less than 3 y.o. URTI, 5-20 y.o. LRTI (primary age group infected). Spread is via respiratory droplets. 2-3 wk. incubation period. Most infx. result in disease. Fever, malaise, headache, cough. Sever cough but non-productive. Gm stain negative. PE unremarkable but CXR with interstitial infiltrates. Can present with rash or Raynaud’s when mycoplasma reaches erythrocytes. Dx. Cold agglutinin test. Also IgM and IgG Ab to mycoplasma Ag. Culture of sputum takes 1-2 wks. to grow. Tx. Macrolides preferably. Azithromycin is usually best choice. Psudomonas aeruginosa particulary causes respiratory system infections with cystic fibrosis. Causes ilateral diffuse infiltrates. Uses proteases to survive on thick mucus by killing IgA. Alginate is an adhesion on the capsule that provides a mucoid aspect to colonies. Causes ADP ribosylation of eukaryotic elongation factor 2 by exotoxin A, the same as diphtheria. Very colorful under UV light. Also characteristic fruity odor. Sugar use and hemolysis. Tx. Fluoroquinolones, aminoglycosides, and third generation beta lactams. Rothia mucilaginosa is a major colonizer of oropharynx. Gm+ coccoid, grows in clusters. Very mucoid and sticky. In immunocompromised can cause pneumonia. Klebsiella pneumonia particularly in alcoholics. Capsule is major virulence determinant, polysaccharide, thick and inhibits C3b activity. Dx. Positive chest x-ray, cavities due to necrosis from abscess. Positive blood and sputum cultures, look like “currant jelly.” Short, Gm- rods, nonmotile, lactose fermenting, urease positive. Tx. Extended-spectrum beta-lactams, newer cephalosporins combined with aminoglycosides. Legionella pneumophila Gm- rod. Thin watery secretions in upper airway. (most other pneumonias are thick, purulent). Bronchoalveolar washings show the Gm- sample. Legionella does do thick secretions in lower airway. No known person-to-person. Legionella found in tap water and cooling reservoirs. Inhalation of aerosolized contaminated water. Most at risk are smokers and immunosuppressed. The integrity of the mucociliary escalator is very important. Pneumonia causes serious permanent damage. Pontiac fever comes with a higher attack rate but is milder and self-limiting. Dx. Culture in Buffered Charcoal Yeast Extract. No growth on BAP. Grows inside alveolar macrophages. Extracellular protease causes most of the lung damage. “moth-eaten” lungs with fluid filled patches. Grow in amoeba Hartmanella vermiformis. Must be inhalation of infected amoeba. Modified Gm stain using fuchsin instead of safranin. Urinary Ag test plus sputum culture is best combination. Tx. Macrolide 1st (azithromycin, clarithromycin), fluoroquinolone 2nd (ciprofloxacin, levofloxacin). If not caught early there could be permanent loss of some lung function. Staphylococcus aureus can cause pneumonia b/c of bacteremia. Can cause necrotizing pneumonia via community acquired strains. Can adhere to mucosal cells/nasal epithelial cells via teichoic acid. Viral Etiology SARS Coronavirus ssRNA+. Similar to rhinoviruses except there is usually no fever and coughs and sore throat are rare. Replicates in the lungs and cuases extensive pneumonia. Dx. PCR, ELISA, and viral culture. Only found in URT. No vaccines just Tx. with supportive care. Adenoviruses can lead to LRT pneumonias. Usually benign though. Dx. Immunofluorescence or virus isolation. Linear dsDNA. Influenza (orthomyxoviridae) can cause pneumonia, more on that in the “Influenza workshop”. Influenza usually starts in URT and can spread to the LRT. Causes destruction of cilia and leads to heavy immune response. Respiratory syncytial virus (paramyxoviridae) is a childhood disease targeting children under 2 y.o. Giant multinucleated cells called syncytia form. It is highly contagious and is closely related to Parainfluenza virus. It is spread by aerosol and contact with hands/fomites. Symptoms are similar to rhinovirus with expiratory wheeze normally. Shedding of virus continues for 3 weeks after acute phase. Dx. With syncytia in culture. RSV affects LRT, causing necrotizing bronchiolitis (mediated by the immune response). Peribronchial infiltration results in interstitial pneumonia. Palivizumab is a monoclonal Ab that binds the F proteins and blocks fusion. Male = female (PIV < 5 y.o. men>women). Measles (paramyxoviridae) can be transmitted by aerosol. Characterized by a maculopapular rash that starts on face and spreads to trunk and limbs. High fever and Koplik spots are key indicators. In those with defective immunity, giant cell pneumonia may form. Passive protection can come from immunoglobulin and vaccination comes from the MMR vaccine. Varicella zoster virus (an alpha-herpesvirus): Can cause immune-mediated interstitial pneumonia in adults and can be fatal. Maculopapular rash develops and is more severe in the trunk than in the limbs. Vesicles form from the lesions and then crust over. It enters through the respiratory system. There are vaccines now which are effective. Cytomegalovirus (a beta-herpesvirus) in immunocompromised pts can cause pneumonia. In adults it is sexually transmitted. Histologically shows “owl eye” inclusions. The virus is often latent but can also remain persistent. Tx. With ganciclovir, valganciclovir, cidofovir, and foscarnet to inhibit viral DNA synthesis.